Abstract
Although many studies have assessed mortality and morbidity of conservative treatment after hip fracture in elderly patients, the mortality of conservative treatment done because of economic burden is unclear. Among 451 patients diagnosed with displaced hip fracture during 3 yr, 28 patients (Group I) were enrolled as conservative treatment. Fifty-six patients matched in age, gender, ASA score, and diagnosis (Group II) who had undergone surgical treatment were used as the control group. The causal factors of non-operative treatment and mortality rate and functional recovery were evaluated according to the causal factors of patients with surgical procedure. Ten patients (36%) in Group I involved medical problems and 18 (64%) by economic burdens. The cumulative mortality rate over 3, 6, 12, and 24 months was 54%, 61%, 64%, and 82% in Group I and 9%, 11%, 14%, and 21% in Group II, respectively. At the latest follow-up, all five patients in Group I displayed a nonfunctional ambulatory state, whereas only seven of 44 patients in Group II were in a nonfunctional ambulatory state. Non-surgical treatment following hip fracture that is done because of the economic burden is associated with substantially high mortality and serious functional loss.
Hip fractures are a disabling event and an important cause of morbidity and mortality in elderly people (1-4). The majority of patients following hip fracture are treated operatively to obtain pain relief, hasten mobility, and minimize complications. The indications of conservative treatment after hip fracture in previous reported studies were patients with impacted femoral neck fracture, minimally symptomatic following late diagnosis of hip fracture, already bed-ridden, and significant medical co-morbidity (5-8).
In these patients, high mortality rates in cases with conservative treatment were reported because of poor medical comorbidity (7-9). However, little information is available concerning the prognosis of elderly patients who need surgical intervention but who are discharged without surgery after hip fracture because of economic burden.
The purpose of this study was to determine the causal factors of non-operative treatment following hip fracture and mortality rate and functional recovery according to the causal factors compared to that of patients who underwent surgery.
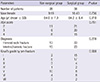
Between January 2009 and December 2011, 451 patients were diagnosed as femoral neck or intertrochanteric fractures. Of these, we identified 32 elderly patients (patients over 65-yr-of-age, 32 hips) with hip fracture who refused surgical treatment and received non-operative procedure at the author's hospital. The diagnostic criteria of hip fracture were a displaced femoral neck or intertrochanteric fracture. The exclusion criteria were impacted femoral neck fracture, isolated trochanteric fracture, high-energy injury such as traffic accident, and metastatic pathological femur fractures. We excluded four patients from enrollment: two patients with pathological fracture and two patients with traumatic trochanteric fracture of the femur. The remaining 28 patients (Group I) were enrolled. Fifty six age-, gender-, American Society of Anesthesiologist (ASA) score- (10), and diagnosis-matched patients with hip fracture who had undergone surgical treatment at our hospital were used as the control group (Group II) in a two-to-one ratio using the propensity scoring method. Demographic data including gender, age, initial diagnosis, ASA score, and pre-fracture ambulatory status by Koval's categories (11) were obtained by reviewing medical records (Table 1).
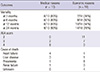
The causes of operation refusal were obtained by reviewing medical records and interview with patients or family members. Change of patient activity and mortality were compared within a minimum of one year between the two groups. Activity levels were defined as follows: I, independent community ambulatory; II, community ambulatory with cane; III, community ambulatory with walker/crutches; IV, independent household ambulator; V, household ambulatory with cane; VI, household ambulatory with walker/crutches, and VII, nonfunctional ambulatory (11). In the analysis, Koval's grade I, II, and III cases were also classified as ambulatory outdoors, whereas Koval's grade IV, V, VI, and VII cases were classified as shut-in patients. Mortality status was identified using hospital records and/or by interviews with family members. Patients unable to attend follow-up evaluations were interviewed by telephone. During the follow-up evaluations, care was taken to interview the caregiver previously interviewed during the patient's hospitalization. This clinical information was collected by one orthopedic surgeon and two nurses.
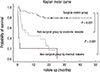
The propensity score matching method using age, gender, ASA score, and diagnosis was used for a comparable control group retrospectively. Cumulative crude mortality rate were calculated at 3, 6, 12, and 24, months and compared between the two groups. Kaplan-Meier survival analysis was performed on both of the groups with a minimum 12 months follow-up using mortality as a primary end point. The correlation of survival rate in both groups was tested by the log-rank test. The Student's t-test was used to analyze age, and the Mann-Whitney to analyze ASA score and Koval's grade. The chi square test was used to analyze gender, diagnosis, and cumulative mortality. The analyses were carried out using SPSS version 18.0 (Chicago, IL, USA). All reported P values are two sided and P<0.05 was considered significant.
Of 28 patients who could not receive operative treatment, the reason in 10 patients (36%) was medical problems with high-risk of surgery. The reason for the remaining 18 (64%) was economic burden, even if surgery is quite possible.
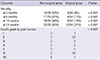
The cumulative mortality rate over 3, 6, and 12 months post-fracture was 54%, 61%, and 64% in Group I and 9%, 11%, and 14% in Group II, respectively. The cumulative mortality rate was 82% (23/28) at 24 months in Group I and 21% (12/56) at 24 months in Group II (Table 2).
With regard to the cause-specific mortality in Group I, the cumulative mortality rate over the 3, 6, and 12 months post-fracture was consistently 80% in 10 patients who refused surgery for medical problems and 39%, 50%, and 56% in 18 patients who refused surgery because of economic burdens. The cumulative mortality rate at the 24-month follow-up was 90% (9/10) and 78% (14/18), respectively (Table 3). The cause of death in Group I by medical reasons was patient medical comorbidity. The cause of death in Group I by economic reasons was pneumonia (n=8), congestive heart failure (n=1), chronic liver disease (n=1), and unknown reasons (n=4).
Kaplan-Meier survivorship analysis with mortality as the end point in Group I and Group II estimated a 57.1% (95% confidence interval, 38.7% to 75.5%) chance of survival during 12 months and 82.1% (95% confidence interval, 72.1% to 92.1%) chance of survival during 12 months, respectively (Fig. 1). In subgroup analysis of Group I, the survival rate was 20.0% (95% confidence interval, 0% to 44.7%) with mortality as the end point at 12 months in the medical reason group and 38.1% (95% confidence interval, 15.4% to 60.8%) with mortality as the end point at 12 months in the economic reason group, respectively.
Of the Group I patients at final follow-up, five patients were alive and all were in a nonfunctional ambulatory state (Koval's grade VII) (Table 2). Of the Group II patients, 44 patients were alive, and 16 patients were outdoor ambulatory and 28 patients were shut-in patients. Only seven patients were in a nonfunctional ambulatory state (Koval's grade VII).
Although many studies have examined mortality and morbidity of conservative treatment after hip fracture in elderly patients, the mortality of conservative treatment that has been done because of economic burden (i.e., inability to pay the costs of surgery) after hip fracture is unclear. To the best of our knowledge, this study is the first study of mortality of conservative treatment after hip fracture in patients who refused surgery because of an economic burden. During the 3-yr study period, 18 of 28 patients who were diagnosed with displaced hip fracture and required surgery refused surgery because of an economic burden and instead received conservative treatment. At a minimum 12-month follow-up, mortality was 56% and all patients were bed-ridden.
Several recent observational studies addressing several different indications of conservative treatment after hip fracture in elderly patients reported favorable results. Hossain et al. (8) conducted a case-control study with 25 patients who were treated non-operatively and 22 patients treated surgically over the same time period. The authors reported that non-surgical treatment with early mobilization did not result in a statistically significant difference in functional outcome compared to surgical treatment patients. Gregory et al. (7) evaluated 102 patients diagnosed with a displaced intracapsular femoral neck fracture. Eighty of these patients underwent hemiarthroplasty and 22 were managed non-operatively because of an unacceptably high risk of death within the perioperative period despite medical optimization. The authors reported that the 30-day mortality in the hemiarthroplasty group was 4% (3/82) compared with 34% (7/22) in the non-operative group. Patients surviving 30 days after fracture had similar mortality rates at 1 yr, regardless of their treatment (27% non-operative vs 25% hemiarthroplasty). Raaymakers and Marti (12) performed a prospective observation study with 170 patients with impacted femoral neck fractures treated with early mobilization. Of these, 16% had died within 1 yr and 86% had achieved union. Although the impacted femoral neck fracture has been described as one of the possible indication of non-operative treatment in some articles, it should be treated surgically because of more than 15% of them displaced eventually. In addition, these findings were not consistent with other previous studies (13). Ions and Stevens (13) performed a prospective observation study with 158 patients who sustained hip fracture (135 in the operation group and 22 in the conservative treatment group). The authors reported that the 6-month mortality rate of the operation group was 9.6% (13 of 135) and that of the non-operated group who had severe medical comorbidity was 60.8% (14 of 23). In this study, the cumulative mortality rate at 6 months follow-up was 61% in Group I and 11% in Group II. In addition, subgroup analysis in conservative treatment group revealed 80% mortality in patients who had severe medical comorbidity and 50% mortality in patients who had refused surgery because of economic burden.
At the latest follow-up, five patients in Group I were all bed-ridden, but more than half of the remaining 44 patients in Group II were restored to the same pre-injury or Grade 1 reduced pre-injury activity levels. Therefore, conservative treatment after hip fracture might lead to serious dependency.
There were several limitations in our study. First, the study was retrospective and was performed in a cohort of prospectively followed patients. However, the study could not be prospectively randomized one because of the high mortality of non-operative treatment. Second, the study design included a small cohort of patients and so might not have had sufficient statistical power to be conclusive. However, the calculated sample size of only 20 patients was deemed sufficient because of the high mortality rate of 4-times that of the surgical control group. Third, our study did not include the medical status about enrolled patients. However, to make a matched case-control study by using a propensity scoring method, we used the ASA score as the medical status indicating the risk of surgery. White et al. (10) reported the ASA score is a reliable index of predictor of mortality and surgical risk. Fourth, the patients who refused surgery because of economic reasons were not universally followed-up. We persuaded the patients and their family and could finished interviews and get information with one orthopedic surgeon and two nurses.
In conclusion, this study demonstrates that the conservative treatment following hip fracture due to economic burden is associated with substantially higher mortality and serious functional loss compared with patients who are treated surgically. This finding should be important for health affiliations and health care providers, and health policy decision makers should take action to reduce mortality and maintain functional activity in elderly patients who refuse surgical treatment.
Figures and Tables
References
1. Bhattacharyya T, Iorio R, Healy WL. Rate of and risk factors for acute inpatient mortality after orthopaedic surgery. J Bone Joint Surg Am. 2002; 84-A:562–572.
2. Kanis JA, Oden A, Johnell O, De Laet C, Jonsson B, Oglesby AK. The components of excess mortality after hip fracture. Bone. 2003; 32:468–473.
3. Yoon HK, Park C, Jang S, Jang S, Lee YK, Ha YC. Incidence and mortality following hip fracture in Korea. J Korean Med Sci. 2011; 26:1087–1092.
4. Kim SR, Ha YC, Park YG, Lee SR, Koo KH. Orthopedic surgeon's awareness can improve osteoporosis treatment following hip fracture: a prospective cohort study. J Korean Med Sci. 2011; 26:1501–1507.
5. Parker M, Johansen A. Hip fracture. BMJ. 2006; 333:27–30.
6. Neuman MD, Fleisher LA, Even-Shoshan O, Mi L, Silber JH. Nonoperative care for hip fracture in the elderly: the influence of race, income, and comorbidities. Med Care. 2010; 48:314–320.
7. Gregory JJ, Kostakopoulou K, Cool WP, Ford DJ. One-year outcome for elderly patients with displaced intracapsular fractures of the femoral neck managed non-operatively. Injury. 2010; 41:1273–1276.
8. Hossain M, Neelapala V, Andrew JG. Results of non-operative treatment following hip fracture compared to surgical intervention. Injury. 2009; 40:418–421.
9. Jain R, Basinski A, Kreder HJ. Nonoperative treatment of hip fractures. Int Orthop. 2003; 27:11–17.
10. White BL, Fisher WD, Laurin CA. Rate of mortality for elderly patients after fracture of the hip in the 1980's. J Bone Joint Surg Am. 1987; 69:1335–1340.
11. Koval KJ, Aharonoff GB, Rosenberg AD, Bernstein RL, Zuckerman JD. Functional outcome after hip fracture: effect of general versus regional anesthesia. Clin Orthop Relat Res. 1998; (348):37–41.
12. Raaymakers EL, Marti RK. Non-operative treatment of impacted femoral neck fractures: a prospective study of 170 cases. J Bone Joint Surg Br. 1991; 73:950–954.
13. Ions GK, Stevens J. Prediction of survival in patients with femoral neck fractures. J Bone Joint Surg Br. 1987; 69:384–387.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download