Abstract
In general, a 2-yr disease-free duration is recommended before kidney transplantation (KT) in end-stage renal disease (ESRD) patients who also have acute leukemia. However, the optimal disease-free interval has not been specified for all subtypes of acute leukemia. Among these subtypes, acute promyelocytic leukemia (APL) shows a favorable prognosis and low relapse rate compared to other types of leukemia. We here report KT after complete remission (CR) of APL in an ESRD patient. Irreversible kidney injury developed in a 23-yr-old man with APL. First, we induced CR and subsequently performed KT 7 months after the achievement of CR. The patient's clinical course after KT was favorable, without allograft rejection or relapse of APL up to1 yr after KT. On the basis of our clinical experience, it is suggested that a long wait may not be necessary before KT in patients with ESRD and APL.
Active malignancy in end-stage renal disease (ESRD) patients is an absolute contraindication to kidney transplantation (KT) for several reasons (1). First, immune suppression contributes to the progression of cancer, which can significantly increase patient mortality (2). Indeed, the incidence of malignancy in KT recipients is 2-20-fold higher than that in the general population, depending on malignancy type (3). Second, early recurrence with associated morbidity and mortality would waste the transplanted kidney. Therefore, most guidelines recommend a 2-yr disease-free duration before KT (4).
Leukemia is a hematologic malignancy with a relatively lower incidence than solid tumors (5). Only a few reports have described KT after successful treatment of leukemia (6, 7). Therefore, no specific recommendations for the timing of KT in ESRD patients with leukemia are available. Instead, guidelines recommend a 2-yr waiting period after the complete remission (CR) of leukemia, as based on the guidelines for other types of malignancy (2, 8).
Acute leukemia comprises many subtypes, which show a highly variable clinical course. Of note, acute promyelocytic leukemia (APL), a form of acute myeloid leukemia (AML; M3), shows prominently favorable clinical outcomes compared to other types of AML. Therefore, the waiting period before KT after CR of APL may not need to be as long as that recommended for other types of leukemia in ESRD patients. However, no reports have described KT after APL treatment using arsenic trioxide (ATO). In this report, we describe successful living donor KT in a young man who experienced CR of APL, treated with ATO. Importantly, there has been no evidence of APL relapse up to 1 yr after transplantation.
In December 2009, a 23-yr-old man visited the Department of Emergency Medicine due to uncontrolled epistaxis, fatigue, and weight loss. He did not have a specific medical history of interest and specified that no abnormal findings were observed by blood chemistry analysis or urinalysis during a health check-up several months earlier. Laboratory analysis at presentation indicated coagulopathy with a prothrombin time (international normalized ratio) of 2.09, anemia, and thrombocytopenia with 46 × 109 platelets/L. White blood cell count was 6.5 × 109 cells/L and hemoglobin level was 12.7 g/dL. Blood urea nitrogen and serum creatinine (sCr) concentration was 21.6 mg/dL and 0.77 mg/dL, respectively. Lactate dehydrogenase level was 983 U/L, C-reactive protein 22.59 mg/dL, D-dimer 104 µg/mL, and fibrinogen 31 mg/dL, which was suggestive of severe disseminated intravascular coagulation (DIC). On the peripheral blood smear, leukocytes consisting of blasts (63%) and Auer rods were detected. All of these findings led us to suspect AML. We performed bone marrow (BM) biopsy, and APL was diagnosed based on the BM examination (Fig. 1). Cytogenetic molecular study using real-time quantitative polymerase chain reaction (RQ-PCR) showed a promyelocytic leukemia/retinoic acid receptor-α (PML-RARa) fusion transcript of 1.7 in the BM.
We initiated treatment for APL with daily all-trans retinoic acid (ATRA) (25 mg/[m2 · day]) administration and idarubicin (10 mg/day) administration on days 1 and 3. Three days after the initiation of treatment, sudden dyspnea developed and bilateral pulmonary infiltration was detected on chest Radiography. We performed intubation and initiated ventilator care. At this time, the patient's renal function abruptly deteriorated. BUN and sCr level increased to 99.6 mg/dL and 5.71 mg/dL, respectively, and urine volume decreased to 200 mL/day. We changed the patient's treatment regimen to ATO monotherapy (0.15 mg/[kg · day]) and initiated continuous renal replacement therapy (CRRT) for acute renal dysfunction.
At 17 days after the start of ATO treatment, the patient was successfully weaned off the ventilator, and his vital signs became stable. However, his renal function did not recover, and his anuric state persisted. We converted CRRT to hemodialysis, which was performed 3 times per week. The patient's general condition improved thereafter, and he was discharged on hospital day 35. During outpatient department follow-up, CR of APL was detected by BM biopsy findings, and RQ-PCR revealed a PML-RARa transcript of 0 at 3 months after the initiation of treatment.
After the achievement of CR, an additional 5 cycles of ATO chemotherapy (10 mg/day, each cycle lasting 10 days, per 30 or 45 days.) were administered. However, the patient still showed an anuric state and required maintenance hemodialysis therapy over the following 5 months. We performed kidney sonography to assess the reversibility of the observed renal dysfunction. Advanced chronic changes were detected, including decreased kidney size: right 8.4 × 4 × 3 cm, left 8.5 × 4 × 3 cm, lobulated contours, and increased parenchymal echogenicity (Fig. 2). Cortical parenchymal blood flow was markedly decreased on the color Doppler scan.
Up to 7 months after the achievement of CR, APL recurrence was not detected by BM study or cytogenetic molecular study. We therefore decided to perform KT using a kidney from the patient's younger sister. The HLA mismatch number was 2; the panel reactive antibody titer was 0%, and the cross-match test was negative. We administered triple immune suppressant therapy consisting of tacrolimus 4 mg (level, 3-7 ng/dL), mycophenolic acid 1,080 mg, and prednisolone 5 mg per day. After transplantation, the patient showed immediate allograft function. At 14 days after transplantation, sCr level fell from 10.26 mg/dL to 1.32 mg/dL. We performed protocol biopsy at 3 months after transplantation, which showed non-specific findings (Fig. 3). Up to 1 yr after KT, the patient's renal function has remained stable, and no evidence of APL recurrence has been detected by BM biopsy or molecular study performed at 1 yr after KT (Fig. 4).
In this report, we describe the successful management of a combined case of APL and ESRD in a young male patient. We initially performed chemotherapy to induce CR, and subsequently performed KT. This sequential approach enabled us to overcome both APL and ESRD in this patient without recurrence of APL or deterioration of allograft function. To the best of our knowledge, this is the first report of successful management in a patient with both APL and ESRD.
First, as in all patients, we had to evaluate whether continued dialysis or KT would be the most appropriate treatment strategy in this patient. We believed that KT would be better suited than dialysis, as this treatment option would allow us to perform autologous hematopoietic stem cell transplantation (HSCT) as a second-line therapy if APL recurred (9). In general, high-dose chemotherapy during HSCT is not available to patients with severe renal dysfunction (10). In addition, maintenance of hemodialysis during the neutropenic state of HSCT can increase the risk of fatal infection. In contrast, successful cases of BMT in kidney transplanted state without deterioration of renal function or severe infection have been reported (11, 12). Therefore, we elected to perform KT rather than continue dialysis treatment.
Next, we had to determine the most appropriate timing of KT. In general, it is recommended that KT in a patient with acute leukemia and ESRD be performed 2 yr after CR, based on existing guidelines for other types of malignancy. However, specific recommendations for such cases are currently unavailable, because only a few cases of combined acute leukemia and ESRD have been reported. Thus, before determining the timing of KT, we considered 3 factors, namely, CR, relapse, and risk factors. In APL, the CR and 3-yr disease-free survival rate is nearly 90%, which is significantly higher than that of other types of AML, at just 50% (13). Further, the relapse rate of APL within 2 yr after CR is only 6%, which is significantly lower than that of other types of AML (14). Thus, APL differs from other types of AML in that it is associated with a high CR rate and low relapse rate. The present patient also could be categorized into the low-risk group based on traditional risk factors such as age, performance status, and gene study (14), as well as the newly recommended risk model for APL based on WBC and platelet counts; in patients with similar WBC and platelet counts to those observed in our patient, the relapse rate has been reported to be nearly 0% over more than 5 yr (15). Therefore, we performed KT earlier than recommended (7 months after CR), because the risk of APL recurrence was thought to be extremely low in this patient.
Another important consideration in this case was the reversibility of the observed kidney dysfunction, because this patient was a young man without underlying renal disease. The cause of ESRD in this patient was unclear, but acute kidney injury may have resulted from massive cortical necrosis due to severe DIC combined with acute ATRA syndrome, which then progressed to ESRD. The patient's anuric state was sustained until KT, for almost 9 months, and ultrasonography showed advanced chronic changes in the kidney. These findings indicated that irreversible kidney injury had developed in this patient, thus necessitating KT.
We observed the present patient for nearly 2 yr, including the careful monitoring of APL relapse. The incidence of leukemia is highest in the first year after transplantation, where after it shows a decreasing pattern, in contrast to other malignancies, which show an increasing incidence with time after transplantation (5). Moreover, the incidence of de novo APL in renal transplant recipients is extremely low. Only 3 patients presenting with new-onset APL following KT have been reported in the past 3 decades (16, 17). The above findings suggest that the risk of APL relapse in this patient is likely to be very low, as no signs of relapse were observed up to 1 yr after KT.
In conclusion, this is the first report of successful KT after CR of APL. This case suggests that KT can be considered in ESRD patients with APL without a lengthy period of waiting. However, accumulation of more cases of a similar nature may be required before definite conclusions can be made.
Figures and Tables
Fig. 1
Bone marrow aspiration finding (Wright's stain, × 1,000). Abnormal promyelocytes with prominent cytoplasmic granules were found. It is consistent with acute promyelocytic leukemia.
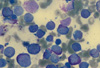
Fig. 2
Kidney ultrasonography finding. Before transplantation, ultrasonography showed decreased kidney size (right 8.4 × 4 × 3 cm, left 8.5 × 4 × 3 cm) and lobulated contour and increased parenchymal echogenicity (arrow). Above finding suggest the advanced chronic change of kidney.
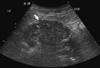
Fig. 3
Protocol allograft biopsy finding (H&E stain, × 100). Protocol biopsy performed at 3 months after transplantation showed non-specific findings without tubulitis or interstitial infiltration.
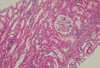
Fig. 4
Clinical course of the patient. CR was achieved at 3 months after the initiation of treatment. Bone marrow biopsy was done total 6 times, four was done first every month after CR and the last biopsy was performed at 17 month after CR, there is no evidence of relapse. Until 9 months from the start of hemodialysis, renal function did not recover and KT was performed. After KT, renal function was normalized immediately, and patient's clinical course was stable until last follow up (2 yr). He is taking triple immune suppressant; tacrolimus, mycophenolic acid, prednisolone. CRRT, continuous renal replacement therapy; HD, hemodialysis; KT, kidney transplantation; CR, complete remission; RQ-PCR, Real-time quantitative polymerase chain reaction; BM biopsy, bone marrow biopsy; Tac, Tacrolimus; MMF, mycophenolic acid.

References
1. Brenner BM, Rector FC. Brenner and Rector's the kidney. 2004. 7th ed. Philadelphia: Saunders;2.
2. Collins AJ, Kasiske B, Herzog C, Chavers B, Foley R, Gilbertson D, Grimm R, Liu J, Louis T, Manning W, et al. Excerpts from the United States Renal Data System 2004 annual data report: atlas of end-stage renal disease in the United States. Am J Kidney Dis. 2005. 45:A5–A7. S1–S280.
3. Rama I, Grinyó JM. Malignancy after renal transplantation: the role of immunosuppression. Nat Rev Nephrol. 2010. 6:511–519.
4. Kasiske BL, Cangro CB, Hariharan S, Hricik DE, Kerman RH, Roth D, Rush DN, Vazquez MA, Weir MR. American Society of Transplantation. The evaluation of renal transplantation candidate: clinical practice guideline. Am J Transplant. 2001. 1:3–95.
5. Kasiske BL, Snyder JJ, Gilbertson DT, Wang C. Cancer after kidney transplantation in the United States. Am J Transplant. 2004. 4:905–913.
6. Sayegh MH, Fine NA, Smith JL, Rennke HG, Milford EL, Tilney NL. Immunologic tolerance to renal allografts after bone marrow transplants from the same donors. Ann Intern Med. 1991. 114:954–955.
7. Helg C, Chapuis B, Bolle JF, Morel P, Salomon D, Roux E, Antonioli V, Jeannet M, Leski M. Renal transplantation without immunosuppression in a host with tolerance induced by allogeneic bone marrow transplantation. Transplantation. 1994. 58:1420–1422.
8. EBPG (European Expert Group on Renal Transplantation). European Renal Association (ERA-EDTA). European Society for Organ Transplantation (ESOT). European Best Practice Guideline for Renal Transplantation (part 1). Nephrol Dial Transplant. 2000. 15:1–85.
9. National Comprehensive Cancer Network ® (NCCN®). NCCN Guidelines version 2. 2011 Acute myeloid leukemia. 2011. 53.
10. Niscola P, Vischini G, Tendas A, Scaramucci L, Giovannini M, Bondanini F, Romani C, Brunetti GA, Cartoni C, Cupelli L, et al. Management of hematological malignancies in patients affected by renal failure. Expert Rev Anticancer Ther. 2011. 11:415–432.
11. Vesole DH, Jagannath S. Transplants from the same donor. Ann Intern Med. 1992. 116:269–270.
12. Gajewski JL, Ippoliti C, Ma Y, Champlin R. Discontinuation of immunosuppression for prevention of kidney graft rejection after receiving a bone marrow transplant from the same HLA identical sibling donor. Am J Hematol. 2002. 71:311–313.
13. Hoffman R, Furie B, Benz EJ Jr, McGlave P, Silberstein LE, Shattil SJ. Hematology: basic principles and practice. 2008. 5th ed. Philadelphia: Churchill Livingstone.
14. Soignet SL, Peter G. Wintrobe's clinical hematology. 2009. 12th ed. Philadelphia: Lippincott Williams & Wilkins.
15. Sanz MA, Lo Coco F, Martin G, Avvisati G, Rayón C, Barbui T, Díaz-Mediavilla J, Fioritoni G, González JD, Liso V, et al. Definition of relapse risk and role of nonanthracycline drugs for consolidation in patients with acute promyelocytic leukemia: a joint study of the PETHEMA and GIMEMA cooperative groups. Blood. 2000. 96:1247–1253.
16. Specchia G, Storlazzi CT, Cuneo A, Surace C, Mestice A, Pannunzio A, Rocchi M, Liso V. Acute promyelocytic leukemia with additional chromosome abnormalities in a renal transplant case. Ann Hematol. 2001. 80:246–250.
17. Lai CP, Chang CC, Chung CY, Chen ML. Unusual acute promyelocytic leukemia following de novo renal transplant: case report and literature review. Clin Nephrol. 2011. 75:27–31.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download