Abstract
An abnormal dipping pattern in ambulatory blood pressure monitoring (ABPM) is a cardiovascular (CV) risk factor. However, its impact on CV mortality has not been investigated sufficiently in clinical practice to be considered a standard parameter. We assessed the association between abnormal dipping patterns and increased CV mortality in a tertiary hospital in Korea. Our retrospective cohort study included 401 patients who underwent ABPM between 1994 and 1996 in Hanyang University Hospital, Seoul, Korea. The patients were classified as risers (<0% drop in systolic BP; n=107), and others included dippers and non-dippers (≥0% drop, n=294). The follow-up period was 120 months. The frequency of CV mortality was 14.0% in risers and 5.8% in others. A Cox regression analysis found a significant association between dipping pattern and CV mortality, after adjusting for age, gender, body mass index, hypertension, diabetes mellitus, smoking and hypercholesterolemia. Risers were at greater risk of CV death than others (RR, 3.02, P=0.022), but there was no difference in event rates between dippers and non-dippers. The reverse dipping pattern may be more frequent in clinical settings than in the population at large, and it is strongly associated with increased risk of CV mortality in Korea.
Over the past decades, ambulatory blood pressure monitoring (ABPM) has provided unique information about the circadian variation of blood pressure (BP) (1, 2). Various features of the 24-hr pattern detected by ABPM have been assessed as potential triggers of target organ damage and cardiovascular (CV) events (3, 4). Particular attention has been paid to nocturnal BP variation, due to its association with poor CV prognosis (5).
Studies have shown that non-dippers (i.e. patients in whom the nocturnal BP decline is blunted or absent) have more subclinical and clinical cardiovascular target organ damage than dippers (6, 7). Moreover, prospective studies using ABPM have shown that nocturnal BP is closely associated with cardiovascular disease (CVD), and the non-dipping and reverse-dipping patterns of nocturnal BP are independent predictors of CVD (2, 8, 9).
To date, the impact of abnormal dipping patterns on cardiovascular mortality in Korean patients has never been evaluated in routine clinical practice to be considered a standard parameter. Thus, our study aimed to investigate retrospectively the all-cause and CV mortality of Korean patients with abnormal BP dipping patterns. This is the first study regarding ABPM on cardiovascular mortality in Korea.
For the purpose of our retrospective cohort study, we analyzed the complete records of 719 patients who underwent ABPM between January 1994 and December 1996 in the Cardiology Center of Hanyang University Hospital in Seoul, Korea (10). Clinical indications for ABPM included newly diagnosed hypertension, decision to start antihypertensive medication, suspected white-coat hypertension, uncontrolled hypertension despite treatment, and suspected hypotensive episodes. The exclusion criteria included incomplete clinical data, age<30 or >70 yr, BP reading success rate<85%, and insufficient numbers of daytime and night-time readings (daytime<14 measurements and night-time<7 measurements) (11). Also excluded were patients with advanced cancer, chronic obstructive pulmonary disease (COPD), liver cirrhosis that resulted in death within one month, and congenital heart disease, valvular heart disease. Because of effect to reliability of ABPM data, night-workers and patients with chronic bedridden state, hypotensive episodes, secondary hypertension, and sleep disorders were excluded (7). Hypertension was defined as clinical systolic BP ≥140 mmHg, or clinical diastolic BP ≥90 mmHg or taking of anti-hypertensive medication, while diabetes mellitus (DM) was defined as fasting blood glucose ≥126 mg/dL or a recorded diagnosis of diabetes. Previous history of CVD was defined as history of heart failure, coronary artery disease (CAD), stroke, or transient ischemic attack (TIA). A final cohort of 401 patients was included in the study (Fig. 1). Patient height, weight, clinical BP, heart rate, and clinical parameters such as smoking status, anti-hypertensive medication status, total cholesterol, and fasting blood glucose were included in the analysis.
Clinical BP was measured with a mercury sphygmomanometer by a physician or qualified nurse, and the average of at least 3 measurements was recorded. Ambulatory BP was recorded using a TM-2421 blood pressure monitor (A&D, Saitama, Japan). The device has undergone independent validation (12, 13). The device was applied to the non-dominant arm for 24 hr, and BP was measured every 15 min during daytime and every 30 min at night. Patients were instructed to maintain their usual activities during monitoring (walking, sleeping, eating and other activities), and to stay calm when sensing cuff inflation. Sleep and waking times were self-reported by the patients.
Nocturnal BP was defined by narrow fixed interval method from 1 a.m. to 6 a.m. as nocturnal systolic/diastolic mean BP. Daytime BP was defined by mean systolic/diastolic BP during 9 a.m. to 9 p.m. 24-hr BP was defined by (nocturnal BP×actual sleep interval + daytime BP×awake interval)/24 (11). Nocturnal dipping was calculated as the percentage decrease in nocturnal systolic BP compared to daytime systolic BP. We classified the patients by their nocturnal dipping patterns as follows: 1) risers, if the dip was <0%; 2) non-dippers, if it was ≥0% but <10%; 3) dippers, if it was ≥10% but <20%, and 4) extreme dippers, if the dip was ≥20%. Hypertension was defined as clinical systolic BP ≥140 mmHg, or clinical diastolic BP ≥90 mmHg or on antihypertensive medication.
In Korea, every individual has a unique identification number that is widely used by social-service and health-care providers. In 2010 we analyzed hospital medical records and mortality data from Statistics Korea to determine the patients' survival and cause of death. The International Classification of Diseases (ICD) is used to code and classify mortality data from death certificates in Statistics Korea, a central government organization for statistics. In this study, we identified all cause of death from ICD code of death certificates. All CV deaths that occurred since the ABPM (i.e. myocardial infarction, stroke, death due to ischemic heart disease, stroke or congestive heart failure, and sudden death) were recorded, with their dates.
Qualitative variables are reported as frequencies and percentages, and quantitative variables as means±standard deviation (SD). Differences between the four groups as a function of dipping pattern were assessed by analysis of variance (ANOVA), Kruskal-Wallis tests and independent t-tests for continuous variables, and chi-square and Fisher's exact probability tests for categorical variables. Scheffe's test was used for post-hoc individual comparisons between groups after ANOVA.
Kaplan-Meier survival curves were plotted, and the log-rank test was used to compare groups. The Cox proportional regression model was used to determine hazard ratios (HR) for subsequent CV mortality. The multivariate model was systematically adjusted for age, gender, body mass index (BMI), history of cardiovascular disease, hypertension, anti-hypertensive medication, smoking, DM, and hypercholesterolemia. All tests were two-tailed, and P values less than 0.05 were considered statistically significant. Data were analyzed using IBM SPSS 19.0 software (IBM SPSS Inc., Chicago, IL, USA).
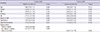
The patients' clinical characteristics are presented in Table 1. Of the 407 patients, 105 (25.8%) were classified as dippers, 189 (46.4%) as non-dippers, 107 (26.3%) as risers and 6 (1.5%) as extreme dippers. Extreme dipper group was excluded from statistical analysis because of too small number. Dipping were significantly lower in risers than in all the other patients (P<0.001).
There were 32 cardiovascular deaths during the follow-up period (5 in dippers, 12 in non-dippers and 15 in risers); the incidence of CV death was higher among the risers than the dippers and non-dippers (Table 1).
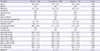
The Kaplan-Meier survival curves are shown in Fig. 2. The overall log-rank statistic for the three groups was 9.29 (P=0.001), while comparisons between the individual groups yielded 0.32 (P=0.571, dippers vs non-dippers), 6.07 (P=0.014, dippers vs risers) and 6.09 (P=0.014, non-dippers vs risers).
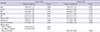
Age, obesity, smoking, DM, past history of CVD, hypercholesterolemia, and hypertension are well-known cardiovascular risk factors. When adjusted for age, gender, BMI, smoking, DM, hypercholesterolemia, hypertension, and the dipping pattern, a multivariate Cox regression analysis determined that age and DM was independent risk factors for CV mortality across all groups. In a two-group model (i.e. risers vs all other patients), risk factors were age, DM and reverse dipping pattern (Table 2).
When adjusted for age, gender, BMI, smoking, DM, hypercholesterolemia, hypertension, and the dipping pattern, a multivariate Cox regression analysis determined that age, gender, DM and dipping pattern was independent risk factors for all-cause mortality across all groups. In a two-group model (i.e. risers vs. all other patients), risk factors were age, gender, DM and reverse dipping pattern (Table 3).
Our study was conducted to further our understanding of different dipping patterns of ambulatory BP and their prognostic significance. Many previous studies showed that reverse dipping status was associated with higher mortality. Therefore, among different dipping patterns, especially, reverse dipping pattern was focused on (9, 14-16). We found that, in the Korean population, different dipping patterns were associated with different risks of all-cause and cardiovascular mortality. While this association was not significant overall (i.e. in the three-group model), there was an increased risk of CV death in risers compared to all other patients, which is consistent with previous studies (17, 18).
In other words, the results of this study were consistent with recent evidence that nocturnal BP is a better predictor of CV outcome (3, 19, 20). Several mechanisms have been proposed to explain higher nocturnal BP and associated worse CV mortality; nocturnal autonomic dysfunction, disturbed baroreflex sensitivity, abnormal sodium handling and nocturnal volume overload (21). The most plausible explanation in present study was nocturnal autonomic dysfunction. The much of patients in this study have complex diseases. A previous study showed that individuals with abnormal dipping pattern have autonomic dysfunction through the night and that abnormal dipping pattern are more commonly found among patients with complex diseases (7). Further prospective studies are needed to reveal which mechanism was dominant to explain association between higher nocturnal BP and worse CV mortality.
In contrast to several previous studies, patients with non-dipping pattern had similar risk of CV deaths, compared to those with dipping pattern in Cox regression model.
Numerous studies have shown that abnormal dipping pattern is highly prevalent in patients with diabetes mellitus (14, 15, 22). DM was found to be an independent risk factor for CV and all-cause mortality in three and two group models (Table 2 and 3). However, other traditional CV risk factor like hypertension, obesity, smoking were statistically insignificant in this study. Maybe several factors influenced this result. First, relatively small and heterogeneous study population was a possible factor. Second, there were 32 cardiovascular deaths during follow up. This small number of events increases the possibility of overfitting when several covariates are forced in the model. Third, a previous study showed that patients of abnormal dipping pattern have autonomic dysfunction through the night and that abnormal dipper pattern was more commonly found among individuals with DM (7). This previous study results suggest that characteristic of our study population influenced the statistical analysis.
Drawing the data from real-world clinical practice was an important advantage of our study. The numbers of risers are many as 26.3% in this population. A number of tertiary care patients present with complex diseases, e.g. ischemic heart disease, which are characterized by a high prevalence of non-dipping pattern (7). Because such patients were included in our study, our results apply also to complex cases. Despite extreme dippers were excluded from statistical analysis, when trying to make comparisons between the groups; nevertheless our results clearly show that the risk of CV death is over three times higher in risers than in other patients. However, as our study population was small, our results cannot be extrapolated to the population at large. It should also be pointed out that records concerning anti-hypertensive treatments were not complete in all cases, and due to the small sample size, we did not investigate different drug regimes. Consequently, the specific impact of anti-hypertensive treatments on nocturnal BP and cardiovascular events could not be assessed in detail. The BP lowering effect of anti-hypertensive drugs is widely known. However, their effects on nocturnal BP have not yet been established. For example, in one recent study, nocturnal BP was affected by the timing of anti-hypertensive treatment (23), while another study found no such effect (24). It is also unclear whether anti-hypertensive treatments affect the relationship between nocturnal BP and CV mortality, as the clinical effects of such treatments have not been studied. Further large-scale studies are needed to investigate the association between different classes of anti-hypertensive drugs, nocturnal BP and the risk of CV death.
Several limitations maybe affected this result. First, nocturnal BP was defined by narrow fixed interval method in this study. Analysis of nocturnal BP based on actual patients' report is reasonable. However, narrow fixed interval method is routinely applied in the analysis of ABPM data (25, 26). Second, possible variable such as BP, DM, smoking, hypercholesterolemia and antihypertensive treatment, were only assessed at baseline, and possible changes during follow up, which might have affected CV and all-cause death. Third, the reproducibility of the classification of dipping pattern based on single ABPM is still unknown enough to be accepted (27, 28). Maybe, most of this result is attributed to small number of CV death and heterogeneous study population. Interestingly, some meta-analysis suggested that prognosis was similar in non-dippers in comparison with dippers (18). However, in that meta-analysis, reverse dipping pattern was associated with a worse CV prognosis. That finding was consistent with our results.
In conclusion, the reverse dipping pattern is an independent predictor of CV death. In addition, reverse-dipping may be more frequent in real-world clinical practice than previously thought. Further well-designed clinical trials are necessary to confirm results and conclusions.
Figures and Tables
Fig. 2
Kaplan-Meier curves for survival with no cardiovascular death after ABPM for dippers, non-dippers, risers. The overall log-rank statistic for the three groups was 9.29 (P = 0.001).
References
1. Ben-Dov IZ, Kark JD, Ben-Ishay D, Mekler J, Ben-Arie L, Bursztyn M. Predictors of all-cause mortality in clinical ambulatory monitoring: unique aspects of blood pressure during sleep. Hypertension. 2007; 49:1235–1241.
2. Staessen JA, Thijs L, Fagard R, O'Brien ET, Clement D, de Leeuw PW, Mancia G, Nachev C, Palatini P, Parati G, et al. Predicting cardiovascular risk using conventional vs ambulatory blood pressure in older patients with systolic hypertension: Systolic hypertension in Europe trial investigators. JAMA. 1999; 282:539–546.
3. Dolan E, Stanton A, Thijs L, Hinedi K, Atkins N, McClory S, Den Hond E, McCormack P, Staessen JA, O'Brien E. Superiority of ambulatory over clinic blood pressure measurement in predicting mortality: the Dublin Outcome Study. Hypertension. 2005; 46:156–161.
4. Kim SG. Clinical implications of ambulatory and home blood pressure monitoring. Korean Circ J. 2010; 40:423–431.
5. Verdecchia P, Porcellati C, Schillaci G, Borgioni C, Ciucci A, Battistelli M, Guerrieri M, Gatteschi C, Zampi I, Santucci A, et al. Ambulatory blood pressure: an independent predictor of prognosis in essential hypertension. Hypertension. 1994; 24:793–801.
6. Kim BK, Lim YH, Lee HT, Lee JU, Kim KS, Kim SG, Kim JH, Lim HK, Shin J. Non-dipper pattern is a determinant of the inappropriateness of left ventricular mass in essential hypertensive patients. Korean Circ J. 2011; 41:191–197.
7. Routledge FS, McFetridge-Durdle JA, Dean CR. Canadian Hypertension Society. Night-time blood pressure patterns and target organ damage: a review. Can J Cardiol. 2007; 23:132–138.
8. Fagard RH, Celis H, Thijs L, Staessen JA, Clement DL, De Buyzere ML, De Bacquer DA. Daytime and nighttime blood pressure as predictors of death and cause-specific cardiovascular events in hypertension. Hypertension. 2008; 51:55–61.
9. Ohkubo T, Imai Y, Tsuji I, Nagai K, Watanabe N, Minami N, Kato J, Kikuchi N, Nishiyama A, Aihara A, et al. Relation between nocturnal decline in blood pressure and mortality: the Ohasama Study. Am J Hypertens. 1997; 10:1201–1207.
10. Shin JH, Lee KJ, Lee J, Choi JH, Lee JU, Kim KS, Kim SK. Significance of nocturnal blood pressure changes by ambulatory blood pressure monitoring. Hanyang J Med. 1997; 17:133–142.
11. O'Brien E, Asmar R, Beilin L, Imai Y, Mallion JM, Mancia G, Mengden T, Myers M, Padfield P, Palatini P, et al. European Society of Hypertension recommendations for conventional, ambulatory and home blood pressure measurement. J Hypertens. 2003; 21:821–848.
12. Imai Y, Sasaki S, Minami N, Munakata M, Hashimoto J, Sakuma H, Sakuma M, Watanabe N, Imai K, Sekino H, et al. The accuracy and performance of the A&D TM 2421, a new ambulatory blood pressure monitoring device based on the cuff-oscillometric method and the Korotkoff sound technique. Am J Hypertens. 1992; 5:719–726.
13. O'Brien E, Atkins N, Staessen J. State of the market: a review of ambulatory blood pressure monitoring devices. Hypertension. 1995; 26:835–842.
14. Liniger C, Favre L, Assal JP. Twenty-four hour blood pressure and heart rate profiles of diabetic patients with abnormal cardiovascular reflexes. Diabet Med. 1991; 8:420–427.
15. Nakano S, Fukuda M, Hotta F, Ito T, Ishii T, Kitazawa M, Nishizawa M, Kigoshi T, Uchida K. Reversed circadian blood pressure rhythm is associated with occurrences of both fatal and nonfatal vascular events in NIDDM subjects. Diabetes. 1998; 47:1501–1506.
16. Ohkubo T, Hozawa A, Yamaguchi J, Kikuya M, Ohmori K, Michimata M, Matsubara M, Hashimoto J, Hoshi H, Araki T, et al. Prognostic significance of the nocturnal decline in blood pressure in individuals with and without high 24-h blood pressure: the Ohasama Study. J Hypertens. 2002; 20:2183–2189.
17. Boggia J, Li Y, Thijs L, Hansen TW, Kikuya M, Björklund-Bodegård K, Richart T, Ohkubo T, Kuznetsova T, Torp-Pedersen C, et al. Prognostic accuracy of day versus night ambulatory blood pressure: a cohort study. Lancet. 2007; 370:1219–1229.
18. Fagard RH. Dipping pattern of nocturnal blood pressure in patients with hypertension. Expert Rev Cardiovasc Ther. 2009; 7:599–605.
19. Fagard RH, Thijs L, Staessen JA, Clement DL, De Buyzere ML, De Bacquer DA. Prognostic significance of ambulatory blood pressure in hypertensive patients with history of cardiovascular disease. Blood Press Monit. 2008; 13:325–332.
20. Fagard RH, Thijs L, Staessen JA, Clement DL, De Buyzere ML, De Bacquer DA. Night-day blood pressure ratio and dipping pattern as predictors of death and cardiovascular events in hypertension. J Hum Hypertens. 2009; 23:645–653.
21. Redon J, Lurbe E. Nocturnal blood pressure versus nondipping pattern: what do they mean? Hypertension. 2008; 51:41–42.
22. Cuspidi C, Vaccarella A, Leonetti G, Sala C. Ambulatory blood pressure and diabetes: targeting nondipping. Curr Diabetes Rev. 2010; 6:111–115.
23. Hermida RC, Ayala DE, Mojón A, Fernández JR. Effects of time of antihypertensive treatment on ambulatory blood pressure and clinical characteristics of subjects with resistant hypertension. Am J Hypertens. 2010; 23:432–439.
24. De la Sierra A, Redon J, Banegas JR, Segura J, Parati G, Gorostidi M, de la Cruz JJ, Sobrino J, Llisterri JL, Alonso J, et al. Prevalence and factors associated with circadian blood pressure patterns in hypertensive patients. Hypertension. 2009; 53:466–472.
25. Palatini P, Mormino P, Canali C, Santonastaso M, De Venuto G, Zanata G, Pessina AC. Factors affecting ambulatory blood pressure reproducibility: results of the HARVEST Trial: hypertension and ambulatory recording venetia study. Hypertension. 1994; 23:211–216.
26. Staessen J, Bulpitt CJ, O'Brien E, Cox J, Fagard R, Stanton A, Thijs L, Van Hulle S, Vyncke G, Amery A. The diurnal blood pressure profile: a population study. Am J Hypertens. 1992; 5:386–392.
27. Parati G, Staessen JA. Day-night blood pressure variations: mechanisms, reproducibility and clinical relevance. J Hypertens. 2007; 25:2377–2380.
28. Manning G, Rushton L, Donnelly R, Millar-Craig MW. Variability of diurnal changes in ambulatory blood pressure and nocturnal dipping status in untreated hypertensive and normotensive subjects. Am J Hypertens. 2000; 13:1035–1038.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download