Abstract
We evaluated the prevalence and risk factors for early age-related macular degeneration (AMD) in Koreans 50 yr of age or older who were examined at a single health promotion center. We retrospectively reviewed the records of 10,449 subjects who visited the center over a 6-month period. Fundus photography was performed on all subjects, and systematic risk factor analysis was conducted using a structured questionnaire. All patients (n = 322) were initially diagnosed with drusen or early AMD using fundoscopy; the control group (n = 10,127) were those yielding normal fundoscopy findings. The age- and gender-adjusted prevalence of early AMD was 3.08%. Advanced age, male gender, smoking status, hyperlipidemia, working outdoors, and residence in rural areas were all significantly associated with an increased risk for development of early AMD. Higher-level ingestion of fruit or herbal medication and an increased amount of exercise were associated with a lower risk of early AMD development. In our Korean cohort, consisting principally of relatively healthy, middle-class urban adults, the prevalence of early AMD was 3.08% that is similar to that reported in earlier epidemiological studies. Several modifiable risk factors such as smoking and hyperlipidemia are associated with the prevalence of early AMD in our cohort.
Age-related macular degeneration (AMD) is the main cause of blindness in elderly patients in the USA and Asia (1, 2). Numerous large-scale population-based studies have described the prevalence of and possible risk factors for AMD, but the results have not been in full agreement (3, 4). Several such studies found that the prevalence of late-stage AMD was lower in Asians than in Caucasians (5), but that the frequency of polypoidal choroidal vasculopathy (PCV) was higher in Asians (6-8). Western population-based studies of the age distribution of AMD patients have estimated the disease prevalence as 4%-12%, depending on age (9-11). Asian population-based studies have yielded differing results; the Beijing Eye Study (5) and the Hisayama study (6) reported a lower prevalence of AMD in Asians. The Shiphai study (12), which detected early AMD in 9.2% of subjects and late-stage disease in 1.9%, found that disease prevalence was similar in Asians and Westerners. In India, the prevalence of AMD has been estimated as 2%-4.6% (7, 8). An earlier Korean population-based study found that the prevalence of early AMD was 5% and that of late-stage disease 0.34% (13).
Many previous reports have identified cardiovascular, genetic, and environmental risk factors for development of AMD (3, 4). Numerous studies have reported that smoking is an environmental risk factor for disease development (14-17). However, Asian population-based studies have found that the relationship between smoking status and AMD was equivocal. The Beijing Eye Study and the Screened Korean population-based study reported that smoking status was not associated with development of AMD (5, 13). Some reports have found relationships between AMD development and cardiovascular risk factors including hypertension, obesity, and hyperlipidemia, but other studies reported no such relationships. Additional environmental risk factors have been identified in different populations (18, 19).
A recent study reported the prevalence of and risk factors for AMD in Korea; the results were somewhat different from other Asian research data (13). In the present work, we determined the prevalence of and risk factors for development of early AMD in Koreans 50 yr of age or older who were examined at a single health promotion center.
The present work was a population-based cross-sectional study of Korean subjects 50 yr of age or older who were examined at the health promotion facility of the Asan Medical Center (University of Ulsan College of Medicine, Seoul, Korea). About 40,000 subjects present for health screening in any given year. Between January and June 2010, 20,112 examinees attended, and 10,449 of those who were at least 50 yr of age were initially enrolled in the present study.
Several fundus photographs, including images taken at 45-degree angles, were obtained using a nonmydriatic digital fundus camera (CR6-45NM; Canon Inc., Tokyo, Japan). All images were stored in an archiving communication system (PACS PiView-STAR; INFINITT, Seoul, Korea) and were interpreted by three screening ophthalmologists. All diagnoses were confirmed by a retinal specialist. Patients in whom early AMD was suspected were classified using the criteria of the International Age-Related Maculopathy (ARM) Epidemiological Study Group (20).
Drusen were classified based on size and the degree of edge sharpness. Drusen of diameter greater than 63 µm were considered to be "soft drusen" and were further graded as "distinct" or "indistinct". Hypo- or hyper-pigmentation of the retinal pigment epithelium (RPE) was considered to be an RPE abnormality. Early AMD was diagnosed based on the presence of: 1) soft distinct drusen; or 2) soft indistinct drusen; or 3) RPE abnormalities (atrophy, or hypo- or hyper-pigmentation); or 4) when both drusen and an RPE abnormality were present. Patients with late AMD, featuring neovascular disease or geographic atrophy, were excluded from the study.
All participants completed a questionnaire and laboratory tests were used to identify cardiovascular risk factors. The confidential questionnaire collected relevant socio-demographic and medical information.
Questions on diet assessed the daily intake of vegetables, animal cholesterol, fatty foods, and fruit. Participants were classified as current smokers, past smokers, or never- smokers. Pack-years of smoking could not be calculated because the reported data were variable. Heavy smoking was defined as the smoking of one or more packs of cigarettes daily. The level of alcohol consumption per week was assessed. The frequency and amount of exercise taken were also recorded. Occupation was classified as indoors or outdoors in nature and residence as urban or rural. Present and past medical conditions including hypertension (HTN), angina, diabetes mellitus, and any history of myocardial infarction (MI) or stroke, were recorded. A medication history, including the use of blood pressure (BP)-lowering agents, antidiabetic drugs, female hormones, calcium and/or vitamin supplements, aspirin, warfarin, and any herbal medication, was recorded for each subject. Any family history of cardiovascular disease was noted.
Systolic and diastolic BP, body mass index (BMI), and waist circumference were measured. Laboratory tests assessed the levels of fasting blood glucose (FBG); hemoglobin A1c (HbA1c); and lipids (total cholesterol, triglycerides [TG], high-density lipoprotein [HDL] cholesterol, and low-density lipoprotein [LDL] cholesterol).
SPSS version 17.0 (SPSS Inc., Chicago, IL, USA) was used for all statistical analyses. Categorical variables were examined via calculation of odds ratios (ORs) with 95% confidence intervals (CIs) using binary logistic regression analysis (crude, and age- and gender-adjusted). After univariate logistic analysis was complete, multivariable logistic regression analysis was performed to identify independent risk factors. A P value less than 0.05 was considered significant.
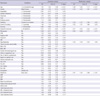
Our study population consisted of 10,449 subjects, 332 (3.08%) of whom were diagnosed with early AMD. Table 1 summarizes the characteristics of the fundus lesions of patients with early AMD. A total of 240 patients (74.5%) had soft distinct drusen; 40 (12.4%) soft indistinct drusen; 33 (10.2%) an RPE abnormality (atrophy, or hypo- or hyper-pigmentation); and 9 (2.8%) AMD of the mixed type. A total of 229 patients (71.2%) showed abnormalities in an extramacular area or in the peripheral retina, whereas 93 (28.8%) had abnormalities in the macular or paramacular area. A total of 230 patients (71.4%) had bilateral AMD and 92 (28.6%) unilateral disease. Bilateral extramacular AMD with soft distinct drusen was the most common disease manifestation. A total of 23 patients (7.1%) had previously undergone ocular surgery.
The mean uncorrected distant visual acuity (LogMAR value) was 0.19 ± 0.23/0.19 ± 0.24 (right/left eye) in the early AMD group and 0.15 ± 0.22/0.16 ± 0.21 in the control group. Average intraocular pressure, as determined by noncontact tonometry, was 12.34 ± 3.07/12.20 ± 2.4 mmHg in the early AMD group and 12.50 ± 3.01/12.30 ± 2.62 mmHg in the control group.
Table 2 lists the risk factors for development of early AMD. Age- and gender-adjusted binary logistic regression analysis indicated that disease status was positively associated with advanced age, male gender, smoking status, level of smoking, hyperlipidemia, working outdoors, and rural residence. Elevated fruit intake, frequent exercise, and use of herbal medications were negatively associated with development of early AMD.
Some initially identified factors were found to yield insignificant correlations with disease status when the data were adjusted in terms of age and gender (Table 2). Multiple logistic regression analysis employing a backward elimination method indicated that advanced age, male gender, smoking status, level of smoking, the amount of exercise taken, hyperlipidemia, and rural residence, were all independently associated with development of early AMD in our study population.
In the present retrospective population-based study, we evaluated the prevalence and type of, and risk factors for, development of early AMD in a relatively healthy, middle-aged, middle-class urban population of Koreans. In Korea, large numbers of the general population visited health promotion centers for regular screening examinations. The health promotion center of the Asan Medical Center services about 40,000 clients each year and evaluated 10,449 subjects 50 yr of age or older between January and June 2010. About 60% of all subjects lived in the city of Seoul, about 25% in other urban areas, and about 15% in rural areas. Occupational analysis indicated that only 3%-4% of participants had outdoor jobs (as farmers, fishermen, mine workers, or laborers). About 80% of subjects had graduated from high school and some were university-educated. Analysis of family income levels indicated that 95% of men and 72% of women were middle-class. Thus, we would classify our study population as middle-aged, middle-class, relatively healthy, urban Koreans.
The age- and gender-adjusted prevalence of early AMD in the present study was 3.08%, similar to that reported in other Asian populations. Western population-based studies have found that the prevalence of AMD was 4%-12%. And work with Asian populations, the prevalence of AMD was variable about 2%-12%. An earlier Korean population-based study reported that the prevalence of early AMD was 5% and that of late-stage disease was 0.34% (13). The lower prevalence of early AMD in our subjects relative to that in Western populations (11) may be attributable to genetic and/or environmental factors.
Bilateral, soft, distinct extramacular or peripheral drusen were the most common feature of early AMD in our study population. Both the mean uncorrected visual acuity and intraocular pressure were within normal ranges in all of our subjects, and did not significantly differ between those with early AMD and controls. Also, a prior history of ocular surgery was not significantly associated with development of early AMD. In the risk factor analysis, advanced age was significantly associated with early AMD; the odds ratio for each incremental year of age was 1.06. Previous work also indicated that age was the most important risk factor for development of AMD (13). Subjects 70 yr of age or older are less likely to proactively visit health promotion centers; we thus recommend that all older subjects be encouraged, by family members or doctors, to undergo regular fundoscopic examinations.
Many studies have found that cigarette smoking is a major risk factor for development of AMD and increases both prevalence and rate of progression of the disease by elevating the level of oxidative stress in the retina and choroid, decreasing the extent of luteal pigment in the retina, activating the immune system, reducing choroidal blood flow, and causing micro-infarctions (14-17). In the present study, we also found a strong positive relationship between cigarette smoking and AMD development, in line with data from prior epidemiological work.
On multivariable analysis, a history of hyperlipidemia was associated with development of early AMD. However, serum lipid data, including the levels of HDL and LDL cholesterol, and TG concentration, were not significantly associated with development of early AMD. It is nonetheless possible that a prior history of lipidemia may have contributed to development of disease, even though all of our patients yielded good lipid profiles at the time of testing for the present study.
Some reports have indicated that outdoor activity and exposure to ultraviolet radiation were associated with the development of drusen and other types of AMD (19, 21). In the present study, working outdoors and residence in a rural area, which presumably result in greater exposure to ultraviolet radiation, were positively associated with development of early AMD, in agreement with the data of previous studies.
Surprisingly, the level of fruit intake was inversely related to development of early AMD in our study population. The Age-Related Eye Disease Study (AREDS) recommended that vitamins A, C, and E should be prescribed for prevention of AMD (22). Such vitamins, present in fruit, presumably stabilize the RPE via protection against oxidative stress.
No previous study has examined a possible association between the level of physical activity and AMD. In our present work, age- and gender-adjusted multivariable regression analysis indicated that the amount and duration of exercise were inversely associated with early AMD. The mechanism underlying this association remains unclear. Further work is needed to identify the types of exercise that protect against development AMD and the reasons why this is so.
We also found that use of herbal medications was inversely associated with early AMD. This finding cannot be readily explained. It is possible that the observed association is spurious, because many different risk factors were explored. However, we suggest that further study of a possible association between use of herbal medications and inhibition of development of early AMD is warranted.
Several previous works found that obesity and cardiovascular disease were both risk factors for AMD, especially late-stage disease (23). In the present study, we found no significant association between cardiovascular risk factors (diabetes mellitus, HTN, angina, or stroke) and early AMD.
Our study had several limitations. First, the work was retrospective in nature, and sample selection bias was thus possible. Second, patients with late AMD, such as those with geographic atrophy, or patients with exudative (wet) AMD, were less likely included in our study. As individuals visiting our health promotion center were relatively-healthy, middle-aged, urban Koreans, visual acuity of our study population was mostly within normal range. Thus, we cannot calculate the overall prevalence of AMD; this is a limitation of our risk factor analysis. Further studies are needed to identify the prevalence of and risk factors for development of both early- and late-stage disease. Third, patients for whom fundus photographs were of poor quality were excluded, possibly biasing our estimate of the prevalence of early AMD. Finally, cataract status and refractive error data were not available for all subjects. The conduct of a prospective, population-based study that collects complete ophthalmologic data from Asians would overcome most of these limitations.
In conclusion, our study of relatively healthy, middle-aged, middle-class urban Koreans who were normal in terms of both visual acuity and intraocular pressure indicated that the prevalence of early AMD (3.08%) was comparable to that found in other studies of Asian populations. Our results indicate that age, male gender, smoking status, a low level of exercise, any history of hyperlipidemia, working outdoors, and rural residence, are all (positively) associated with the development of early AMD. Control of the risk factors can reduce the prevalence of early AMD. Risk factors that are identified in our study are similar to those of general age-related health problem. Therefore, general health care and regular eye examination are needed especially in middle-age and elderly persons.
Figures and Tables
References
1. Pascolini D, Mariotti SP, Pokharel GP, Pararajasegaram R, Etya'ale D, Négrel AD, Resnikoff S. 2002 global update of available data on visual impairment: a compilation of population-based prevalence studies. Ophthalmic Epidemiol. 2004. 11:67–115.
2. Wong TY, Loon SC, Saw SM. The epidemiology of age related eye diseases in Asia. Br J Ophthalmol. 2006. 90:506–511.
3. Morris B, Imrie F, Armbrecht AM, Dhillon B. Age-related macular degeneration and recent developments: new hope for old eyes? Postgrad Med J. 2007. 83:301–307.
4. Haines JL, Hauser MA, Schmidt S, Scott WK, Olson LM, Gallins P, Spencer KL, Kwan SY, Noureddine M, Gilbert JR, et al. Complement factor H varant increases the risk of age-related macular degeneration. Science. 2005. 308:419–421.
5. Li Y, Xu L, Jonas JB, Yang H, Ma Y, Li J. Prevalence of age-related maculopathy in the adult population in China: the Beijing eye study. Am J Ophthalmol. 2006. 142:788–793.
6. Oshima Y, Ishibashi T, Murata T, Tahara Y, Kiyohara Y, Kubota T. Prevalence of age related maculopathy in a representative Japanese population: the Hisayama study. Br J Ophthalmol. 2001. 85:1153–1157.
7. Nirmalan PK, Katz J, Robin AL, Tielsch JM, Namperumalsamy P, Kim R, Narendran V, Ramakrishnan R, Krishnadas R, Thulasiraj RD, et al. Prevalence of vitreoretinal disorders in a rural population of southern India: the Aravind Comprehensive Eye Study. Arch Ophthalmol. 2004. 122:581–586.
8. Gupta SK, Murthy GV, Morrison N, Price GM, Dherani M, John N, Fletcher AE, Chakravarthy U. Prevalence of early and late age-related macular degeneration in a rural population in northern India: the INDEYE feasibility study. Invest Ophthalmol Vis Sci. 2007. 48:1007–1011.
9. Klein R, Klein BE, Linton KL. Prevalence of age-related maculopathy. The Beaver Dam Eye Study. Ophthalmology. 1992. 99:933–943.
10. Mitchell P, Smith W, Attebo K, Wang JJ. Prevalence of age-related maculopathy in Australia. The Blue Mountains Eye Study. Ophthalmology. 1995. 102:1450–1460.
11. Augood CA, Vingerling JR, de Jong PT, Chakravarthy U, Seland J, Soubrane G, Tomazzoli L, Topouzis F, Bentham G, Rahu M, et al. Prevalence of age-related maculopathy in older Europeans: the European Eye Study (EUREYE). Arch Ophthalmol. 2006. 124:529–535.
12. Chen SJ, Cheng CY, Peng KL, Li AF, Hsu WM, Liu JH, Chou P. Prevalence and associated risk factors of age-related macular degeneration in an elderly Chinese population in Taiwan: the Shihpai Eye Study. Invest Ophthalmol Vis Sci. 2008. 49:3126–3133.
13. Song SJ, Youm DJ, Chang Y, Yu HG. Age-related macular degeneration in a screened South Korean population: prevalence, risk factors, and subtypes. Ophthalmic Epidemiol. 2009. 16:304–310.
14. Cohen SY, Creuzot-Garcher C, Darmon J, Desmettre T, Korobelnik JF, Levrat F, Quentel G, Paliès S, Sanchez A, de Gendre AS, et al. Types of choroidal neovascularisation in newly diagnosed exudative age-related macular degeneration. Br J Ophthalmol. 2007. 91:1173–1176.
15. Tomany SC, Wang JJ, Van Leeuwen R, Klein R, Mitchell P, Vingerling JR, Klein BE, Smith W, De Jong PT. Risk factors for incident age-related macular degeneration: pooled findings from 3 continents. Ophthalmology. 2004. 111:1280–1287.
16. Klein R, Knudtson MD, Cruickshanks KJ, Klein BE. Further observations on the association between smoking and the long-term incidence and progression of age-related macular degeneration: the Beaver Dam Eye Study. Arch Ophthalmol. 2008. 126:115–121.
17. Fraser-Bell S, Wu J, Klein R, Azen SP, Varma R. Smoking, alcohol intake, estrogen use, and age-related macular degeneration in Latinos: the Los Angeles Latino Eye Study. Am J Ophthalmol. 2006. 141:79–87.
18. Klein R, Klein BE, Moss SE. Relation of smoking to the incidence of age-related maculopathy. The Beaver Dam Eye Study. Am J Epidemiol. 1998. 147:103–110.
19. Kernt M, Hirneiss C, Neubauer AS, Lackerbauer CA, Eibl KH, Wolf A, Ulbig M, Kampik A. Protective effect of blue light-absorbing IOLs on the human retinal pigment epithelium. Ophthalmologe. 2010. 107:150–157.
20. Bird AC, Bressler NM, Bressler SB, Chisholm IH, Coscas G, Davis MD, de Jong PT, Klaver CC, Klein BE, Klein R, et al. An international classification and grading system for age-related maculopathy and age-related macular degeneration. The International ARM Epidemiological Study Group. Surv Ophthalmol. 1995. 39:367–374.
21. Pham TQ, Rochtchina E, Mitchell P, Smith W, Wang JJ. Sunlight-related factors and the 10-year incidence of age-related maculopathy. Ophthalmic Epidemiol. 2009. 16:136–141.
22. SanGiovanni JP, Chew EY, Clemons TE, Ferris FL 3rd, Gensler G, Lindblad AS, Milton RC, Seddon JM, Sperduto RD. The relationship of dietary carotenoid and vitamin A, E, and C intake with age-related macular degeneration in a case-control study: AREDS Report No. 22. Arch Ophthalmol. 2007. 125:1225–1232.
23. Liu Y, Wen F, Huang S, Luo G, Yan H, Sun Z, Wu D. Subtype lesions of neovascular age-related macular degeneration in Chinese patients. Graefes Arch Clin Exp Ophthalmol. 2007. 245:1441–1445.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download