Abstract
After an episode of acute bleeding from esophageal varices, patients are at a high risk for recurrent bleeding and death. However, there are few reports regarding the long-term results of secondary prophylaxis using endoscopic variceal ligation (EVL) against variceal rebleeding in pediatrics. Thirty-seven, who were followed for over 3 yr post-eradication, were included in the study. The mean duration of follow up after esophageal variceal eradication was 6.4±1.9 yr. The mean time required to achieve the eradication of varices was 3.25 months. The mean number of sessions and O-bands needed to eradicate varices was 1.9±1.2 and 3.8±1.5, respectively. During the period before the first EVL treatment, 145 episodes of bleedings developed in 37 children. Over the 3 yr of follow-up after variceal eradication, only 4 episodes of rebleeding developed in 4 of 37 patients. The four rebleeding episodes consisted of an esophageal variceal bleed, a gastric variceal bleed, a duodenal ulcer bleed, and a bleed caused by hemorrhagic gastritis. There was no mortality during long-term follow up after variceal eradication. During long-term follow up after esophageal variceal eradication using solely EVL in children with esophageal variceal bleeds, rebleeding episodes and recurrence of esophageal varices were rare. EVL is a safe and highly effective method for the long-term prophylaxis of variceal rebleeding in children with portal hypertension.
Gastroesophageal variceal hemorrhage is the most serious life threatening complication of portal hypertension. In the pediatric population, many underlying diseases cause portal hypertension and esophageal variceal bleeding (1-4). These diseases can be classified into intrahepatic and extrahepatic diseases. Biliary atresia is the most common cause of liver cirrhosis in children. Patients with biliary atresia should undergo a Kasai operation as soon as possible after diagnosis. Of patients with biliary atresia, half of patients will die or require liver transplantation within 6 yr following Kasai operation if the patient first presented with esophageal variceal bleedings (5).
Treatments for esophageal variceal bleedings include pharmacologic, endoscopic and surgical therapies. Endoscopic variceal ligation (EVL) with pharmacologic treatment, including nonselective β-blockers and/or mononitrate isosorbide, is recommended as the treatment of choice to prevent episodes of rebleeding in adults with esophageal varices (6-11).
Although EVL is the most well-studied treatment approach for children with esophageal variceal bleeding (12-14), there are few reports about long-term results of the use of EVL for prevention of variceal rebleeding episodes (12, 15). We focused on analyzing the long-term effects of EVL to prevent variceal rebleeding episodes or the recurrence of varices during a follow-up period of more than 3 yr post-eradication, especially for high-risk esophageal varices.
Sixty eight children were admitted to Seoul National University Children's Hospital over a 10-yr period due to esophageal variceal bleeding caused by various intra- and extrahepatic diseases. A total of 324 sessions of endoscopic variceal ligation (EVL) were performed to treat variceal bleeding or to prevent rebleeding from esophageal varices in the 68 patients.
Out of the 68 children, 37 were seen for follow-up over a period longer than 3 yr after variceal eradication. These 37 children were included in the study. The mean age at the first EVL was 8.7±4.3 yr (mean±2SD). The study group included 24 male children and 13 female children. The mean duration of follow up after esophageal variceal eradication was 6.4±1.9 yr.
Somatostatin was administered in most patients and blood transfusion was occasionally performed. When patients were hemodynamically stable, the first EVL was performed and the following EVLs were scheduled. Using an endoscope and Stiegmann-Goff endoscopic ligator, all variceal ligations were performed under the general anesthesia. Overtube was not utilized for any patients.
We retrospectively gathered clinical information, endoscopic findings and the results of variceal ligation. Endoscopic severity of esophageal varices was graded either I, II or III (16). Grade I varices are flattened by air insufflation. Grade II varices are not flattened by air insufflation and are separated by areas of healthy mucosa. Grade III varices are confluent and not flattened by insufflations. Other findings associated with a high risk of gastrointestinal bleeding were noted, including the presence of red wale markings on the esophageal mucosa and portal hypertensive gastropathy.
Esophageal varices were defined as eradicated if they were reduced in size to Grade I or were not apparent upon endoscopic examination after EVL. Rebleeding episodes were defined as bleeds that developed after eradication of esophageal varices. Recurrence of varices was defined as varices that newly developed after eradication of esophageal varices. Both the treatment effect of EVL for acute esophageal variceal bleeding and rebleeding rate after variceal eradication were analyzed (17, 18).
This study was reviewed and approved by the institutional review board of Seoul National University Hospital (IRB No. 1307-095-505). We received written informed consent from the parents of all participating children.
The data were analyzed using the SPSS 18.0 software program (SPSS Inc., Chicago, IL, USA). The difference between EVL procedure configurations for intra- and extrahepatic disease was compared using Student's t-test. A paired t-test was used to analyze the efficacy of secondary prophylaxis with EVL, examining the difference between findings before the first EVL and after eradication of esophageal varices.
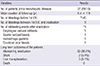
The underlying diseases of 37 patients was classified into intra- (n=19) and extrahepatic (n=18) diseases. Biliary atresia (n=14) and portal vein thrombosis (n=16) were the most common causes of intra- and extraheptic diseases, respectively (Table 1). At the time of first EVL, there were no patients with grade I esophageal varices, 15 patients with grade II and 22 patients with grade III. To attain eradication of esophageal varices, the mean numbers of EVL sessions and of O-bands per session required were 1.9±1.2 and 3.8±1.5 , respectively. The mean interbanding interval to eradication was 1.2 months between sessions. Red wale markings and portal hypertensive gastropathy were detected on the first EVL in 23 (62%) and 23 (62%) patients, respectively. Gastric varices were noted during the first EVL treatment in 9 patients (24%).
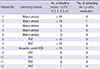
The efficacy of secondary prophylaxis with EVL was analyzed (Table 2). The mean duration of follow-up after eradication was 6.4±1.9 yr. Before the first EVL, 145 bleeding episodes occurred in 37 children. However, after eradication of esophageal varices, only 4 episodes of rebleeding occurred in 4 out of 37 patients (P=0.000). The four rebleeding episodes included an esophageal variceal bleed, a gastric variceal bleed, one episode of hemorrhagic gastritis and a duodenal ulcer bleed. There was no significant difference in the frequency of rebleeding episodes between patients with intra- or extrahepatic disease. Only one (2.7%) of 37 patients presented with recurrent esophageal varices after eradication.
A few patients presented with minor chest pain or abdominal discomfort immediately after EVL. EVL-related bleedings were rare and minor. With regards to the long-term prognosis of the study patients, 31 patients (83.8%) maintained eradication status (Table 2). Two patients with portal vein thrombosis (5.4%) had distal splenorenal shunts due to gastric varices and pancytopenia, respectively. Three patients (8.1%), consisting of 2 patients with biliary atresia and 1 with Wilson's disease, underwent liver transplantation due to disease progression of liver cirrhosis. No deaths occurred.
We also identified a prominent decrease in the frequency of bleeding before and after variceal eradication in 12 children who each had more than 5 bleeding episodes prior to the first EVL treatment (Table 3).
We analyzed the long-term results and the efficacy of secondary prophylaxis in children with high-risk esophageal varices. The mean duration of follow up after esophageal variceal eradication was 6.4±1.9 yr. Our study included many patients with high-risk esophageal varices, including 23 out of 37 patients (62%) noted to have red wale markings at the initial endoscopy. For the 37 pediatric patients in the study, a total of 145 episodes of esophageal variceal bleedings was noted before the first EVL treatments, reduced to 4 rebleeding episodes after eradication. Recurrence of esophageal varices occurred in 1 out of 37 children. We also identified a prominent decrease in the frequency of bleeding before and after variceal eradication in 12 children who each had more than 5 bleeding episodes prior to the first EVL treatment.
There are few reports regarding the effect of secondary prophylaxis for long-term periods after eradication (12, 15). Duche et al. (15) reported the efficacy of EVL to prevent rebleeding episodes, but the mean duration of follow-up was 28 months (range 1-128). In their study, rebleeding episodes after eradication developed in 2 out of 22 patients. Dos Santos et al. (12) reported a high rate of rebleeding episodes (27.8%) and a high rate of recurrence of esophageal varices (44.4%) in the EVL-alone group, over an average follow-up period of 4.2 yr after eradication.
We performed EVLs at a mean interval of 1.2 months. The initial sessions were spaced more closely (monthly) and once control of bleeding had been achieved were given more infrequently (every 3-6 months) until the varices were eradicated. Although many authors had recommended performing EVL treatments every 1-3 week (19-22), Harewood et al. (23) revealed the interval was significantly shorter in the rebleeding group (2 weeks; interquartile range 0-2 weeks) than in the non-rebleeding group (5 weeks; interquartile range 3-7 weeks) of adult patients with esophageal varices.
We did not use pharmacologic treatments, such as propranolol, nadolol and mononitrate isosorbide, for secondary prophylaxis. According to adult guidelines (9, 10, 24, 25), EVLs with nonselective β-blockers and/or mononitrate isosorbide is recommended as the first choice for secondary prophylaxis in adults with esophageal variceal bleeding. In contrast to adults, children with variceal bleeding have poorer outcomes after EVL with pharmacologic treatment when compared to EVL alone (12). Propranolol prophylaxis avoids the risk of endoscopic treatment. However, the risks of variceal bleeding and mortality increase when propranolol is discontinued (26). In children, propranolol is not recommended for routine use at this time because of insufficient data on its safety and efficacy (27).
Over long-term follow-up of the study patients, there were no deaths. Two (5.4%) and 3 (8.1%) patients underwent distal splenorenal shunt and liver transplantation, respectively. Dos Santos et al. (12) and Duche et al. (15) reported a mortality rate of 9% during long-term follow-up after eradication of esophageal varices in children with esophageal variceal bleeding.
In conclusion, over long-term follow up after esophageal variceal eradication using EVL alone in children with esophageal variceal bleeds, rebleeding episodes and recurrence of esophageal varices were rare. EVL is a safe and highly effective method for the long-term prophylaxis of variceal rebleeding in children with portal hypertension.
Figures and Tables
References
1. Kim SY, Seo JK. Esophageal varix in children: endoscopic evaluation and clinical characteristics. J Korean Pediatr Soc. 1993; 36:1691–1700.
2. Hill ID, Bowie MD. Endoscopic sclerotherapy for control of bleeding varices in children. Am J Gastroenterol. 1991; 86:472–476.
3. Goenka AS, Dasilva MS, Cleghorn GJ, Patrick MK, Shepherd RW. Therapeutic upper gastrointestinal endoscopy in children: an audit of 443 procedures and literature review. J Gastroenterol Hepatol. 1993; 8:44–51.
4. Price MR, Sartorelli KH, Karrer FM, Narkewicz MR, Sokol RJ, Lilly JR. Management of esophageal varices in children by endoscopic variceal ligation. J Pediatr Surg. 1996; 31:1056–1059.
5. Miga D, Sokol RJ, Mackenzie T, Narkewicz MR, Smith D, Karrer FM. Survival after first esophageal variceal hemorrhage in patients with biliary atresia. J Pediatr. 2001; 139:291–296.
6. Sharara AI, Rockey DC. Gastroesophageal variceal hemorrhage. N Engl J Med. 2001; 345:669–681.
7. Laine L, Cook D. Endoscopic ligation compared with sclerotherapy for treatment of esophageal variceal bleeding: a meta-analysis. Ann Intern Med. 1995; 123:280–287.
8. Rubenstein JH, Eisen GM, Inadomi JM. A cost-utility analysis of secondary prophylaxis for variceal hemorrhage. Am J Gastroenterol. 2004; 99:1274–1288.
9. Kravetz D. Prevention of recurrent esophageal variceal hemorrhage: review and current recommendations. J Clin Gastroenterol. 2007; 41:S318–S322.
10. Sarin SK, Wadhawan M, Agarwal SR, Tyagi P, Sharma BC. Endoscopic variceal ligation plus propranolol versus endoscopic variceal ligation alone in primary prophylaxis of variceal bleeding. Am J Gastroenterol. 2005; 100:797–804.
11. De la Peña J, Brullet E, Sanchez-Hernández E, Rivero M, Vergara M, Martin-Lorente JL, Garcia Suárez C. Variceal ligation plus nadolol compared with ligation for prophylaxis of variceal rebleeding: a multicenter trial. Hepatology. 2005; 41:572–578.
12. Dos Santos JM, Ferreira AR, Fagundes ED, Ferreira AP, Ferreira LS, Magalhães MC, Bittencourt PF, Carvalho SD, Figueiredo Filho PP, Penna FJ. Endoscopic and pharmacological secondary prophylaxis in children and adolescents with esophageal varices. J Pediatr Gastroenterol Nutr. 2013; 56:93–98.
13. Molleston JP. Variceal bleeding in children. J Pediatr Gastroenterol Nutr. 2003; 37:538–545.
14. Augustin S, Altamirano J, González A, Dot J, Abu-Suboh M, Armengol JR, Azpiroz F, Esteban R, Guardia J, Genescà J. Effectiveness of combined pharmacologic and ligation therapy in high-risk patients with acute esophageal variceal bleeding. Am J Gastroenterol. 2011; 106:1787–1795.
15. Duché M, Ducot B, Ackermann O, Baujard C, Chevret L, Frank-Soltysiak M, Jacquemin E, Bernard O. Experience with endoscopic management of high-risk gastroesophageal varices, with and without bleeding, in children with biliary atresia. Gastroenterology. 2013; 145:801–807.
16. Lykavieris P, Gauthier F, Hadchouel P, Duche M, Bernard O. Risk of gastrointestinal bleeding during adolescence and early adulthood in children with portal vein obstruction. J Pediatr. 2000; 136:805–808.
17. De Franchis R. Baveno V Faculty. Revising consensus in portal hypertension: report of the Baveno V consensus workshop on methodology of diagnosis and therapy in portal hypertension. J Hepatol. 2010; 53:762–768.
18. Shneider B, Emre S, Groszmann R, Karani J, McKiernan P, Sarin S, Shashidhar H, Squires R, Superina R, de Ville de Goyet J, et al. Expert pediatric opinion on the Report of the Baveno IV consensus workshop on methodology of diagnosis and therapy in portal hypertension. Pediatr Transplant. 2006; 10:893–907.
19. Garcia-Tsao G. Current management of the complications of cirrhosis and portal hypertension: variceal hemorrhage, ascites, and spontaneous bacterial peritonitis. Gastroenterology. 2001; 120:726–748.
20. Lo GH, Chen WC, Chen MH, Hsu PI, Lin CK, Tsai WL, Lai KH. Banding ligation versus nadolol and isosorbide mononitrate for the prevention of esophageal variceal rebleeding. Gastroenterology. 2002; 123:728–734.
21. Patch D, Sabin CA, Goulis J, Gerunda G, Greenslade L, Merkel C, Burroughs AK. A randomized, controlled trial of medical therapy versus endoscopic ligation for the prevention of variceal rebleeding in patients with cirrhosis. Gastroenterology. 2002; 123:1013–1019.
22. Villanueva C, Miñana J, Ortiz J, Gallego A, Soriano G, Torras X, Sáinz S, Boadas J, Cussó X, Guarner C, et al. Endoscopic ligation compared with combined treatment with nadolol and isosorbide mononitrate to prevent recurrent variceal bleeding. N Engl J Med. 2001; 345:647–655.
23. Harewood GC, Baron TH, Song LM. Factors predicting success of endoscopic variceal ligation for secondary prophylaxis of esophageal variceal bleeding. J Gastroenterol Hepatol. 2006; 21:237–241.
24. Jalan R, Hayes PC. UK guidelines on the management of variceal haemorrhage in cirrhotic patients: British Society of Gastroenterology. Gut. 2000; 46:III1–III15.
25. Gawrieh S, Saeian K. Management of esophageal varices: an update from Digestive Disease Week and American Association for the Study of Liver Diseases 2003. Curr Gastroenterol Rep. 2004; 6:206–209.
26. Abraczinskas DR, Ookubo R, Grace ND, Groszmann RJ, Bosch J, Garcia-Tsao G, Richardson CR, Matloff DS, Rodés J, Conn HO. Propranolol for the prevention of first esophageal variceal hemorrhage: a lifetime commitment? Hepatology. 2001; 34:1096–1102.
27. Schreiber RA. Propranolol and portal hypertension: should kids be on the block? J Pediatr Gastroenterol Nutr. 1999; 29:10–11.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download