Abstract
Several lines of evidence indicate that prehypertension is more atherogenic than normal blood pressure. Serum γ-glutamyltransferase (GGT) is known to be positively associated with prehypertensive status and the progression of hypertension. However, there have been no prospective studies of serum GGT level as a predictor of prehypertension. Apparently 13,435 healthy men (mean age 42.0 ± 6.6 yr) with normal blood pressure were included in a prospective cohort study in 2005 and were followed up to 2010 with the endpoint being incident of prehypertension. During the follow up period (median 2.80 ± 1.44 yr; actual follow-up 37,679.1 person-year), prehypertension was developed in 7,867 (58.6%) participants. Risk estimations for incident prehypertension were analyzed based on quartiles of serum GGT levels using multivariate adjusted Cox proportional hazards model. In unadjusted model, the hazard ratio for incident prehypertension for the highest 3 quartiles of baseline serum GGT level was 1.21 (1.13-1.29), 1.29 (1.21-1.38), and 1.57 (1.47-1.67) compared the lowest quartile of serum GGT level, respectively (P for trend < 0.001). These associations still remained statistically significant, even after adjusting for multiple covariates. These findings indicate that increased serum GGT level is independently associated with incident prehypertension in Korean men.
Serum γ-glutamyltransferase (GGT), a plasma membrane-bound enzyme, has been used as a biological marker for alcohol intake or liver cell damage (1-3). However, recent studies have shown that serum GGT might be related to oxidative stress and might have a role in the pathogenesis of cardiovascular disease, diabetes mellitus, strokes and metabolic syndrome (4-6).
In the seventh Joint national committee (JNC-7), National Heart, Lung, and Blood Institute (NHLBI) of United States presented a new diagnostic classification for blood pressure (BP) where systolic BP (SBP) is between 120-139 mmHg or diastolic BP (DBP) is between 80-89 mmHg, previously categorized as normotensive and borderline BP in the JNC-6, is now categorized as prehypertension. This is based on the study results that the risk of cerebral infarction and coronary artery disease increases in patients with SBP/DBP above 115/75 mmHg, and the risk is doubled as BP increases by 20/10 mmHg (7). In Strong Heart Study, the incidence rate of hypertension within 4 yr in prehypertensive group was 38%, and in Framingham Heart-Study, the risk of hypertension was doubled in prehypertensive group compared with normotensive group (8, 9). Additionally, the risk of cardiovascular disease in prehypertensive group has 1.8 times higher than that of normotensive group (10).
Recent cross-sectional studies have reported the association between serum GGT and hypertension and prehypertension prevalence (11-15). However, there was no prospective cohort study on the association between serum GGT and incident prehypertension. In this study, we examined the clinical association between baseline serum GGT level and incident prehypertension in Korean men.
The present study was a prospective cohort study to examine the association between serum GGT level and incident prehypertension in Korean men participating in a medical health check-up program at the Total Healthcare Center of Kangbuk Samsung Hospital, Sungkyunkwan University, Seoul, Korea. We included in the present study only men who were normotensive at baseline. Initially, participants who had abnormal blood pressure and participants with prehypertension and hypertension were excluded from this study. In 2005, 46,728 men who had participated in a medical health check-up program were recruited in this study. Among the 46,728 participants, 29,233 men were excluded due to the following reasons: 238 had a history of a malignancy; 323 had a history of cardiovascular disease; 3,241 were receiving antidyslipidemic medications; 19,793 and 9,591 had a baseline prehypertension and hypertension. Because some participants had more than one exclusion criteria, the total number of men who were eligible for the study was 17,495. We further excluded 4,060 participants who did not attend any follow-up visit between 2006 and 2010. Accordingly, 13,435 participants were included in the final analysis and were observed for incident prehypertension. The total follow-up period was 37,679.1 person-year and average follow-up period was 2.80 ± 1.44 person-years.
Study data included a medical history, a physical examination, information provided by a questionnaire, anthropometric measurements and laboratory measurements. The medical history was assessed by the examining physicians. All the participants were asked about health-related behavior including alcohol intake, cigarette smoking and physical activity. Questions about alcohol intake included the frequency of alcohol intake per week and the usual amount of alcohol intake per day. We considered participants as current smoker who reported to smoke at that time of the study. In addition, the participants were asked about the frequency of physical activity, such as jogging, bicycling, and swimming that lasted long enough to produce perspiration (≥ 1 time/week). Body mass index (BMI) was calculated as the weight (kilograms) divided by height (meters) squared.
After a 5-min rest, BP was measured on the right upper arm in the sitting position using a standardized mercury sphygmomanometer. SBP and DBP were recorded as the first and fifth Korotkoff phases, respectively. According to the JNC-7 guidelines, the measured BP was classified as normal (SBP < 120 mmHg and a DBP < 80 mmHg), prehypertension (SBP 120 to 139 mmHg or DBP 80 to 90 mmHg) and hypertension (SBP ≥ 140 mmHg or DBP ≥ 90 mmHg, or current use of medication for hypertension). Diabetes mellitus was defined as fasting serum glucose more than 126 mg/dL, or current use of medication for diabetes.
After fasting for at least 12 hr, peripheral venous samples were collected. Total cholesterol, triglyceride, low-density lipoprotein (LDL) cholesterol, high-density lipoprotein (HDL) cholesterol, creatinine, high-sensitivity C-reactive protein (hs-CRP), fasting blood glucose, insulin, aspartate aminotransferase (AST), alanine aminotransferase (ALT), and GGT were measured. Serum GGT was measured using Bayer Reagent Packs (Bayer HealthCare, Tarrytown, NY, USA) on an automated chemistry analyzer (ADVIA 1650 Autoanalyzer; Bayer Diagnostics, Leverkusen, Germany). Insulin levels were measured with immunoradiometric assays (Biosource, Nivelles, Belgium). Insulin resistance was calculated with the homeostasis model assessment of insulin resistance (HOMA-IR): fasting serum insulin (µU/mL) × FBG (mg/dL)/22.5 (16). The clinical laboratory has been accredited and participates annually in inspections and surveys by the Korean Association of Quality Assurance for Clinical Laboratories.
Data in the text and tables were expressed as the mean ± standard deviation (SD) or medians (interquartile range) for continuous variables and percentages of the number for categorical variables. Participants were divided into quartiles on the basis of serum GGT level as follows: quartile 1, GGT < 17 IU/L; quartile 2, GGT 17 to 25 IU/L; quartile 3, 25 to 40 IU/L GGT; and quartile 4, GGT ≥ 40 IU/L. The one-way ANOVA and chi-square-test were used to analyze the statistical differences among the characteristics of the participants at the baseline visit according to the quartile groups of serum GGT level. The distributions of continuous variables were evaluated, and log transformations were used in the analysis as required. For cases with incident prehypertension, the time spent at incident prehypertension was assumed to be the midpoint between the baseline visit and the visit at which prehypertension was first diagnosed. The person years were calculated as the sum of follow-up times from the baseline until the assumed time prehypertension was diagnosed or until the final examination of each individual. Compared to the lowest quartile of serum GGT, the hazards ratios (HRs) of the highest 3 quartiles of serum GGT was calculated by the Cox proportional hazard model after adjustment for baseline characteristics such as age, log (hsCRP), total cholesterol, creatinine, recent smoking status, alcohol intake, regular exercise and diabetes mellitus. For the linear trends of risk, the number of quartiles was used as a continuous variable and tested on each model. To use the Cox proportional hazards models, we checked the validity of the proportional hazards assumption. Two approaches were used to assess the validity of the proportional hazards assumption. First, the assumption was assessed by log-minus-log-survival function and found to graphically hold. Second, to confirm the validity of the proportional hazards assumption, time-dependent covariate analysis was used. The time-dependent covariate was not statistically significant, suggesting that the proportional hazards assumption is not violated (P = 0.055). P values less than 0.05 were considered to be statistically significant. Statistical analyses were performed PASW Statistics 18 (SPSS Inc., Chicago, IL, USA).
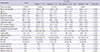
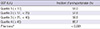
The demographic and biochemical characteristics of the study participants according to the quartile groups of serum GGT level are presented in Table 1. During 37,679.1 person-years of follow-up, 7,867 (58.6%) cases of prehypertension were diagnosed between 2006 and 2010. At the baseline visit, the mean age and BMI of study participants were 42.0 ± 6.6 yr and 23.6 ± 2.6 kg/m2, respectively. There were significant linear trends across the quartiles of serum GGT level with respect to all of the listed variables. Age, BMI, SBP, DBP, total cholesterol, triglyceride, LDL-cholesterol, fasting blood glucose, insulin, HOMA-IR, hsCRP, AST and ALT tended to increased as the serum GGT quartile increased. The percentages of current smoker, alcohol intake participant and diabetes mellitus have a tendency to increase along with the increase of the serum GGT quartile. However, HDL-cholesterol and the percentages of regular exercise participants tended to decrease along with the increase in the serum GGT quartile, respectively. Table 2 shows the incident prehypertension have a tendency to increase according to the quartile groups of serum GGT level.
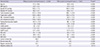
The baseline characteristics of participants with or without incident prehypertension are shown in Table 3. Participants who were diagnosed prehypertension during the follow-up period had higher serum GGT level at baseline compared with those who did not develop prehypertension. In contrast to participants without incident prehypertension, those with incident prehypertension were slightly older (42.6 vs 41.2 yr) and more likely to have a less favorable metabolic profiles at baseline. As expected, all clinical variables showed statistically significant differences between two groups except for recent smoking status.
Table 4 presented the results of Cox proportional HRs and 95% confidence interval (CI) for prehypertension according to the quartile groups of serum GGT levels. In unadjusted model, the HRs and 95% CI for incident prehypertension for the highest 3 quartiles of baseline serum GGT level 1.21 (95% CI, 1.13-1.29), 1.29 (95% CI, 1.21-1.38) and 1.57 (95% CI, 1.47-1.67) compared to the lowest quartile of serum GGT, respectively (P for trend < 0.001). The age adjusted HRs was 1.19 (95% CI, 1.12-1.27), 1.26 (95% CI, 1.18-1.34) and 1.51 (95% CI, 1.42-1.61) compared to the lowest quartile of serum GGT, respectively (P for trend < 0.001). These associations still maintained statistically significant, even after further adjustments for explanatory variables (age, total cholesterol, log [hsCRP], creatinine, recent smoking status, alcohol intake, regular exercise and diabetes mellitus) in model 1 and 2. In model 1, the adjusted HRs (95% CI) for incident of prehypertension were 1.21 (1.12-1.30), 1.23 (1.13-1.32) and 1.48 (1.37-1.60), respectively (P for trend < 0.001). In model 2, the adjusted HRs (95% CI) for incident prehypertension were 1.19 (1.11-1.29), 1.21 (1.12-1.31) and 1.44 (1.33-1.56), respectively (P for trend < 0.001).
Serum GGT level was found to be positively associated with the incident prehypertension in Korean men, free of baseline prehypertension, hypertension and many other diseases. The HR of prehypertension was increased with in a dose-dependent manner by increasing quartiles of serum GGT. Theses association persisted after adjusting for age, total cholesterol, log (hsCRP), creatinine, current smoking status, alcohol intake, regular exercise, and diabetes mellitus.
In our study, 17,495 eligible male participants were selected because of sex differences in serum GGT level. Serum GGT was significantly higher in men compared to women due to the greater consumption of alcohol and higher prevalence of liver disease in men (17). Another reason was the difference in distribution of excess fat in men and women. Serum GGT in women with BMI above 32 kg/m2 was comparable to the serum GGT in men with BMI in the range of 20-24 kg/m2 (18, 19).
To the best of our knowledge, our study was the first prospective cohort study demonstrating a positive association between baseline serum GGT level and incident prehypertension; therefore we were unable to compare our results with those of others. Only several previous cross-sectional studies showed that serum GGT is associated with prevalence of prehypertension. Higher serum GGT levels were associated with prehypertension in nationally representative sample of the US adults, with the multivariate odds ratio (OR) (95% CI) of 1.84 (1.37-2.46) comparing quartile 4 of serum GGT (> 29 U/L) to quartile 1 (< 13 U/L). Their results were consistent in subgroup analyses of race-ethnicity, age, smoking, alcohol intake, BMI, waist circumference and diabetes (13). Similar results were found in a community-based cross-sectional study from Japan and Turkey. The multivariate OR (95% CI) for prehypertension was 1.73 (1.06-3.18) for the middle tertile (29-53 IU/L) and 2.37 (1.31-4.31) for the highest tertile (> 53 IU/L), compared to the lowest tertile of serum GGT (< 29 IU/L) in Japanese men (14). And the mean serum GGT level was higher in the prehypertension group than in the control group (24.33 and 18.85 U/L, respectively; P < 0.001) in Turkish men and women (15). These findings were consistent with previous reports related to hypertension (16, 20). However, we further suggest that serum GGT level is also related to incident prehypertension, a stage with higher risk of progressing to hypertension. Therefore, if people who have higher serum GGT level change their life-style with the healthy behavior such as a combination of increased physical activity, moderation in alcohol intake, and consumption of a diet that is lower in sodium content and higher in fruit, vegetables, and low-fat dairy products, then risk of progressing to hypertension will be decreased (21, 22). Prehypertension was one of the main contributors to hypertension, and possibly to the future development of cardiovascular disease, although there were differences in the progression rate prehypertension to hypertension (9, 23). Thus, we consistently suggest that higher serum GGT level within physiologically normal range may be useful to predict the risk of prehypertension.
GGT is an enzyme expressed in serum and most cell surfaces; however the function of GGT on these cells is uncertain. Emerging evidence has been shown that serum GGT might be an important enzyme in the pathogenesis of cardiovascular diseases. However, the mechanisms by which the serum GGT level increases the risk of prehypertension are not fully understood. In our study, the serum GGT predicted the incident prehypertension independently of the alcohol intake. Therefore, the association between serum GGT and prehypertension is not mediated by alcohol intake. Several lines of recent evidence suggest that an association between serum GGT and incident prehypertension is plausible. First, serum GGT has been interpreted as a reliable marker of oxidative stress (3, 6). Serum GGT has a critical role in the maintenance of intracellular defense mechanism by initiating extracellular catabolism of glutathione, the main antioxidant in mammalian cells (1, 2, 24). These associations suggest that GGT may be a marker of oxidative stress. Oxidative stress caused increase of BP by direct vasoconstriction and sodium retention in the vascular smooth muscle and endothelial cells (3). Second, insulin resistance could play a major role in the association between serum GGT and incident prehypertension, because GGT might be interpreted as a marker for hepatic steatosis and hepatic insulin resistance (3, 5). More recent studies suggest that leptin may stimulate sympathetic outflow from the hypothalamus which will increase the heart rate and BP (25). In this study, HOMA-IR increased in dose-response manner with increasing quartiles of serum GGT. Serum GGT might be a reliable predictor of diabetes and hypertension, even within a physiologically normal range in the CARDIA study (6). Third, serum GGT activity probably reflected chronic inflammation associated with low levels of anti-inflammatory hormones or cytokines. Serum GGT was strongly associated with C-reactive protein, the widely recognized marker of chronic inflammation (5, 26). These results strongly suggest that GGT is involved in the pathway of inflammation. However to clarify the mechanisms of prehypertension, further interventional studies that target serum GGT are needed.
Several limitations of this study must be considered. First, participants were self-selected and approximately 23% of participants were excluded because they were unattended any follow up visit. Therefore this study might posses some selection bias. Moreover, a single reading of BP on only 1 visit may have served as a drawback because of large random fluctuations in a casual reading.
In conclusion, serum GGT was an early predictor for progression of prehypertension in healthy Korean men. Therefore increased serum GGT level is implicated in increased BP and the progression of prehypertension. In addition, it is needed to determine whether a more aggressive intervention, such as nutritional or lifestyle modifications that decrease serum GGT level, will decrease the risk of prehypertension.
Figures and Tables
Table 1
Baseline characteristics of participants according to quartile groups of serum GGT level (n=13,435)
References
1. Whitfield JB. Gamma glutamyltransferase. Crit Rev Clin Lab Sci. 2001; 38:263–355.
2. Paolicchi A, Tongiani R, Tonarelli P, Comporti M, Pompella A. Gamma-glutamyltranspeptidase-dependent lipid peroxidation in isolated hepatocytes and HepG2 hepatoma cells. Free Radic Biol Med. 1997; 22:853–860.
3. Lee DH, Blomhoff R, Jacobs DR Jr. Is serum gamma glutamyltransferase a marker of oxidative stress? Free Radic Res. 2004; 38:535–539.
4. Lee DH, Silventoinen K, Hu G, Jacobs DR Jr, Jousilahti P, Sundvall J, Tuomilehto J. Serum gamma-glutamyltransferase predicts non-fatal myocardial infarction and fatal coronary heart disease among 28,838 middle-aged men and women. Eur Heart J. 2006; 27:2170–2176.
5. Lee DS, Evans JC, Robins SJ, Wilson PW, Albano I, Fox CS, Wang TJ, Benjamin EJ, D'Agostino RB, Vasan RS. Gamma glutamyltransferase and metabolic syndrome, cardiovascular disease, and mortality risk: the Framingham Heart Study. Arterioscler Thromb Vasc Biol. 2007; 27:127–133.
6. Lee DH, Jacobs DR Jr, Gross M, Kiefe CI, Roseman J, Lewis CE, Steffes M. Gamma-glutamyltransferase is a predictor of incident diabetes and hypertension: the Coronary Artery Risk Development in Young Adults (CARDIA) Study. Clin Chem. 2003; 49:1358–1366.
7. Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL Jr, Jones DW, Materson BJ, Oparil S, Wright JT Jr, et al. Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. National Heart, Lung, and Blood Institute. National High Blood Pressure Education Program Coordinating Committee. Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension. 2003; 42:1206–1252.
8. De Marco M, de Simone G, Roman MJ, Chinali M, Lee ET, Russell M, Howard BV, Devereux RB. Cardiovascular and metabolic predictors of progression of prehypertension into hypertension: the Strong Heart Study. Hypertension. 2009; 54:974–980.
9. Vasan RS, Larson MG, Leip EP, Kannel WB, Levy D. Assessment of frequency of progression to hypertension in non-hypertensive participants in the Framingham Heart Study: a cohort study. Lancet. 2001; 358:1682–1686.
10. Zhang Y, Lee ET, Devereux RB, Yeh J, Best LG, Fabsitz RR, Howard BV. Prehypertension, diabetes, and cardiovascular disease risk in a population-based sample: the Strong Heart Study. Hypertension. 2006; 47:410–414.
11. Yamada Y, Ishizaki M, Kido T, Honda R, Tsuritani I, Ikai E, Yamaya H. Alcohol, high blood pressure, and serum gamma-glutamyltranspeptidase level. Hypertension. 1991; 18:819–826.
12. Nilssen O, Førde OH, Brenn T. The Tromsø Study: distribution and population determinants of gamma-glutamyltransferase. Am J Epidemiol. 1990; 132:318–326.
13. Shankar A, Li J. Association between serum gamma-glutamyltransferase level and prehypertension among US adults. Circ J. 2007; 71:1567–1572.
14. Kawamoto R, Kohara K, Tabara Y, Kusunoki T, Otsuka N, Miki T. Association between serum gamma-glutamyltransferase level and prehypertension among community-dwelling men. Tohoku J Exp Med. 2008; 216:213–221.
15. Karakurt O, Cagirici G, Eryasar NE. Gamma-glutamyltransferase activity increases in prehypertensive patients. Turk J Med Sci. 2011; 41:975–980.
16. Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC. Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia. 1985; 28:412–419.
17. Skurtveit S, Tverdal A. Sex differences in gamma-glutamyltransferase in people aged 40-42 years in two Norwegian counties. Drug Alcohol Depend. 2002; 67:95–98.
18. Pintus F, Mascia P. Distribution and population determinants of gamma-glutamyltransferase in a random sample of Sardinian inhabitants: 'ATS-SARDEGNA' Research Group. Eur J Epidemiol. 1996; 12:71–76.
19. Lazo M, Selvin E, Clark JM. Brief communication: clinical implications of short-term variability in liver function test results. Ann Intern Med. 2008; 148:348–352.
20. Miura K, Nakagawa H, Nakamura H, Tabata M, Nagase H, Yoshida M, Kawano S. Serum gamma-glutamyltransferase level in predicting hypertension among male drinkers. J Hum Hypertens. 1994; 8:445–449.
21. Zhang H, Thijs L, Kuznetsova T, Fagard RH, Li X, Staessen JA. Progression to hypertension in the non-hypertensive participants in the Flemish Study on Environment, Genes and Health Outcomes. J Hypertens. 2006; 24:1719–1727.
22. Whelton PK, He J, Appel LJ, Cutler JA, Havas S, Kotchen TA, Roccella EJ, Stout R, Vallbona C, Karimbakas J, et al. National High Blood Pressure Education Program Coordinating Committee. Primary prevention of hypertension: clinical and public health advisory from the National High Blood Pressure Education Program. JAMA. 2002; 288:1882–1888.
23. Winegarden CR. From "prehypertension" to hypertension? additional evidence. Ann Epidemiol. 2005; 15:720–725.
24. Pastore A, Federici G, Bertini E, Piemonte F. Analysis of glutathione: implication in redox and detoxification. Clin Chim Acta. 2003; 333:19–39.
25. Haynes WG, Morgan DA, Walsh SA, Sivitz WI, Mark AL. Cardiovascular consequences of obesity: role of leptin. Clin Exp Pharmacol Physiol. 1998; 25:65–69.
26. Lee DH, Jacobs DR Jr. Association between serum gamma-glutamyltransferase and C-reactive protein. Atherosclerosis. 2005; 178:327–330.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download