Abstract
Despite recent successful efforts to shorten the door-to-balloon time in patients with acute ST-segment elevation myocardial infarction (STEMI), prehospital delay remains unaffected. Nonetheless, the factors associated with prehospital delay have not been clearly identified in Korea. We retrospectively evaluated 423 patients with STEMI. The mean symptom onset-to-door time was 255 ± 285 (median: 150) min. The patients were analyzed in two groups according to symptom onset-to-door time (short delay group: ≤ 180 min vs long delay group: > 180 min). Inhospital mortality was significantly higher in long delay group (6.9% vs 2.8%; P = 0.048). Among sociodemographic and clinical variables, diabetes, low educational level, triage via other hospital, use of private transport and night time onset were more prevalent in long delay group (21% vs 30%; P = 0.038, 47% vs 59%; P = 0.013, 72% vs 82%; P = 0.027, 25% vs 41%; P < 0.001 and 33% vs 48%; P = 0.002, respectively). In multivariate analysis, low educational level (1.66 [1.08-2.56]; P = 0.021), symptom onset during night time (1.97 [1.27-3.04]; P = 0.002), triage via other hospital (1.83 [1.58-5.10]; P = 0.001) and private transport were significantly associated with prehospital delay (3.02 [1.81-5.06]; P < 0.001). In conclusion, prehospital delay is more frequent in patients with low educational level, symptom onset during night time, triage via other hospitals, and private transport, and is associated with higher inhospital mortality.
Despite considerable improvement of care and outcomes of acute ST-segment elevation myocardial infarction (STEMI) in recent years, STEMI remains one of the most fatal disease in Korea as in the western and developing countries (1, 2). Because of the front wave of necrosis expanding from endocardium subtended by infarct artery, the size of infarction and mortality increases in proportion to the elapsed time after coronary artery occlusion (3, 4). Timely reperfusion of infarct related artery is the cornerstone of treatment for interrupting the progression of necrosis and salvaging myocardium (5, 6). The outcomes of reperfusion therapy are critically dependent on the ischemic time from the onset of symptoms to the treatment (7, 8).
Strategy to shorten the ischemic time involves integrated efforts to shorten the time delay in successive stages of patients' decision, transfer, and inhospital management. Recent efforts to implement the expedient reperfusion as recommended in clinical guidelines (door-to-needle time ≤ 30 min, door-to-balloon time ≤ 90 min) resulted in significant curtailment of inhospital time delay to treatment and improved clinical outcomes (9-11). However, time delay prior to hospital arrival has been largely unaffected, with little signs of change ever reported in recent years (12, 13).
Prehospital delay in patients with STEMI has been found to be an important factor of in-hospital and long-term mortality (14). Nonetheless, the magnitude of, and factors associated with prehospital time delay have not clearly identified in Korea. Accordingly, the purpose of this study was to investigate and clarify the factors related to prehospital time delay in patients with STEMI presented to the emergency department.
Patients aged 18 yr or older who presented with acute STEMI to the emergency department of Samsung Changwon Hospital from January 2008 to December 2010 were registered for the analysis. During this time, a total of 430 consecutive patients were hospitalized. Seven patients were excluded in whom the accurate time of symptom onset could not be determined.
Demographic, medical history and clinical characteristics were registered from the hospital records by trained physicians and nurses. Educated nurses gave a person-to-person call to patients or their family members and interviewed to ask questions enlisted in questionnaire and variables difficult to get from hospital records. Clinical as well as socioeconomic variables were investigated with regard to age, sex, characteristics of symptoms, time of symptom onset, activity at the time of onset, location of residence, level of education, attendance of family member or bystanders, knowledge about myocardial infarction, the first reaction of patient to initial symptom, means of transportation, and triage via other hospitals. Patients were divided into two groups according to prehospital time delay; short delay group in whom time from symptom onset to hospital arrival is 180 min or less, and long delay group in who the time is more than 180 min.
STEMI was defined according to the criteria of the universal definition of myocardial infarction (15). Crushing chest pain persisting longer than 20 min with or without diaphoresis was classified as typical symptoms, while other symptoms like shortness of breath, epigastric pain, nausea, and loss of consciousness were classified as atypical symptoms.
Symptom onset-to-door time was the time from the onset of symptoms to the arrival at the emergency department, and constitute a prehospital delay.
Categorical variables were summarized by counts and relative frequencies; numeric variables, by their median and range. Differences in patients' sociodemographic and clinical characteristics were compared between subgroups with chi-square test for categorical variables and Student t test for continuous variables. Overall survival was estimated using the Kaplan-Meier product limit method and differences in survival between groups were assessed by the log rank test. The logistic regression model was employed to identify the significant independent prognostic factors affecting response (symptom onset-to-door time). The multivariate model was created using a backward elimination method, and the probability was set at 0.05 for removal. Crude and adjusted odds ratios (OR) and 95% confidence interval (CI) were calculated. P values lower than 0.05 were considered statistically significant. This was a retrospective study therefore alpha was not adjusted for multiple testing. All statistical analyses were carried out using SPSS version 14.0 and MedCalc version 11.6.1 statistical software (SPSS Inc., Chicago, IL, USA).
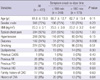
Baseline characteristics of 423 study patients are shown in Table 1. The mean age was 61.6 ± 13.0 yr, and 73% of the patients were male. Of all patients, 87% (n = 369) were eligible for thrombolysis or primary percutaneuous coronary intervention (PCI). Acute reperfusion therapy was performed in 95% of these patients (thrombolysis, 12 patients [3%]; primary PCI, 340 patients [97%]) (Table 2). The patients in the short- and long delay groups did not differ with respect to the demographic characteristics, social and past medical history, except for diabetes where the prevalence was higher in long delay group than in short delay group (30% vs 21%, P = 0.038).
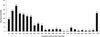
The mean symptom onset-to-door time of total 423 patients was 255 ± 285 (median: 150) min. Of the study groups, 337 patients (79.7%) arrived at the hospital within 6 hr of symptom onset and only 28 patients (6.6%) arrived within 30 min of symptom onset, a goal recommended in the recent guidelines (16) (Fig. 1).
The sociodemographic characteristics are presented in Table 3. Seventy-six percent of overall patients enrolled in this study was referred from other hospital or clinics. Among sociodemographic variables, low educational level, triage via other hospital, use of private transport, and symptom-onset during night time (6 pm-6 am) were more frequently observed in long delay group. Age, gender, characteristics of symptoms, previous ischemic heart disease (IHD), residential area, knowledge about acute myocardial infarction (AMI), and patients' responses to symptoms were not different between two groups.
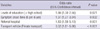
In univariate analysis, body mass index (BMI), history of diabetes, levels of education, symptom-onset-time, triage via referral hospital and use of private transport were significantly associated with prehospital delay (Table 4). By multiple logistic regression analysis, low levels of education (< high school), symptom onset during night time (6 pm-6 am), triage via other hospital and use of private transport were statistically significant factors associated with prehospital delay (Table 5).
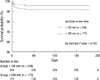
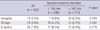
Nineteen patients (4.5%) had died during the admission (Table 6). Inhospital mortality was significantly higher in long delay group compared with short delay group (12 [6.9%] vs 7 [2.8%], P = 0.048). Mortality at 30 days and 6 month was also higher in the long delay group, but the difference was not statistically significant (10 [4.2%] vs 14 [8.1%], P = 0.092; 17 [6.3%] vs 17 [9.9%], P = 0.178, respectively) (Fig. 2). On Kaplan-Meier analysis the survival at 6 month was similar between two groups (Fig. 3).
In the reperfusion era, the outcomes of STEMI critically depend on the total ischemic time from the onset of symptom to treatment (7, 8). Prehospital delay is an important determinant of total ischemic time, yet unlike inhospital delay, it is difficult to employ systematic approach to reduce the delay substantially. Therefore, prehospital delay remains largely unchanged over recent years in spite of the notable improvement in reducing time delay in the hospital after patient's arrival (9-13).
The result of this study showed that in the typical Korean community comprised of a large city and surrounding suburban area, the time from symptom onset to hospital arrival was still too long for optimal management of the patients with acute STEMI. Prehospital time delay in this study (mean 255 ± 285 min; median 150 min) already exceeded the goal of total ischemic time 120 min (16). It has not been improved from earlier data of regional community in which median prehospital time delay was 172 min and also similar to previous nationwide registry data (17, 18). Although 79.7% of study patients arrived at the hospital within 6 hr of symptom onset, only 6.6% of the patients arrived within 30 min of symptom onset, which is the goal of the recent guideline for the optimal reperfusion (16).
It was noticeable that only 7% of study patients both in short and long delay group were aware of the possibility of acute MI. This might have deterred the patient's prompt action to call for help, and accounted for much of the delay. In addition, about 30% of the patients were using private transport to arrive at a hospital, and 76% of the patients were transferred via other hospital, contributing to delayed presentation. These data suggest that a nationwide and/or local-based coordinated effort is required to enhance public awareness for risk of STEMI and to build an efficient emergency dispatch system.
To find the factors that correlate with delayed hospital arrival, patient-related factors and sociodemogrpahic factors were sought in the study population. Multivairate logistic regression revealed that patient's level of education, symptom onset during night time, arrival via other hospital, and use of private transport were significant determinants for prehospital time delay. These findings differed from previous report that old age, female gender, diabetes, hypertension, previous history of coronary heart disease or coronary intervention were associated with prolonged prehospital delay (19-23). Relatively small sized study population, and low incidence of previous coronary disease in the present study may have reduced the power to discriminate the risk among the patients. Remarkably, low level of education (not completing high school) was significant factor for prehospital delay (hazard ratio 1.66) in this study. Shorter time of education has been also shown to increase the delay in an Australian study (24). It is conceivable that low level of patient education elicited slower reaction of patients, or it just might mirror the low socioeconomic status, which has been shown to be related to time delay (25). Night time onset and arrival via other hospitals were another factors, which was understandable and concurred with other study (17, 26). Most strongly associated with time delay was use of private transport as opposed to ambulance (hazard ratio 3.02), although the rate of private transport decreased considerably compared with previous regional community study in Korea (17). The cause of this relation is difficult to define, but private transportation may be accounted by other factors, such as low level of education or the lack of patient's perception of urgency. Prehospital triage by the emergency medical service should be encouraged because it is associated with a shorter time to treatment and more favorable clinical outcomes (27).
In this study, inhospital mortality was significantly higher in long delay group compared with short delay group. During the period of 30 days and 6 months follow-up, the mortality benefit of short treatment delay was continuously observed, although the differences were not statistically significant. Of the study patients eligible for reperfusion therapy, 340 (92%) of 369 patients were treated with primary PCI and the above result was consistent with previous report that treatment delay is critical determinants of outcomes after primary PCI (3). Several studies, mostly observational ones including Korean registry, have suggested that the time dependency of reperfusion effect was less pronounced in the setting of primary PCI than in fibrinolysis (18, 28, 29). However, the concept of "time-insensitivity" of primary PCI has been recently questioned because of the confounding factors associated with observational data (30). Therefore, although the role of primary PCI as a better reperfusion strategy is valid, the importance of reducing time delay should be applied to primary PCI, too.
Several limitations of this study warrant consideration. Firstly, the number of the patients in this study was relatively small. This might have deprived the power to detect the association between several variables and the time delay. Secondly, this study was retrospective, based on the information in the hospital medical records and interviews with patients and their family members, which could have been affected by recall bias. Finally, initial means of transportation and times between visiting first hospital and arriving in emergency department were not evaluated because of inaccurate information from referring hospitals. Despite the limitations, the present study could provide the descriptive data showing the current status of triage for emergency management of STEMI patients.
In conclusion, the present study demonstrated significant prehospital delay in the treatment of STEMI patients in Korean community and the delay was correlated with inhospital mortality. In Korean STEMI patients, low educational level, symptom onset during night time, triage via other hospital and private transport are associated with the treatment delay. Public campaigns, education and counseling of patients and their families are needed to raise the public awareness of STEMI that should prompt to seek immediate medical attention for optimal patients' outcomes.
Figures and Tables
References
1. Lloyd-Jones D, Adams R, Carnethon M, De Simone G, Ferguson TB, Flegal K, Ford E, Furie K, Go A, Greenlund K, et al. Heart disease and stroke statistics--2009 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation. 2009. 119:e21–e181.
2. Hong JS, Kang HC, Lee SH, Kim J. Long-term trend in the incidence of acute myocardial infarction in Korea: 1997-2007. Korean Circ J. 2009. 39:467–476.
3. De Luca G, Suryapranata H, Ottervanger JP, Antman EM. Time delay to treatment and mortality in primary angioplasty for acute myocardial infarction: every minute of delay counts. Circulation. 2004. 109:1223–1225.
4. Kloner RA, Jennings RB. Consequences of brief ischemia: stunning, preconditioning, and their clinical implications: part 1. Circulation. 2001. 104:2981–2989.
5. Van de Werf F, Bax J, Betriu A, Blomstrom-Lundqvist C, Crea F, Falk V, Filippatos G, Fox K, Huber K, Kastrati A, et al. Management of acute myocardial infarction in patients presenting with persistent ST-segment elevation: the Task Force on the Management of ST-Segment Elevation Acute Myocardial Infarction of the European Society of Cardiology. Eur Heart J. 2008. 29:2909–2945.
6. Schomig A, Ndrepepa G, Mehilli J, Schwaiger M, Schuhlen H, Nekolla S, Pache J, Martinoff S, Bollwein H, Kastrati A. Therapy-dependent influence of time-to-treatment interval on myocardial salvage in patients with acute myocardial infarction treated with coronary artery stenting or thrombolysis. Circulation. 2003. 108:1084–1088.
7. Francone M, Bucciarelli-Ducci C, Carbone I, Canali E, Scardala R, Calabrese FA, Sardella G, Mancone M, Catalano C, Fedele F, et al. Impact of primary coronary angioplasty delay on myocardial salvage, infarct size, and microvascular damage in patients with ST-segment elevation myocardial infarction: insight from cardiovascular magnetic resonance. J Am Coll Cardiol. 2009. 54:2145–2153.
8. Gersh BJ, Anderson JL. Thrombolysis and myocardial salvage. Results of clinical trials and the animal paradigm: paradoxic or predictable? Circulation. 1993. 88:296–306.
9. Nam YH, Cha KS, Kim JH, Park SY, Park TH, Kim MH, Kim YD. Reduction of door-to-balloon time by new performance processes in patients with ST-segment elevation myocardial infarction undergoing primary percutaneous coronary intervention. Angiology. 2011. 62:257–264.
10. Blankenship JC, Scott TD, Skelding KA, Haldis TA, Tompkins-Weber K, Sledgen MY, Donegan MA, Buckley JW, Sartorius JA, Hodgson JM, et al. Door-to-balloon times under 90 min can be routinely achieved for patients transferred for ST-segment elevation myocardial infarction percutaneous coronary intervention in a rural setting. J Am Coll Cardiol. 2011. 57:272–279.
11. Gross BW, Dauterman KW, Moran MG, Kotler TS, Schnugg SJ, Rostykus PS, Ross AM, Weaver WD. An approach to shorten time to infarct artery patency in patients with ST-segment elevation myocardial infarction. Am J Cardiol. 2007. 99:1360–1363.
12. McGinn AP, Rosamond WD, Goff DC Jr, Taylor HA, Miles JS, Chambless L. Trends in prehospital delay time and use of emergency medical services for acute myocardial infarction: experience in 4 US communities from 1987-2000. Am Heart J. 2005. 150:392–400.
13. Goldberg RJ, Gurwitz JH, Gore JM. Duration of, and temporal trends (1994-1997) in, prehospital delay in patients with acute myocardial infarction: the second National Registry of Myocardial Infarction. Arch Intern Med. 1999. 159:2141–2147.
14. Turi ZG, Stone PH, Muller JE, Parker C, Rude RE, Raabe DE, Jaffe AS, Hartwell TD, Robertson TL, Braunwald E. Implications for acute intervention related to time of hospital arrival in acute myocardial infarction. Am J Cardiol. 1986. 58:203–209.
15. Thygesen K, Alpert JS, White HD. Universal definition of myocardial infarction. Eur Heart J. 2007. 28:2525–2538.
16. Antman EM, Anbe DT, Armstrong PW, Bates ER, Green LA, Hand M, Hochman JS, Krumholz HM, Kushner FG, Lamas GA, et al. ACC/AHA guidelines for the management of patients with ST-elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to Revise the 1999 Guidelines for the Management of Patients with Acute Myocardial Infarction). Circulation. 2004. 110:e82–e292.
17. Kim JA, Jeong JO, Ahn KT, Park HS, Jang WI, Kim MS, Kim JH, Park JH, Lee JH, Choi SW, et al. Causative factors for time delays in patients with acute ST-segment elevation myocardial infarction undergoing primary percutaneous coronary intervention. Korean J Med. 2010. 78:586–594.
18. Song YB, Hahn JY, Gwon HC, Kim JH, Lee SH, Jeong MH. The impact of initial treatment delay using primary angioplasty on mortality among patients with acute myocardial infarction: from the Korea acute myocardial infarction registry. J Korean Med Sci. 2008. 23:357–364.
19. Nguyen HL, Gore JM, Saczynski JS, Yarzebski J, Reed G, Spencer FA, Goldberg RJ. Age and sex differences and 20-year trends (1986 to 2005) in prehospital delay in patients hospitalized with acute myocardial infarction. Circ Cardiovasc Qual Outcomes. 2010. 3:590–598.
20. Perkins-Porras L, Whitehead DL, Strike PC, Steptoe A. Pre-hospital delay in patients with acute coronary syndrome: factors associated with patient decision time and home-to-hospital delay. Eur J Cardiovasc Nurs. 2009. 8:26–33.
21. Saczynski JS, Yarzebski J, Lessard D, Spencer FA, Gurwitz JH, Gore JM, Goldberg RJ. Trends in prehospital delay in patients with acute myocardial infarction (from the Worcester Heart Attack Study). Am J Cardiol. 2008. 102:1589–1594.
22. Berton G, Cordiano R, Palmieri R, Guarnieri G, Stefani M, Palatini P. Clinical features associated with pre-hospital time delay in acute myocardial infarction. Ital Heart J. 2001. 2:766–771.
23. Sheifer SE, Rathore SS, Gersh BJ, Weinfurt KP, Oetgen WJ, Breall JA, Schulman KA. Time to presentation with acute myocardial infarction in the elderly: associations with race, sex, and socioeconomic characteristics. Circulation. 2000. 102:1651–1656.
24. Dracup K, McKinley SM, Moser DK. Australian patients' delay in response to heart attack symptoms. Med J Aust. 1997. 166:233–236.
25. Foraker RE, Rose KM, McGinn AP, Suchindran CM, Goff DC Jr, Whitsel EA, Wood JL, Rosamond WD. Neighborhood income, health insurance, and prehospital delay for myocardial infarction: the atherosclerosis risk in communities study. Arch Intern Med. 2008. 168:1874–1879.
26. Ribeiro S, Gaspar A, Rocha S, Nabais S, Azevedo P, Salgado A, Pereira MA, Correia A. Predictors of pre-hospital delay in patients with ST-segment elevation myocardial infarction. Rev Port Cardiol. 2010. 29:1521–1532.
27. Postma S, Dambrink JH, de Boer MJ, Gosselink AT, Eggink GJ, van de Wetering H, Hollak F, Ottervanger JP, Hoorntje JC, Kolkman E, et al. Prehospital triage in the ambulance reduces infarct size and improves clinical outcome. Am Heart J. 2011. 161:276–282.
28. Zijlstra F, Patel A, Jones M, Grines CL, Ellis S, Garcia E, Grinfeld L, Gibbons RJ, Ribeiro EE, Ribichini F, et al. Clinical characteristics and outcome of patients with early (<2 h), intermediate (2-4 h) and late (>4 h) presentation treated by primary coronary angioplasty or thrombolytic therapy for acute myocardial infarction. Eur Heart J. 2002. 23:550–557.
29. Cannon CP, Gibson CM, Lambrew CT, Shoultz DA, Levy D, French WJ, Gore JM, Weaver WD, Rogers WJ, Tiefenbrunn AJ. Relationship of symptom-onset-to-balloon time and door-to-balloon time with mortality in patients undergoing angioplasty for acute myocardial infarction. JAMA. 2000. 283:2941–2947.
30. Terkelsen CJ, Christiansen EH, Sorensen JT, Kristensen SD, Lassen JF, Thuesen L, Andersen HR, Vach W, Nielsen TT. Primary PCI as the preferred reperfusion therapy in STEMI: it is a matter of time. Heart. 2009. 95:362–369.




 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download