Abstract
The aim of this study is to compare clinical outcomes for seven years, between sirolimus-eluting stent (SES) and bare metal stent (BMS). During the BMS and drug-eluting stent (DES) transition period (from April 2002 to April 2004), 434 consecutive patients with 482 lesions underwent percutaneous coronary intervention, using BMS or SES. Using propensity score matching, 186 patients with BMS and 166 patients with SES were selected. Seven year clinical outcomes of major adverse cardiac events (MACE), such as cardiac death, myocardial infarction (MI) and ischemia-driven target vessel revascularization (TVR), and angiographic definite stent thrombosis (ST) were compared. At one-year follow up, patients with SES showed significantly lower MACE (9.1% in BMS vs 3.0% in SES, P = 0.024). However, cumulative MACE for 7 yr was not significantly different between two groups (24.7% in BMS vs 17.4% in SES, P = 0.155). There was no significant difference in MI, TVR, death and ST. The TVR were gradually increased from 1 to 7 yr in SES, on the contrary to that of BMS. In conclusion, although SES showed better clinical outcomes in the early period after implantation, it did not show significant benefits in the long-term follow up, compared with that of BMS.
First-generation drug-eluting stent (DES), such as sirolimus-eluting stent (SES), have reduced in-stent restenosis (ISR), compared with that of bare-metal stent (BMS) in a broad spectrum of patients and lesion subsets (1). However, the therapeutic benefits are most pronounced, during the first-year, which was driven by the strong suppression of neo-intimal hyperplasia (2). Recently, a late catch-up phenomenon was observed by the increasing incidence of late target lesion revascularization (TLR), after SES implantation (3). Otherwise, BMS has shown different healing process, in which neointimal hyperplasia was peaking at 6-9 months after procedures and regressing thereafter (4). In the present study, we have evaluated the short and the long term clinical outcomes of patients with stents implanted in transition period from BMS to DES.
A total of 434 consecutive patients, with 482 lesions, underwent percutaneous coronary intervention (PCI), using BMS or SES (Cypher, Cordis, Miami Lakes, FL, USA), during the transition period from BMS to DES (April 2002 to April 2004) in the interventional cardiology registry database of Yeungnam Unversity Medical Center, Daegu, Korea were enrolled. Among them, 352 patients, with 388 lesions (BMS, 186; SES, 166), were selected with propensity score matching analysis.
PCI was performed using standard techniques. All patients received 325 mg aspirin orally, and a loading dose of 300 mg of clopidogrel before coronary angiography (CAG). For the emergency cases, 300 mg loading dose of clopidogrel was initiated before CAG, or after PCI for the patients with poor condition. After PCI, the patients were routinely treated with aspirin 100 mg/day, clopidogrel 75 mg/day and/or cilostazol 200 mg/day at the operator's discretion. The patients were advised to maintain life-long aspirin therapy. The duration of taking clopidogrel was at the operator's discretion, which depended on the complexity of the lesion and procedure.
Study outcomes were a composite of major adverse cardiac events (MACE), including cardiac death, myocardial infarction (MI), target lesion revascularization (TLR), ischemia-driven target vessel revascularization (TVR) and definite stent thrombosis (ST) for 7 yr. MI was defined as typical ischemic chest pain and/or ST-segment, and/or T-wave abnormalities with an increased creatine kinase-MB level ≥ 2 times the reference values, without any new pathologic Q waves. TLR was defined as either surgical or percutaneous re-intervention driven by significant (> 50%) luminal diameter narrowing within the stent or the 5 mm borders proximal and distal to the stent and that was undertaken in the presence of either anginal symptoms or objective evidence of ischemia. Ischemia-driven TVR was defined as emergency or elective coronary artery bypass grafting or repeat PCI in the target vessel for chest pain or a positive test result for ischemia (exercise stress test, stress echocardiogram, 24-hr Holter monitoring, evidence of ST segment depression or increase in > 1 lead on electrocardiogram at rest, or radionuclide study showing a reversible defect). Stent thrombosis (ST) was defined as previously described by the Academic Research Consortium (5). Death was defined as cardiac mortality; the mortality from proven non-cardiac origin was excluded. Cumulative rates of event-free survival and MACE were analyzed over 7 yr follow-up period. The Follow-up clinical information was obtained from medical records of outpatient clinic, medical insurance record and/or direct telephone contact. The death records and causes were obtained from the data supported by Statistics Korea.
The results are expressed as the means ± SDs or numbers (%). Comparisons of categorical variables were done, using the chi-square test. Student's t-test was used to compare the continuous variables. MACE-free survival distributions were estimated, according to the Kaplan-Meier methods. The log-rank test was used to compare MACE-free survival between the two groups. A P value < 0.05 was considered statistically significant. Propensity scores were made for the BMS and SES group, based on patient and lesion characteristics. The following variables were used to calculate the propensity score: age, sex, diabetes mellitus, hypertension, smoking, dyslipidemia, left ventricular ejection fraction, diagnosis, disease vessel, lesion location, type of lesion, bifurcation lesion, ostial lesion, chronic total occlusion lesion, stent diameter, and stent length. Data was analyzed using the SPSS 12.0 software for Windows (SPSS, Chicago, IL, USA).
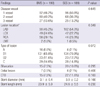
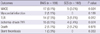
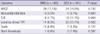
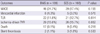
The baseline characteristics between the two groups are similar (Table 1). Substantial patients with acute myocardial infarction were enrolled (40.4% in BMS vs 28.9% in SES, P = 0.083) in this study. Medical therapy including aspirin, statin and beta-blocker between two groups also were not statistically different. Angiographic and procedural findings were shown in Table 2. There were no differences in the disease vessel number and the lesion location. Most lesions are type B1 (65.8% in BMS vs 70.9% in SES, P = 0.072). The patients with chronic total occlusion lesion was 7.5% in BMS and 11.6% in SES (P = 0.169). Stent diameter was 3.1 ± 0.4 mm in BMS and 3.0 ± 0.2 mm in SES (P = 0.166). Stent length was 23.9 ± 5.9 in BMS and 24.6 ± 5.5 in SES (P = 0.230). Cumulative one year outcomes are shown in Table 3. The rate of TLR was higher in BMS than that of SES (7.5% in BMS vs 1.8% in SES, P = 0.012). The rate of ischemia-driven TVR was higher in BMS than that of SES (8.1% in BMS vs 2.4% in SES, P = 0.024). However, the rates of MI and cardiac deaths were not different (Table 3). Cumulative MACE was higher in BMS, compared to those in SES (9.1% in BMS vs 3.0% in SES, P = 0.024). Clinical outcomes in 1 to 7 yr are represented in Table 4. The rate of MACE between the two groups were not different (17.1% in BMS vs 14.9% in SES, P = 0.740). The rate of TLR (4.7% in BMS vs 11.1% in SES, P = 0.064) and TVR (8.3% in BMS vs 13.7% in SES, P = 0.082) have a higher trend to SES than that of BMS. Death, MI and stent thrombosis were not different between the two groups in those years. Cumulative seven-year MACE was presented in Table 5 and showed no difference between the two groups (24.7% in BMS vs 17.4% in SES, P = 0.155), during the 7 yr follow-up. Further, the rate of TLR (11.8% in BMS vs 12.7% in SES, P = 0.814) and ischemia-driven TVR (15.6% in BMS vs 15.7% in SES, P = 0.862) were not different for 7 yr. Incidence of all cause death was 16.4% (58 of 352 patients). The rates of MI, deaths and stent thrombosis were not different for 7 yr. Kaplan-Meier cumulative event curves for patients treated with BMS or SES was presented in Fig. 1. It showed total MACEs were not different, during the 7 yr after stent implantation. During the first year, the rate of MACE of BMS was higher than that of SES. However, the rate of MACE was not different at the end of the 7-yr follow-up period. These findings are shown again in the ischemia-driven TVR in Fig. 2. During the 1 yr follow-up, the results of SES were superior to BMS, but the beneficial effects were reduced as time went by.
The main findings of this study are that SES showed better clinical outcomes in the early period after implantation, however, it did not show significant benefits in the long-term follow-up, compared with that of BMS. Furthermore, stent thrombosis and adverse cardiac events, in terms of the rate of MI and death, were not different between BMS and SES. However, the rate of TVR was higher in SES for the first year, but the rate of TVR was continuously increased during the 7-yr follow-up, despite that of BMS was retarded from 1 yr after the stent implantation.
The "late catch-up" phenomenon refers to slow, but persistent increase of neo-intimal hyperplasia during the long-term period. The main mechanism of ISR after BMS was neointimal hyperplasia, which has been reported to show a lumen loss in the first 6 months and with lumen enlargement from 6 months to 3 yr (4, 6). Therefore, TLR, beyond 1 yr after BMS implantation, had been reported to be uncommon. Compared with BMS, DES has different components, including stent platform, active pharmacologic compound and drug carrier. From these compositions, DES also has dramatically reduced ISR by inhibition of neointimal hyperplasia for the early period after implantation. In an animal study, late neo-intimal growth was developed within SES compared with BMS and inflammation and delayed cellular proliferation were possible causes of late neointimal growth (7). Furthermore, long-term inflammation has been reported after SES implantation by pathological observation in humans (8). Sustained inflammation by drug polymer might cause continuous vessel wall injury and could be another possible cause of the late TLR increase. Despite concerns regarding the possibilities that a delayed vascular healing and chronic inflammation, after SES implantation, is associated with the delayed neointimal growth, long-term efficacy of SES in transition period from BMS to DES has not yet been evaluated in the real-world practice. Caixeta et al. reported 5-yr clinical outcomes after SES implantation (9). During the follow-up period, TVR was reduced nearly 2-fold in the SES versus the BMS group, mainly due to remarkably lower rates of TLR during the first year, and it is unlikely that the use of SES is associated with a late catch-up phenomenon. Further, some reported that late catch-up by imaging was not connected with clinical late catch-up (10, 11). However, Shiode et al. (12) showed that from 6 months to 3 yr, stenosis of BMS-treated lesions regressed, but stenosis of SES-treated lesions progressed. Park et al. (13) also showed that late catch up occurred in both paclitaxel-eluting stents and SES with greater delayed late loss in SES. Recently published five-year clinical and angiographic outcomes of a randomized comparison of SES and paclitaxel-eluting stent also showed the continuous increase in the late lumen loss in conjunction with the ongoing risk of very late stent thrombosis, which suggests that vascular healing remains incomplete, up to 5 yr after implantation of the first-generation DES (2). These studies demonstrate that even though current absolute differences of minimal lumen diameter, diameter stenosis are small, these differences can become larger over time. Our study compared long-term clinical outcomes, between BMS to DES in the transition period. Although the rates of myocardial infarction and cardiac deaths are not different, the rate of ischemia-driven TVR was significantly higher in BMS, compared with that in SES in the first year. However, the rate of ischemia-driven TVR of SES continuously increased, despite no substantial rise of that of BMS, and the benefits, during the first years, were lost over time, towards the 7 yr period. From our study, a late catch-up could exist and ischemia-driven TVR continuously increased over time in the first-generation DES, especially SES, and these findings might have an influence on the adverse cardiac events in the future with a longer period of the follow-up study. Furthermore, our results also might seem to be the clinical reflection of main mechanism of the delayed vascular healing and persistent inflammation of the first-generation SES.
Our study conducted further evaluation of independent risk factors for MACE by multivariate analysis. Variables includes old age over 70 yr, history of diabetes mellitus (DM), presence of multivessel disease over 2 vessels, history of statin therapy, and usage of stent (DES and BMS). From these, DM was only independent risk factor for MACE (P = 0.047; OR, 1.4; 95% C.I. 0.86-2.2).
This study has several limitations. First, the number of enrolled patients was small enough to fully assess the clinical outcomes from a single center. Second, this study focused on the clinical outcomes, and we could not give accurate information about angiographic quantitative coronary analysis. However, our data showed that lesion characteristics such as disease vessel number, lesion location and type of lesion, which had trend but showed no statistical differences, and procedural findings such as stent diameter were not different between two groups. Third, this study was retrospective in its design, and selection bias may be present. So we conducted propensity match analysis to minimize the chance of selection bias. Fourth, our results could imply that SES and DES had no differences of clinical usage in patients with coronary artery disease and one could think that both stents (DES or BMS) would be equally useful in daily clinical practice. However, DES used in this study was 1st generation SES, which was released at over 10 yr ago and now 2nd or 3rd generation DES were released. The number of patients was small and large number of patients could show better results. Fifth, our results showed that cumulative MACE for 7 yr was not significantly different (24.7% in BMS vs 17.4% in SES, P = 0.155). However, there were quite numerical differences because of limitations such as small number of enrolled patients. So it could represent different results if conditions were changed. Sixth, there were some trends of increased death in BMS compared with DES in spite of no statistical differences (9.1% in BMS vs 5.4% in DES, P = 0.218). This seemed to be higher age, which also showed no differences in baseline characteristics, in BMS than in DES (68±9 in BMS vs 66±10 in DES, P = 0.085).
In conclusion, although SES showed better clinical outcomes in the early period after implantation, it did not show significant benefits in the long-term follow-up, compared with that of BMS. Therefore, longer term of clinical data is needed to assess the longevity of good clinical outcomes, which have been shown in the early period.
Figures and Tables
Fig. 1
Kaplan-Meier curves for major adverse cardiac events (MACE) during each time periods. Panel A shows no differences in MACE for 7 yr between two groups (P = 0.344). However, the rate of MACE was higher in bare-metal stent (BMS) than Sirolimus-eluting stent (SES) for 1 yr after stent implantation (Panel B, P = 0.026). After 1 yr, the rate of MACE was similar between two groups (Panel C, P = 0.754).

Fig. 2
Kaplan-Meier curves for ischemia-driven target vessel revascularization (TVR) during each time periods. Panel A shows no difference in TVR between bare-metal stent (BMS) and Sirolimus-eluting stent (SES, P = 0.710). However, there are significant differences during 1 yr after stent implantation (8% in BMS vs 2% in SES, P = 0.020, Panel B). After 1 yr, the rate of TVR was not different between two groups (Panel C, P = 0.144).

Table 1
Baseline characteristics

BMS, bare-metal stent; SES, Sirolimus-eluting stent; PCI, percutaneous coronary intervention; CVA, cerebrovascular accident; LVEF, left ventricular ejection fraction; STEMI, ST-segment elevation myocardial infarction; NSTEMI, non-ST-segment elevation myocardial infarction; ACE, angiotensin converting enzyme; ARB, angiotensin receptor blocker.
References
1. Morice MC, Serruys PW, Sousa JE, Fajadet J, Ban Hayashi E, Perin M, Colombo A, Schuler G, Barragan P, Guagliumi G, et al. A randomized comparison of a sirolimus-eluting stent with a standard stent for coronary revascularization. N Engl J Med. 2002. 346:1773–1780.
2. Räber L, Wohlwend L, Wigger M, Togni M, Wandel S, Wenaweser P, Cook S, Moschovitis A, Vogel R, Kalesan B, et al. Five-year clinical and angiographic outcomes of a randomized comparison of sirolimus-eluting and paclitaxel-eluting stents: results of the Sirolimus-Eluting Versus Paclitaxel-Eluting Stents for Coronary Revascularization LATE trial. Circulation. 2011. 123:2819–2828.
3. Nakagawa Y, Kimura T, Morimoto T, Nomura M, Saku K, Haruta S, Muramatsu T, Nobuyoshi M, Kadota K, Fujita H, et al. Incidence and risk factors of late target lesion revascularization after sirolimus-eluting stent implantation (3-year follow-up of the j-Cypher Registry). Am J Cardiol. 2010. 106:329–336.
4. Kimura T, Abe K, Shizuta S, Odashiro K, Yoshida Y, Sakai K, Kaitani K, Inoue K, Nakagawa Y, Yokoi H, et al. Long-term clinical and angiographic follow-up after coronary stent placement in native coronary arteries. Circulation. 2002. 105:2986–2991.
5. Cutlip DE, Windecker S, Mehran R, Boam A, Cohen DJ, van Es GA, Steg PG, Morel MA, Mauri L, Vranckx P, et al. Clinical end points in coronary stent trials: a case for standardized definitions. Circulation. 2007. 115:2344–2351.
6. Kimura T, Yokoi H, Nakagawa Y, Tamura T, Kaburagi S, Sawada Y, Sato Y, Yokoi H, Hamasaki N, Nosaka H, et al. Three-year follow-up after implantation of metallic coronary-artery stents. N Engl J Med. 1996. 334:561–566.
7. Carter AJ, Aggarwal M, Kopia GA, Tio F, Tsao PS, Kolata R, Yeung AC, Llanos G, Dooley J, Falotico R. Long-term effects of polymer-based, slow-release, sirolimus-eluting stents in a porcine coronary model. Cardiovasc Res. 2004. 63:617–624.
8. Virmani R, Guagliumi G, Farb A, Musumeci G, Grieco N, Motta T, Mihalcsik L, Tespili M, Valsecchi O, Kolodgie FD. Localized hypersensitivity and late coronary thrombosis secondary to a sirolimus-eluting stent: should we be cautious? Circulation. 2004. 109:701–705.
9. Caixeta A, Leon MB, Lansky AJ, Nikolsky E, Aoki J, Moses JW, Schofer J, Morice MC, Schampaert E, Kirtane AJ, et al. 5-year clinical outcomes after sirolimus-eluting stent implantation insights from a patient-level pooled analysis of 4 randomized trials comparing sirolimus-eluting stents with bare-metal stents. J Am Coll Cardiol. 2009. 54:894–902.
10. Pocock SJ, Lansky AJ, Mehran R, Popma JJ, Fahy MP, Na Y, Dangas G, Moses JW, Pucelikova T, Kandzari DE, et al. Angiographic surrogate end points in drug-eluting stent trials: a systematic evaluation based on individual patient data from 11 randomized, controlled trials. J Am Coll Cardiol. 2008. 51:23–32.
11. Byrne RA, Kastrati A, Kufner S, Massberg S, Birkmeier KA, Laugwitz KL, Schulz S, Pache J, Fusaro M, Seyfarth M, et al. Randomized, non-inferiority trial of three limus agent-eluting stents with different polymer coatings: the Intracoronary Stenting and Angiographic Results: Test Efficacy of 3 Limus-Eluting Stents (ISAR-TEST-4) Trial. Eur Heart J. 2009. 30:2441–2449.
12. Shiode N, Shirota K, Tsunoda F, Kato Y, Fujiwara M, Mimura A. Late progression after sirolimus-eluting stent implantation for de novo lesions: comparison with bare metal stent implantation. Circ J. 2010. 74:1104–1110.
13. Park KW, Kim CH, Lee HY, Kang HJ, Koo BK, Oh BH, Park YB, Kim HS. Does late catch-up exist in drug-eluting stents: insights from a serial quantitative coronary angiography analysis of sirolimus versus paclitaxel-eluting stents. Am Heart J. 2010. 159:446–453.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download