Abstract
There are no previous large scale studies which have evaluated the phenotypes and clinical characteristics of Korean Crohn's disease patients who underwent intestinal resection. The purpose of this multicenter retrospective cohort study was to evaluate the clinical characteristics of Korean Crohn's disease patients who underwent intestinal resection during the study period. A total of 686 patients were enrolled in this study. The study period was over a 20-yr period (1990-2009). The patients were divided into the first-10-yr group and the second-10-yr group. The phenotypes and clinical characteristics were compared between the groups. The most common site of the disease was the ileal area (37.8%) and stricturing behavior was observed in 38.3% patients. The most common type of surgery was segmental resection of the small bowel (30.6%). These phenotypes showed a similar pattern in both the first and second study period groups and did not show any significant differences between the groups. The number of registered patients increased continuously. The phenotypes of Korean Crohn's disease patients who underwent intestinal resection are different compared with previously reported clinical characteristics of general Crohn's disease patients.
Crohn's disease (CD) is a chronic inflammatory disease that involves the entire gastrointestinal tract from the mouth to the anus. Clinical manifestations of CD include diarrhea, abdominal pain, and weight loss; are variable from acute to chronic in nature; and commonly involve growth retardation in children. Intestinal stricture, entero-cutaneous fistula formation, entero-entero, perianal, and intestinal obstruction can be noted, and these are common indications for surgery in CD patients.
Despite the amount of time that has passed since Crohn et al. (1) reported 'regional ileitis' in 1932, the etiopathogenesis of CD is not clear. Environmental factors, abnormal immunologic reaction, and genetic susceptibility have been considered major causes related to the incidence of CD (2).
The incidence rate of CD has been reported to be higher in Western countries than in Asian countries (3). Recently, the incidence rate of inflammatory bowel disease (IBD) has been increasing in Korea and China as lifestyles change to a more Western style (4, 5). This implies that environmental factors are related to the etiology of CD. According to the increasing rate of IBD in Korea, intestinal resection due to CD is an important issue not only for patients with CD but also for medical providers. Thus, evaluation of phenotypes confining to Korean patients with CD who underwent intestinal resection could be valuable and could represent Asian patients with CD who underwent intestinal resection. However, to date, no studies have evaluated the phenotypic characteristics of Korean patients with CD who underwent an intestinal resection. Thus, the aim of this study was to evaluate the phenotypes of patients with CD who underwent intestinal resection and the changing pattern of the indication for surgery and types of surgery in Korea.
A database of the registry of CD patients who underwent intestinal surgery due to CD was established in 2009 by the Inflammatory Bowel Disease Study Group of the Korean Society of Coloproctology. All patients who fulfilled the diagnostic criteria of CD were registered in the database (6, 7).
Seventeen major tertiary university-affiliated hospitals and one colorectal specializing hospital collaborated on this project. Data were collected retrospectively using medical charts from each hospital and then consolidated in a main computer at the Yonsei University College of Medicine. Variables associated with patient demographics and phenotypes of CD in the registry were selected based on the Montreal classification (6).
Data for this study were extracted from this database. A total of 686 patients were registered in the database, and all of these patients were enrolled in this study. Patients had biopsy-proven CD and underwent intestinal resection as treatment for CD. The study period spanned a total of 20 yr. The study period was decided by the first primary intestinal surgery of the enrolled patients for the treatment of CD.
Patient characteristics and phenotypes of CD were evaluated. Patients were divided into the first-10-yr group and the following second-10-yr group. Differences in phenotype and clinical characteristics were evaluated by the process of time by comparing the two groups.
Data were analyzed using the SPSS statistical program (Statistical Product and Service Solution, version 18 for Windows, SPSS Inc., Chicago, IL, USA). Age, disease location, disease behavior, perianal disease, family history, main symptoms and extraintestinal manifestations were categorized according to the Montreal classification (6). These phenotypes were compared between the first and second study periods using the chi-square test. Causes and types of abdominal surgery were also compared between the two periods using the chi-squared test. P values which were less than 0.05 were considered statistically significant.
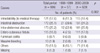
The number of enrolled patients has been increasing continuously (Fig. 1), and the total number of patients who were enrolled in the study was 686. The number of male and female patients was 479 (69.8%) and 207 (30.2%), respectively. The median age was 31 yr (range 5-80 yr). The most common age period was 17-40 yr (76.1%, n = 522). The location of the disease was ileal (37.8%), ileocolic (35.0%), colonic (16.0%) and upper gastrointestinal tract (4.5%). The most common behavior of the disease was the stricturing type (38.3%), and the penetrating type was observed in 30.0% of the patients. Non-stricturing and non-penetrating types were observed in 24.1% of the patients. Perianal disease was noted in 21.0% of the patients. Abdominal pain was the most common main symptom (69.0%). As for the other main symptoms, diarrhea, weight loss, fever and abdominal mass were noted in 18.5%, 5.7%, 1.3%, and 0.9% of the patients, respectively. Besides the main symptoms, other symptoms including anemia, somatitis, erythema nodosum, and arthritis were noted in 2.5%, 0.7%, 0.6%, and 0.4% of the patients, respectively (Table 1). The phenotypes were not different significantly between the first period (1990-2000) and the second period (2001-2009; Table 1).
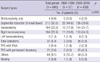
Intestinal obstruction (25.1%) and intra-abdominal abscess (25.2%) were the main causes of abdominal surgery. The percentage of patients who received intestinal resection due to intractability to medical therapy was 17.6%, and 16.8% of the patients received an intestinal resection due to an entero-cutaneous fistula. Fulminant colitis and massive bleeding were the causes of abdominal surgery in 0.7% and 1.9% of the patients, respectively. These causes of abdominal surgery were similar for both time periods (Table 2).
Segmental resection of the small bowel was performed in 30.6% of the patients. Ileocecetomy and right hemicolectomy were each performed in 23.9% of the patients. A total colectomy was performed in 5.4% of the patients. A total proctocolectomy with a permanent ileostomy was performed in 3.6% of the patients, and a total proctocolectomy with an ileal J-pouch anal anastomosis was performed in 0.4% of the patients. Strictureplasty only was performed in 0.6% of the patients. There was no significant difference in surgical procedures between the first and second time period (Table 3).
The most common disease location and the most common disease behavior were the ileal area and the stricturing type, respectively, in the present study cohort. These phenotypes are different from those of CD patients in Western countries. The most common disease location in Western countries is the ileocolic area. Inflammatory disease behavior has been reported as the most common type in both Eastern and Western countries (7-9). Moreover, a study from Korea reported that the most common disease behavior was the inflammatory type, and the most common disease location was the ileocolic area (7). We postulate that the reason why the most common disease behavior was the stricturing type is that the cases in this study are based on patients who underwent surgery for CD. This postulation could be possible considering that the stricturing disease behavior could be one of the main causes of intestinal obstruction. In the subgroup analysis, the stricturing disease behavior was noted in 86.2% (n = 137/n = 159, missing data n = 13) of patients who underwent intestinal surgery due to intestinal obstruction (n = 172).
Environmental factors can be important etiologies if it is considered that the incidence of CD in Asia is increasing (3, 10). Diets and other lifestyle patterns of Asian countries are becoming similar to those in Western countries according to the socioeconomic status of developing Asian countries. These environmental changes could be considered the reason why the incidence of CD in Asia is increasing even though, to date, the incidence rate of CD in Caucasian countries is higher than in Asian countries (3, 10, 11). In the present study, an annual rapidly increasing number of CD patients who were registered because they underwent intestinal resection for treatment of CD in the database showed a similar pattern with that of previous studies (3, 10, 11), and this might imply that environmental factors may play a major role in the etiopathogenesis of Crohn's disease.
In the present study, the phenotypes were not different in the comparison between the first 10 yr and the second 10 yr. Throughout the 20-yr study period, the environmental situation has been changing according to developing socioeconomic status. In the present study, it can be assumed that environmental factors did not influence each of the phenotypes changing in CD patients who underwent intestinal resection even though it might be related to the increasing incidence of CD. Similarly, the types of abdominal operations were not different in the comparison between the first 10 yr and the second 10 yr. This is predictable because the types of operation are usually decided by the disease location or the behavior of the disease, and the disease location and disease behavior were not changed throughout the study period.
Family history of CD is known to be risk factor of the development of CD (12, 13). Family history was noted in 2.3% of the patients in the present study. These results are similar to a previous Japanese study in which the family history was noted in 2.8% of CD patients and a Korean study in which the family history was noted in 1.51% of CD patients (14, 15). The positive rate of family history in CD patients who underwent intestinal resection was similar with the study results where general CD patients were evaluated (14, 15). However, the 2.3% positive family history rate of CD in the present study is relatively quite lower than the positive family history rate of CD in Western countries, in which, the positive family history rate of CD is reported to be from 5% to 18% (12, 15-17).
The numbers of male and female patients were 479 (69.8%) and 207 (30.2%), respectively. Male predominance was noted in the present study. The male and female ratio was 2.3:1, and these results are similar to previous reports from Eastern Countries (10, 18, 19). Meanwhile, in Western countries, there was a 20-30% female predominance observed in CD patients (20, 21). Environmental, ethnic and genetic factors may be the etiologic factors for this difference.
At the time of the operation, a perianal fistula was observed in 21% of the patients. These results are similar to a previous study from Korean and to Western studies (7, 22, 23). However, Ye et al. reported that the cumulative frequency of perianal fistulas was 54.3% after 15 yr from the first diagnosis (7). This was a relatively high incidence compared to the Western studies. In the study performed here, the cumulative frequency of perianal fistulas were not evaluated. The cumulative frequency of perianal fistulas in patients who received intestinal resection due to CD will be evaluated in our next study.
The present study has some limitations. There is a selection bias because the data were collected from 17 major university hospitals and one specialized colorectal hospital. However, the hospitals that participated in this study are spread evenly throughout Korea. Thus, the data in the present study can represent the phenotypes of Korean CD patients who underwent intestinal resection even though these data have a basic selection bias. Nevertheless, large scale cohort studies are necessary to confirm the results of this study and investigate the detailed characteristic phenotypes of Korean CD patients who underwent intestinal resection compared to total CD patients or CD patients who do not undergo intestinal resection.
The CD patients who were only being treated medically were excluded because the registry was built by investigators who are gastrointestinal surgeons. Thus, our results cannot be generalized to the whole CD patient population. However, the results of the present study show the specific phenotypes of CD patients confined to CD patients who underwent intestinal resection. Thus, the results of this study might have an important value since surgical treatment is a major concern to patients and their caregivers.
The annual registered number of CD patients who underwent intestinal resection has been increasing since 1990. The ileal area and the stricturing type are the most common disease location and disease behavior, respectively, in this study population. These phenotypic characteristics are different from those of the general CD patients, and did not change during the 20-yr study period.
Figures and Tables
ACKNOWLEDGMENTS
The authors thank the members of the Korean IBD study group for their help in data acquisition and MiSun Park for the English revision. The authors have no conflicts of interest in this study.
References
1. Crohn BB, Ginzburg L, Oppenheimer GD. Regional ileitis: a pathological and clinical entity. JAMA. 1932. 99:1323–1329.
2. Lees CW, Satsangi J. Genetics of inflammatory bowel disease: implications for disease pathogenesis and natural history. Expert Rev Gastroenterol Hepatol. 2009. 3:513–534.
3. Yang SK, Loftus EV Jr, Sandborn WJ. Epidemiology of inflammatory bowel disease in Asia. Inflamm Bowel Dis. 2001. 7:260–270.
4. Zheng JJ, Zhu XS, Huangfu Z, Shi XH, Guo ZR. Prevalence and incidence rates of Crohn's disease in mainland China: a meta-analysis of 55 years of research. J Dig Dis. 2010. 11:161–166.
5. Yang SK, Hong WS, Min YI, Kim HY, Yoo JY, Rhee PL, Rhee JC, Chang DK, Song IS, Jung SA, et al. Incidence and prevalence of ulcerative colitis in the Songpa-Kangdong District, Seoul, Korea, 1986-1997. J Gastroenterol Hepatol. 2000. 15:1037–1042.
6. Satsangi J, Silverberg MS, Vermeire S, Colombel JF. The Montreal classification of inflammatory bowel disease: controversies, consensus, and implications. Gut. 2006. 55:749–753.
7. Ye BD, Yang SK, Cho YK, Park SH, Yang DH, Yoon SM, Kim KJ, Byeon JS, Myung SJ, Yu CS, et al. Clinical features and long-term prognosis of Crohn's disease in Korea. Scand J Gastroenterol. 2010. 45:1178–1185.
8. Romberg-Camps MJ, Dagnelie PC, Kester AD, Hesselink-van de Kruijs MA, Cilissen M, Engels LG, Van Deursen C, Hameeteman WH, Wolters FL, Russel MG, et al. Influence of phenotype at diagnosis and of other potential prognostic factors on the course of inflammatory bowel disease. Am J Gastroenterol. 2009. 104:371–383.
9. Song XM, Gao X, Li MZ, Chen ZH, Chen SC, Hu PJ, He YL, Zhan WH, Chen MH. Clinical features and risk factors for primary surgery in 205 patients with Crohn's disease: analysis of a South China cohort. Dis Colon Rectum. 2011. 54:1147–1154.
10. Yao T, Matsui T, Hiwatashi N. Crohn's disease in Japan: diagnostic criteria and epidemiology. Dis Colon Rectum. 2000. 43:S85–S93.
11. Yang SK, Yun S, Kim JH, Park JY, Kim HY, Kim YH, Chang DK, Kim JS, Song IS, Park JB, et al. Epidemiology of inflammatory bowel disease in the Songpa-Kangdong district, Seoul, Korea, 1986-2005: a KASID Study. Inflamm Bowel Dis. 2008. 14:542–549.
12. Peeters M, Nevens H, Baert F, Hiele M, de Meyer AM, Vlietinck R, Rutgeerts P. Familial aggregation in Crohn's disease: increased age-adjusted risk and concordance in clinical characteristics. Gastroenterology. 1996. 111:597–603.
13. Binder V, Orholm M. Familial occurrence and inheritance studies in inflammatory bowel disease. Neth J Med. 1996. 48:53–56.
14. Yoshida Y, Murata Y. Inflammatory bowel disease in Japan: studies of epidemiology and etiopathogenesis. Med Clin North Am. 1990. 74:67–90.
15. Park JB, Yang SK, Byeon JS, Park ER, Moon G, Myung SJ, Park WK, Yoon SG, Kim HS, Lee JG, et al. Familial occurrence of inflammatory bowel disease in Korea. Inflamm Bowel Dis. 2006. 12:1146–1151.
16. Yang H, McElree C, Roth MP, Shanahan F, Targan SR, Rotter JI. Familial empirical risks for inflammatory bowel disease: differences between Jews and non-Jews. Gut. 1993. 34:517–524.
17. Orholm M, Munkholm P, Langholz E, Nielsen OH, Sørensen TI, Binder V. Familial occurrence of inflammatory bowel disease. N Engl J Med. 1991. 324:84–88.
18. Song IS, Chang DK, Kim CY. Current status of Crohn's disease in Korea. Korean J Med. 1998. 55:158–168.
19. Wang YF, Zhang H, Ouyang Q. Clinical manifestations of inflammatory bowel disease: East and West differences. J Dig Dis. 2007. 8:121–127.
20. Bernstein CN, Blanchard JF, Rawsthorne P, Wajda A. Epidemiology of Crohn's disease and ulcerative colitis in a central Canadian province: a population-based study. Am J Epidemiol. 1999. 149:916–924.
21. Lashner BA. Epidemiology of inflammatory bowel disease. Gastroenterol Clin North Am. 1995. 24:467–474.
22. American Gastroenterological Association Clinical Practice Committee. American Gastroenterological Association medical position statement: perianal Crohn's disease. Gastroenterology. 2003. 125:1503–1507.
23. Yoon YS, Yu CS, Yang SK, Yoon SN, Lim SB, Kim JC. Intra-abdominal fistulas in surgically treated Crohn's disease patients. World J Surg. 2010. 34:1924–1929.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download