Abstract
Nowadays, infectious aortitis has become a rare disease thanks to antibiotics, but remains life-threatening. We present a case of a patient with acupuncture-induced infectious aortitis leading to aortic dissection. Chest computed-tomogram scan revealed Stanford type A dissection with pericardial effusion. Under the impression of an impending rupture, emergent surgery was performed. During surgery, infectious aortitis was identified incidentally, so she underwent resection of the infected aorta including surrounding tissues. Then the ascending aorta and hemi-arch were replaced with a prosthetic graft as an in situ fashion. The resected tissue and blood cultures revealed Staphylococcus aureus, so prolonged antibiotherapy was prescribed.
Acupuncture has been used widely in many Asian countries for thousands of years to control various diseases and symptoms, and it has recently become globalized. Although it has documented safety and efficacy, several serious complications have been reported (1, 2). In this report, we describe a rare case of infectious aortitis leading to aortic dissection resulting from acupuncture, and a literature review.
An 83-yr-old woman with history of hypertension was admitted emergently with fever, chill, and chest pain for 2 weeks on 8 July 2012. She had been treated with acupuncture on her back and buttock because of chronic back pain before the onset of symptoms. Blood pressure was 80/50 mmHg, heart rate was 94 beats per minute, and body temperature was 38.2℃. Other vital signs were unremarkable. White blood cell count was 27,420/µL with 90% neutrophils and C-reactive protein was 14.78 mg/dL on laboratory examination. Blood and urine culture was done to investigate the focus of fever. Because she complaint of chest pain and mediastinal widening on an initial chest x-ray was documented, chest computed tomogram (CT) was performed to rule out acute aortic syndromes. And it revealed a dissection of the ascending aorta with hemopericardium and an incidentally noted abscess in the right buttock (Fig. 1). Transthoracic echocardiography revealed severely dilated ascending aorta with intimal flap suggestive of aortic dissection, a moderate amount of pericardial effusion without tamponade sign, and no visible vegetations. The left and right ventricular functions were preserved and the cardiac valves had no abnormal findings except mild aortic valve regurgitation. Under the impression of acute aortic dissection with an impending rupture, an emergent operation was performed.
The surgery was performed through a median sternotomy and a subclavicular incision. After pericardiotomy, blood with fresh clots was observed and removed securely. On the superior wall of the proximal aortic arch just distal to the innominate artery and beneath the innominate vein, inflamed friable tissue with a hematoma was observed and cultured microbiologically. Cardiopulmonary bypass (CPB) was started and systemic cooling was instituted with arterial cannulation in the right axillary artery and venous cannulation in the right atrium.
During removal of the infected adventitial tissue and sharp dissection of the arch and the ascending aorta, the aorta suddenly ruptured. By careful management of the patient's vital signs, the ruptured aorta was firmly compressed and she was cooled continuously. Left ventricular vent was placed through the right superior pulmonary vein. Upon cardiac fibrillation, a cross-clamp was placed and the aorta was opened by a transverse incision, which revealed circular dissection that reached just above the sinotubular junction leaving the coronary ostia unaffected. Then cardioplegia was antegrade infused into the coronary opening.
Upon reaching the core temperature to 20℃, CPB was discontinued and a cross-clamp was off. The ascending aorta was opened by vertical incision, which was extended from the previous transverse aortic incision upward to the proximal aortic arch. Antegrade cerebral perfusion of about 10 mL/kg/min was initiated through the arch vessels and adjusted to maintain cerebral perfusion pressures of 60 mmHg.
During selective cerebral perfusion, the infected friable aortic walls and dissecting aneurysm were completely removed and debrided. After false lumen obliteration, distal aortic reconstruction of hemi-arch replacement was performed with an open anastomosis technique using a one-branched graft (InterGard®, Maquet, France). Distal aortic anastomosis was then complete and an additional arterial cannula was inserted into a side-branch of the graft. After vigorous de-airing maneuvers, flow to the head vessels and lower body was resumed and simultaneously rewarming was initiated. Proximal aortic anastomosis was performed at the level of the sinotubular junction during the rewarming period.
The patient was easily weaned off bypass, and transesophageal echocardiography showed no abnormal findings.
Histopathological examination from the ascending aorta, obtained during the operation, showed aortitis without giants cells and caseous necrosis. Cultures from the aortic necrotic materials and blood returned positive for methicillin-sensitive Staphylococcus aureus, for which she received intravenous cefazolin for 6 weeks. And oral Rifampin 600 mg a day was prescribed for 2 weeks after the end of intravenous antibiotic treatment. After surgery, follow-up blood cultures were performed two times a week. In next week, blood cultures were converted to negative. During the antibiotic treatment, biochemical parameters of inflammation were slowly improved and normalized. Additionally the right buttock abscess was progressively improved and subsided without a surgical drainage on physical examination. After 11 days of ICU treatment because of acute renal failure and 46 days of hospitalization, she was discharged. She remains asymptomatic 2 months later without signs of recurrence, and postoperative follow-up chest CT that was performed after 4 weeks revealed the patent bypass grafts (Fig. 2).
Infectious aortitis is a rare but life-threatening condition, and most commonly affects the abdominal aorta (3, 4). Infection of the aorta can arise by several mechanisms. Similar to endocardium, aortic intima is generally highly resistant to infection, but disrupted intima becomes vulnerable to infection. Thus, bacteremic seeding of an existing intimal injury or atherosclerotic plaque may lead to aortitis. Additionally, normal or atherosclerotic vessels can become involved, resulting from septic emboli of the aortic vasa vasorum, contiguous infective focus extending to the aorta wall, and direct bacterial inoculation at the time of trauma, such as a penetrating injury (5).
Various microorganisms have been associated with infectious aortitis, most commonly Staphylococcus, Enterococcus, Streptococcus, and Salmonella species (6).
Clinical manifestations are often nonspecific and have a broad spectrum, depending upon the site of infection and its localized impact and characteristics, frequently causing delays in diagnosis. However, rapid diagnosis is extremely important, because this condition has high mortality and morbidity (7, 8). Computed tomography (CT) is widely available and allows a rapid exclusion of other aortic pathologies that may mimic acute aortitis. Furthermore, CT findings of periaortic density and adjacent gas collection suggest an impending rupture, even if no aneurysm is present (5, 9). Echocardiogram, magnetic resonance angiography, and positron emission tomography are also useful (5, 6). However, neither of these methods led to the correct finding in a case of a patient with aortitis of the ascending aorta. When image studies show signs of potential aortic rupture, prompt management is mandatory since the mortality of ruptured infectious aortitis has been reported to be as high as 90% (10).
Optimal management for infectious aortitis requires complete surgical excision and reconstruction of the infected aorta combined with prolonged antibiotic administration. Antibiotics with broad antimicrobial coverage should be initiated as soon as the diagnosis of infectious aortitis is suspected, and while awaiting microbiologic data. The antibiotic regimen can then be tailored, based upon the results of culture and sensitivity data. While no clinical studies have established the optimal duration of antibiotic therapy for aortitis, a treatment course of at least 6 to 12 weeks after surgical debridement and clearance of blood cultures is generally recommended (5, 6). Some authors even recommend life-long oral antibiotics following the intravenous course, especially for microorganisms difficult to treat or after in situ prosthetic bypass (7).
The goal of surgery is to control probable rupture, confirm the diagnosis, remove septic foci, and reconstruct the arterial vasculature (8). For revascularization, prosthetic grafts may be placed in situ or in an extra-anatomic fashion. The best method for revascularization remains controversial. There is special concern over whether the type of reconstruction might contribute to an increased risk of graft-related complications. Theoretically, in situ reconstruction may lead to a higher rate of early graft infection, and extra-anatomic bypass may be impractical, especially when aortic branches are involved, and a lower long-term patency rate may necessitate further aortic reconstruction. However, there have been many reports on the efficacy, safety, and durability of in situ prosthetic graft, with very low rates of early graft infection and mortality (4, 7). Therefore, in situ prosthetic graft reconstruction is currently the preferred method of revascularization (5, 7).
This case is of interest for several reasons. First, the illness was induced by acupuncture. We believe that the pre-existing atherosclerotic aorta was contaminated by systemic bacteremia caused by acupuncture, leading to infectious aortitis. However, it is uncertain whether the abscess in the right buttock was a consequence of systemic seeding from aortitis or a focus of continuous bacteremia leading to aortitis. In our opinion, the latter is more reasonable because of previous acupuncture history before the onset of symptoms and no other seeding site from aortitis. The second interesting points are the anatomic location and the type of acute aortic syndromes induced by aortitis. The thoracic aorta is a less-frequent site (about 30%) than the abdominal aorta for the formation of spontaneous mycotic aneurysm (3, 4). Some reports have been dealt with aortitis involving the descending thoracic aorta, but infectious aneurysm on the ascending aorta seems to be extremely rare (11-13). With regards to a type of acute aortic syndromes, many reports have noted that infectious aortitis causes aneurysmal formation or rupture usually. Our case involved the ascending aorta and presented not an aneurysmal formation but acute aortic dissection caused by aortitis, which is extremely rare according to a MEDLINE search and literature review. Additionally, acute Stanford type A dissection combined with aortitis caused by acupuncture has not been reported previously.
In conclusion, infectious aortitis can have an aggressive presentation and a complicated early outcome. Thus clinicians must be aware of this rare, but serious pathology, and that it may present in patients with an existing intimal injury or atherosclerotic plaque. Once the diagnosis is established or suspected, early and complete surgical excision of the infected aorta in combination with prolonged antibiotics (extended for at least 6-12 weeks) is of critical importance.
Figures and Tables
Fig. 1
Enhanced chest CT scans with axial (A) and coronal images (B) show the dissection flap of the ascending aorta with pericardial effusion and wall thickening of the proximal aortic arch, which may be suggested a soft tissue infection or hematoma. Mediastinal fluid collection and bilateral pleural effusion are also noted. (C) Abscess on the right buttock (white arrow) was found incidentally at CT scans.
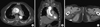
Fig. 2
Pre-operative (A) and post-operative (B) three-dimensional volume rendering of contrast-enhanced CT scans. (A) Preoperative CT scans show Stanford type A aortic dissection with the enlarged ascending aorta and that the proximal aortic arch was aneurysmal and atherosclerous changes. During surgery, infectious aortitis was identified incidentally at the proximal aortic arch (arrowhead). (B) Postoperative chest CT scans revealed that the ascending aorta and hemiarch were replaced with a prosthetic graft (asterisk) and patent. Also proximal and distal anastomotic lines (arrow) were visible.

References
1. Lao L, Hamilton GR, Fu J, Berman BM. Is acupuncture safe? a systematic review of case reports. Altern Ther Health Med. 2003. 9:72–83.
2. Lee S, Lim SH, Kim DK, Joo HC. Acupuncture induced necrotizing aortitis with infected pseudoaneurysm formation. Yonsei Med J. 2008. 49:322–324.
3. Long R, Guzman R, Greenberg H, Safneck J, Hershfield E. Tuberculous mycotic aneurysm of the aorta: review of published medical and surgical experience. Chest. 1999. 115:522–531.
4. Oderich GS, Panneton JM, Bower TC, Cherry KJ Jr, Rowland CM, Noel AA, Hallett JW Jr, Gloviczki P. Infected aortic aneurysms: aggressive presentation, complicated early outcome, but durable results. J Vasc Surg. 2001. 34:900–908.
5. Lopes RJ, Almeida J, Dias PJ, Pinho P, Maciel MJ. Infectious thoracic aortitis: a literature review. Clin Cardiol. 2009. 32:488–490.
6. Gornik HL, Creager MA. Aortitis. Circulation. 2008. 117:3039–3051.
7. Ting AC, Cheng SW, Ho P, Poon JT, Tsu JH. Surgical treatment of infected aneurysms and pseudoaneurysms of the thoracic and abdominal aorta. Am J Surg. 2005. 189:150–154.
8. Foote EA, Postier RG, Greenfield RA, Bronze MS. Infectious aortitis. Curr Treat Options Cardiovasc Med. 2005. 7:89–97.
9. Malouf JF, Chandrasekaran K, Orszulak TA. Mycotic aneurysms of the thoracic aorta: a diagnostic challenge. Am J Med. 2003. 115:489–496.
10. Bronze MS, Shirwany A, Corbett C, Schaberg DR. Infectious aortitis: an uncommon manifestation of infection with Streptococcus pneumoniae. Am J Med. 1999. 107:627–630.
11. Maillet JM, Palombi T, Sablayrolles JL, Bonnet N. Septic rupture of an atherosclerotic plaque of the ascending aorta. Interact Cardiovasc Thorac Surg. 2012. 15:790–791.
12. Bedeleanu D, Coman C, Encica S, Hagiu R, Molnar A, Cãpâlneanu R. Stanford type A aortic dissection in a hypertensive patient with atherosclerosis of aorta and aortitis. Echocardiography. 2000. 17:181–185.
13. Choi JB, Yang HW, Oh SK, Yun KJ. Rupture of ascending aorta secondary to tuberculous aortitis. Ann Thorac Surg. 2003. 75:1965–1967.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download