Abstract
The diagnostic accuracy of the data reported in the Korean tuberculosis surveillance system (KTBS) has not been adequately investigated. We reviewed the clinical data of pulmonary tuberculosis (PTB) cases notified from private medical facilities through KTBS between January and June, 2004. PTB cases were classified into definite (culture-proven), probable (based on smear, polymerase chain reaction, histology, bronchoscopic finding, computed tomography, or both chest radiograph and symptoms) or possible (based only on chest radiograph) tuberculosis. Of the 1126 PTB cases, sputum AFB smear and culture were requested in 79% and 51% of the cases, respectively. Positive results of sputum smear and culture were obtained in 43% and 29% of all the patients, respectively. A total of 73.2% of the notified PTB cases could be classified as definite or probable and 81.7% as definite, probable, or possible. However, where infection was not confirmed bacteriologically or histologically, only 60.1% of the patients were definite, probable, or possible cases. More than 70% of PTB notified from private sectors in Korea can be regarded as real TB. The results may also suggest the possibility of over-estimation of TB burden in the use of the notification-based TB data.
Tuberculosis (TB) still remains a huge health burden worldwide. The World Health Organization (WHO) estimated that 9.3 million new cases and 1.7 million deaths by TB occurred in 2007 globally, based on data provided by individual countries including Korea (1, 2). Korea has evaluated the burden of TB using several methods. From 1965 to 1995, the Korean National Tuberculosis Association conducted seven nationwide TB prevalence surveys at five-year intervals (3, 4) which provided useful information identifying the status and trends of TB in Korea. However, the nationwide surveys had limitations: for example, as TB prevalence rate decreased, the sample size required for a survey increased, which led to a higher cost. Thus, a web-based surveillance system named as the Korean TB surveillance system (KTBS) based on notification launched in 2000 and has been implemented across the country in place of additional nationwide surveys (5).
By Korean TB Prevention Law, physicians in both public and private sector making or suspecting the diagnosis of TB are legally responsible for notification, and these notified data are collected in KTBS. The Korean government reported the incidence rate based on the KTBS data. As a result, the number of TB cases reported from the private sector were included in the national figure for the first time (6). Although KTBS is a simple way to collect and analyze massive data on the TB burden in Korea, evaluating the accuracy of data from KTB S is essential (7). However, there have been concerns on the completeness and the accuracy of the data especially from private sectors. First, there are possibilities of missed notifications, which can result in an underestimation of TB burden (7-13). On the contrary, a question whether a 'notified TB' case is a 'real TB' can also be raised. Some notified cases as TB might not be real TB cases, which can lead to overestimating the TB burden. In fact, a study reported that the concordance rate between notified TB reports and medical records of 'sputum culture examination' was lower than expected (23%) in one private general hospital in Korea (14). However, there have been no comprehensive analyses on the diagnostic accuracy of the notified cases as pulmonary tuberculosis (PTB) of private sectors in Korea.
The aim of our study was to estimate the diagnostic accuracy in pulmonary TB patients notified from private sectors of Korea by analyzing the randomly sampled notified cases with a sensitive analysis.
For disease surveillance, the diagnosis of TB was standardized on the basis of laboratory and/or clinical evidence of active disease due to the Mycobacterium tuberculosis complex. The WHO/IUATLD case definitions were used in both the public and private sectors. A definite tuberculosis case is culture positive case for M. tuberculosis complex (15). Notification was conducted by the standard nationwide surveillance systems (KTBS) which was supervised by the Korea Centers for Disease Control and Prevention. The TB notification form included case characteristics, history of previous treatment, history of BCG vaccination, examinations for diagnosis (such as sputum smear or culture, histologic and radiological examinations, tuberculin skin test), site of tuberculosis by International Classification of Disease-10 (ICD-10) code and treatment information (16).
A total of 20,652 patients were reported as 'new' TB cases from private sectors of Korea in 2004. Among the 10,160 notified new tuberculosis cases during the first half of 2004, 1,530 cases from 488 private medical facilities were randomly selected by stratified proportional to size sampling by region and classification (general hospital, hospital, clinic). After the selection, medical records of TB patients treated at private sector during that period were collected by requesting the selected medical facilities to send copies of medical records and to complete a questionnaire between December 2005 and January 2006. The questionnaire included demographics, types of TB by site, history of treatment, ICD-10 code, results of initial and follow up chest radiographs, results of sputum smear and culture examinations for diagnosis, the date of diagnosis or treatment, and the initial treatment regimen. After collecting requested medical records and additional questionnaire from each relevant private sector, reinforcement work has been performed by health workers in the public health centers or co-workers of this study. All of the collected data were transferred to and organized at the Korea Institute of Tuberculosis (KIT). The cases that were notified as PTB were included in the study. Of the 1,530 randomly selected patients, the cases without the ICD-10 code at notification (cases lacking clinical information or cases other than TB), the cases with A17-A18 (extrapulmonary TB only), the cases with A19 (miliary TB), the cases with A15.4 or A16.3 (mediastinal TB lymphadenitis only), and the cases with A15.6 or A16.5 (TB pleurisy only) were excluded. A total of 1,126 PTB cases remained for further analysis. To assess the completeness of notifications, laboratory data including initial chest radiographs and follow-up chest radiographs after the initiation of anti-TB treatment as well as clinical symptoms at diagnosis were also examined.
All the cases were reclassified into nine categories using clinical, laboratory, or radiologic data (1, 14): 'definite TB' cases (category 1, acid-fast bacilli [AFB] culture positive); 'probable TB' cases (category 2, smear positive; category 3, TB PCR positive; category 4, histopathologically diagnosed; category 5, bronchoscopically positive, i.e. compatible with endobronchial tuberculosis; category 6, radiographically active TB on chest CT examination; category 7, active TB on initial simple chest radiographs with symptoms for more than two weeks or 'possible TB' cases for more sensitive inclusion (category 8, active TB on initial simple chest radiograph other than category 7; category 9, radiographical improvement with anti-TB treatment). 'Radiographically active TB' was defined as cases with multinodular lesions, miliary nodules, cavity or airspace consolidation. Calcified or fibrotic lesions were excluded. The reports provided by the radiologist at each applicable hospital were used. Lastly 'improvement of follow-up chest radiograph' was defined as reduction of lesions after at least one month of anti-TB medication.
The 95% confidence intervals of each class of the notified cases were estimated by calculating the ratio (p), the total number of cases (n) divided by the number of each case, ± 1.96 × √{p (1-p)/n}. Statistical analyses were performed using the SPSS version 12.0 (SPSS Inc, Chicago, IL, USA) and STATA Version 11.1 (StataCorp., College Station, TX, USA).
Of the 1,530 randomly selected cases, 404 cases were excluded: 219 cases were missing the ICD-10 code at notification (cases lacking of clinical information or cases other than TB), 86 cases were A17-A18 (extrapulmonary TB only), 7 cases were A19 (miliary TB), 9 cases were A15.4 or A16.3 (mediastinal TB lymphadenitis only), 83 cases were A15.6 or A16.5 (TB pleurisy only).
A total of 1,126 PTB patients from private sectors was included in the analysis as described above. The median age was 45 yr (range 2-96) and 60.6% of the patients were male. Baseline characteristics including type of cases, type of tuberculosis, ICD-10 code, clinical symptoms are summarized in Table 1. Six hundred and thirty-two (56.1%) patients were notified as laboratory diagnosed TB cases (A15), and 74.3% of them were symptomatic with cough and sputum being the most common symptoms.
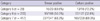
Laboratory tests for the diagnosis of PTB performed in private sector are listed in Table 2. Sputum AFB smear was performed in approximately 80% of the patients and 42.5% of the notified PTB cases were smear positive. Sputum M. tuberculosis culture was verified in approximately half of the patients (51%) and 29% of the total patients were M. tuberculosis culture positive. PCR (14.3%) or biopsy (3.6%) were performed in a relatively small number of PTB patients. Fifty-seven patients (5.1%) were examined bronchoscopically and 49% (28 cases) showed positive results (e.g. active caseating inflammation). Chest CT was performed in about a quarter of patients and a high positive result (83.5%) was reported. A simple chest radiograph was performed in the majority of the patients (71.1%) and 'radiographically active PTB' lesions were reported in 77%. The most commonly involved site of the lung was right upper lung field (31.7%). The left upper lung field was the next most commonly involved site (27.7%). A follow-up radiologic examination at least one month after the initiation of anti-TB medication was assessed in 454 patients and 77.5% showed radiologic improvement. When the utilization of the diagnostic modalities by private sector scale was analyzed, the performance rates of all the diagnostic methods including AFB smear and culture, TB PCR, bronchoscopy, chest radiography and chest CT were lower in primary clinic compared to those of secondary and tertiary hospitals (Table 2). Definite TB, categorized as a M. tuberculosis complex culture positive case, was observed in 28.9% (95% CI, 26.3%-31.5%) of the total patients. When the diagnostic criteria of TB was extended according to the proposed classification, definite and probable TB combined was 73.2% (95% CI, 70.6%-75.8%); and definite, probable, and possible TB combined was 81.7% (95% CI, 79.4%-84.0%) (Table 3). A detailed microbiological information of categories 5, 6, 7 is summarized in Table 4. When the analyses were limited to the patients who were notified as presumptive TB patients (PTB not confirmed bacteriologically or histologically; A16), definite case was observed in only one patient. Definite and probable TB cases were observed in 41.7% (95% CI, 37.4%-46.0%); and definite, probable, and possible TB cases were 60.1% (95% CI, 55.8%-64.4%) of the total patients, respectively (Table 5).
A total of 206 cases did not meet the criteria of the proposed categories 1-9. Of these, 143 cases were treated with anti-TB medication for less than 30 days, 21 cases for 30 to 90 days, and 42 cases for longer than 90 days (34 patients were treated for longer than six months).
In this study, definite TB cases confirmed by culture of M. tuberculosis complex (category 1, the current gold standard of diagnosis of TB) were only 28.9% (95% CI, 26.3%-31.5%) of the total cases. The percentage of definite cases or bacteriologically, pathologically or bronchoscopically probable TB cases (category 2-5) were 55.7% (95% CI, 52.8%-58.6%) of the total cases, and if radiographically positive TB cases (category 6-7) are also included, the percentage of the "definite or probable TB" cases became 73.2% of the total cases.
When possible cases were regarded as real TB (category 1-9), still the percentage of real TB was 81.7% (95% CI, 79.4%-84.0%), not 100%. Due to the nature of a retrospective study, the limitations concerning a lack of sufficient information despite an extensive review of the medical records is encountered. The definite number of cases that were not real TB among cases not included in Category 1-9 could not be determined. Therefore, the results should not be interpreted directly as 'only 81.7% of the notified new PTB patients had real PTB' or 'approximately 20% of the notified new PTB patients did not have TB'. However, the study suggests that some cases notified as PTB might not be real TB. In fact, 69% of 206 cases that were not included in categories 1-9 were treated with anti-TB medication for less than one month, which suggests that some may be cases with other than PTB, such as pneumonia. So far, most reports focused on underestimation of TB by the notification system and emphasized the importance of notification (10, 17, 18). On the contrary, this study may suggests the possibility of overestimation of tuberculosis.
It is possible that the microbiological tests are not performed sufficiently when physicians diagnose a case as PTB in Korea, which could lead to overdiagnosis. Although WHO recommends that patients suspected of having TB should have appropriate specimens collected for smear and culture for M. tuberculosis (19), smear-positive patients were 42.5% among the new PTB cases in our study, which is lower to some degree than that of global epidemiology data that showed smear-positive rate of approximately 57% in 2008 (1). It may be due to the fact that sputum test is less requested in Korea than in other countries in substantial number of patients with suspected TB. Sputum smear and culture test results for M. tuberculosis could be verified only in 79% and 51% of cases, respectively, in our study. It is possible that the physicians did not request sputum tests or have requested sputum smears only without culture. According to a Korean study performed at a tertiary hospital, the initial sputum examinations were not performed at the time of diagnosis of PTB in 20% of patients which was similar to our results (Table 2) (20).
The guidelines for TB management in Korea published in 2004 recommended doctors to collect two sputum specimens for AFB smear and at least one for culture from cases that are suspected to have PTB (suspicious findings on chest radiographs or suspicious symptoms of PTB) in the diagnosis of PTB (21). In our study, we verified sputum culture results in 51% and requests of two or more sputum AFB smear tests in 35.3% of total patients. The rates are obviously lower than those of public sectors. In 2004 (the same year of our study), the request rate of AFB smear ( = [total count of requested AFB smear tests] ÷ [total number of registered PTB cases × 2]) was 95% and that of culture in public health care centers was 98%.
One of the possible explanations for the lack of adherence to the national guideline in the diagnosis of PTB is the capacity for sputum tests. Secondary and tertiary hospitals of Korea are equipped with laboratories where mycobacterial tests can be performed, while the majority of primary clinics are not. Therefore private physicians in the primary clinics must send the specimen to commercial or public health laboratories (e.g. public health care center or laboratories of Korean National Tuberculosis Association) for microbiological tests (specifically, the culture) which is cumbersome and requires a relatively longer period for acquiring the results. Our data suggest that primary clinics rather than secondary or tertiary hospitals are less likely to perform sufficient microbiological tests (Tables 2, 3). However, the exact percentage or number of physicians using the hospital, commercial and public labs are unknown.
The low adherence to the national guideline in the diagnosis of TB in Korea calls for a continuing medical education and a greater role of the public health organization. In Korea, PPM-DOTS (public-private mix for directly observed therapy, short course) have been introduced to large scale private sectors recently, which could encourage physicians to adhere to the national guideline as public sectors. Such national services provided and organized in primary clinics may prove beneficial to primary physicians. If the accessibility to public laboratories improves, the diagnosis based on microbiology in private sectors will also become more reliable.
The lack of proper microbiological tests may lead to overdiagnosis of TB. In the absence of positive sputum AFB smears, most cases of PTB are diagnosed on the basis of clinical findings which depend heavily on the findings of chest radiographs (22). However, some limitations exist: 1) inter-observer variability in interpretation of chest radiographs (23); 2) difficulty in differentiation of pneumonia from PTB (24) since it shows clinical and radiological response with rifampicin (25, 26); 3) an inexperienced physician in TB contributing to lower TB prevalence rate and lower diagnostic accuracy of chest radiographs (27-30); 4) Difficulty in differentiation from non-tuberculous mycobacteria (NTM) lung diseases which have been increasing in Korea (31).
In this study, the assessment of the diagnostic validity of PTB using chest radiograph at diagnosis and follow-up chest radiograph after at least one month of anti-tuberculosis treatment was performed. The diagnosis of TB can be strongly inferred by the clinical and radiographic response to anti-TB treatment (19). The cases with a cavity, multiple nodules or consolidation in initial chest radiograph were regarded as 'compatible with active PTB (category 8)' in our study, and comprised only 54.9% (95% CI, 52.0%-57.8%) (33-36). However, 77.5% of the 454 cases with follow-up chest radiographs showed radiographic response (category 9). This suggests that a large number of cases whose initial chest radiographs revealed atypical findings of TB and showed improvement spontaneously or with a rifampicin-including anti-TB regimen may be of other lung diseases such as pneumonia.
A variety of diagnostic modalities are utilized to diagnose TB in private sectors of Korea where medical resources and laboratory services are more advanced and easily accessible than those of other developing countries. The advanced diagnostic modalities contribute to more accurate diagnosis of TB. For example, chest CT is more sensitive than chest radiography in the detection of PTB. According to a study that compared chest CT with chest radiograph, the radiographic diagnosis of TB was initially correct in only 49% of all tuberculosis cases, while CT diagnosis of PTB was correct in 91% (36). Because the definitive diagnosis still requires an isolation and identification of M. tuberculosis complex in a clinical specimen, invasive procedures such as bronchoscopy with washing or biopsy may help in the diagnosis of TB. In addition, use of polymerase chain reaction (PCR) detection of bacterial DNA is increasing recently in the diagnosis of TB. Although performance frequency of PCR was relatively low (14.3%), half of the patients showed positive PCR results in the present study.
Some limitations exist due to the retrospective nature of the study as mentioned above. The missing data may affect the result. Chest radiography reports were found only in 71.1% of the patients, and chest radiograph was not performed in 5.2% of the notified PTB patients. Although the cases with an unknown status of chest radiograph were 23.6%, the imaging was probably performed in most of those cases and assessed by clinicians without the official reports of the radiologists. Patients who showed active TB in initial chest radiographs or improvement in the follow-up chest radiographs were approximately 62% of the total cases (n = 695). Of the 247 cases in which whether chest radiographs were performed or not is 'uncertain', 130 cases were classified into categories 1-9. Assuming that 62% of the remaining 117 cases also meet the criteria for radiological TB, then additional 72 possible cases (6.4% of the total of 1,126 cases) may be added. Since the records of other diagnostic tests such as PCR, histology, or bronchoscopy mostly remained unknown, most of the tests of unknown status may have been categorized as 'not performed' examination. Although the TB data from the year 2004 were analyzed in this study, it is difficult to conclude that it directly reflects the present clinical situation.
In conclusion, in 2004, the private sectors in Korea utilized various laboratory tests in diagnosis of PTB and more than 70% of the notified PTB cases were 'real TB'. The results may suggest the possibility of over-estimation of TB burden with the use of the notification-based TB data.
Figures and Tables
Table 2
The test modality and yield for diagnosis of tuberculosis that performed in private sector of Korea classified by scale of private hospital (n = 1,126)

References
1. World Health Organization. Global tuberculosis control: a short update to the 2009 report. 2009. Geneva: World Health Organization.
2. Dye C, Scheele S, Dolin P, Pathania V, Raviglione MC. Consensus statement. Global burden of tuberculosis: estimated incidence, prevalence, and mortality by country. WHO Global Surveillance and Monitoring Project. JAMA. 1999. 282:677–686.
3. Ministry of Health and Welfare and Korean National Tuberculosis Association. Report on the 7th tuberculosis prevalence survey in Korea. 1995. Seoul: Ministry of Health and Welfare and Korean National Tuberculosis Association.
4. Hong YP, Kim SJ, Lew WJ, Lee EK, Han YC. The seventh nationwide tuberculosis prevalence survey in Korea, 1995. Int J Tuberc Lung Dis. 1998. 2:27–36.
5. Lew WJ, Lee EG, Bai JY, Kim HJ, Bai GH, Ahn DI, Lee JK, Kim SJ. An internet-based surveillance system for tuberculosis in Korea. Int J Tuberc Lung Dis. 2006. 10:1241–1247.
6. World Health Organization. Global tuberculosis control: surveillance, planning, financing. 2003. Geneva: World Health Organization.
7. Pillaye J, Clarke A. An evaluation of completeness of tuberculosis notification in the United Kingdom. BMC Public Health. 2003. 3:31.
8. EuroTB and the National Coordinators for Tuberculosis Surveillance in the WHO. European Region. Surveillance of tuberculosis in Europe. Report on tuberculosis cases notified in 2006. 2006. Saint-Maurice: Institut de Veille Sanitaire.
9. Heo E, Oh SY, Jeong I, Lee JS, Lim HJ, Park YS, Lee JW, Han SK, Lee CH. The diagnostic accuracy of notified new culture-negative pulmonary tuberculosis patients in public healthcare centers. Korean J Med. 2009. 76:44–51.
10. Jelastopulu E, Alexopoulos EC, Venieri D, Tsiros G, Komninou G, Constantinidis TC, Chrysanthopoulos K. Substantial underreporting of tuberculosis in West Greece: implications for local and national surveillance. Euro Surveill. 2009. 14:19152.
11. Baussano I, Bugiani M, Gregori D, van Hest R, Borraccino A, Raso R, Merletti F. Undetected burden of tuberculosis in a low-prevalence area. Int J Tuberc Lung Dis. 2006. 10:415–421.
12. Cojocaru C, van Hest NA, Mihaescu T, Davies PD. Completeness of notification of adult tuberculosis in Iasi County, Romania: a capture-recapture analysis. Int J Tuberc Lung Dis. 2009. 13:1094–1099.
13. Sheldon CD, King K, Cock H, Wilkinson P, Barnes NC. Notification of tuberculosis: how many cases are never reported? Thorax. 1992. 47:1015–1018.
14. Kim CH, Koh WJ, Kwon OJ, Ahn YM, Lim SY, An CH, Youn JW, Hwang JH, Suh GY, Chung MP, et al. The accuracy of tuberculosis notification reports at a private general hospital after enforcement of new Korean tuberculosis surveillance system. Tuberc Respir Dis. 2003. 54:178–190.
15. World Health Organization. International Union Against Tuberculosis and Lung Disease. Royal Netherlands Tuberculosis Association. Revised international definitions in tuberculosis control. Int J Tuberc Lung Dis. 2001. 5:213–215.
16. World Health Organization. International statistical classification of diseases and related health problems: 10th revision. 2008. Geneva: World Health Organization.
17. Migliori GB, Spanevello A, Ballardini L, Neri M, Gambarini C, Moro ML, Trnka L, Raviglione MC. Validation of the surveillance system for new cases of tuberculosis in a province of northern Italy. Varese Tuberculosis Study Group. Eur Respir J. 1995. 8:1252–1258.
18. Rieder HL, Watson JM, Raviglione MC, Forssbohm M, Migliori GB, Schwoebel V, Leitch AG, Zellweger JP. Surveillance of tuberculosis in Europe. Working Group of the World Health Organization (WHO) and the European Region of the International Union Against Tuberculosis and Lung Disease (IUATLD) for uniform reporting on tuberculosis cases. Eur Respir J. 1996. 9:1097–1104.
19. American Thoracic Society. CDC. Infectious Diseases Society of America. Treatment of tuberculosis. MMWR Recomm Rep. 2003. 52:1–77.
20. Koh WJ, Kwon OJ, Kim CH, Ahn YM, Lim SY, Yun JW, Hwang JH, Suh GY, Chung MP, Kim H, et al. Clinical characteristics and treatments outcomes of patients of pulmonary tuberculosis at a private general hospital. Tuberc Respir Dis. 2003. 55:154–164.
21. Korea Center for Disease Control and Prevention. The guideline of TB management. 2004.
22. Siddiqi K, Lambert ML, Walley J. Clinical diagnosis of smear-negative pulmonary tuberculosis in low-income countries: the current evidence. Lancet Infect Dis. 2003. 3:288–296.
23. Balabanova Y, Coker R, Fedorin I, Zakharova S, Plavinskij S, Krukov N, Atun R, Drobniewski F. Variability in interpretation of chest radiographs among Russian clinicians and implications for screening programmes: observational study. BMJ. 2005. 331:379–382.
24. Schlossberg D. Acute tuberculosis. Infect Dis Clin North Am. 2010. 24:139–146.
25. Korvick JA, Peacock JE Jr, Muder RR, Wheeler RR, Yu VL. Addition of rifampin to combination antibiotic therapy for Pseudomonas aeruginosa bacteremia: prospective trial using the Zelen protocol. Antimicrob Agents Chemother. 1992. 36:620–625.
26. Sharma A, Shariff M, Thukral SS, Shah A. Chronic community-acquired Acinetobacter pneumonia that responded slowly to rifampicin in the anti-tuberculous regime. J Infect. 2005. 51:e149–e152.
27. Catanzaro A, Perry S, Clarridge JE, Dunbar S, Goodnight-White S, LoBue PA, Peter C, Pfyffer GE, Sierra MF, et al. The role of clinical suspicion in evaluating a new diagnostic test for active tuberculosis: results of a multicenter prospective trial. JAMA. 2000. 283:639–645.
28. Llewellyn H. The effect of disease prevalence on positive predictive value: a simple model. Cytopathology. 2006. 17:101–103.
29. Schulman KA, Escarce JJ, Eisenberg JM, Hershey JC, Young MJ, McCarthy DM, Williams SV. Assessing physicians' estimates of the probability of coronary artery disease: the influence of patient characteristics. Med Decis Making. 1992. 12:109–114.
30. Lee S. Yoo S, editor. Clinical epidemiology. 2004. Seoul: Gyechook Publisher;141–159.
31. Jeon K, Koh WJ, Kwon OJ, Suh GY, Chung MP, Kim H, Lee NY, Park YK, Bai GH. Recovery rate of NTM from AFB smear-positive sputum specimens at a medical centre in South Korea. Int J Tuberc Lung Dis. 2005. 9:1046–1051.
32. Scott B, Schmid M, Nettleman MD. Early identification and isolation of inpatients at high risk for tuberculosis. Arch Intern Med. 1994. 154:326–330.
33. Tattevin P, Casalino E, Fleury L, Egmann G, Ruel M, Bouvet E. The validity of medical history, classic symptoms, and chest radiographs in predicting pulmonary tuberculosis: derivation of a pulmonary tuberculosis prediction model. Chest. 1999. 115:1248–1253.
34. Kanaya AM, Glidden DV, Chambers HF. Identifying pulmonary tuberculosis in patients with negative sputum smear results. Chest. 2001. 120:349–355.
35. Bah B, Massari V, Sow O, Siriwardana M, Camara LM, Larouzé B, Murray JF. Useful clues to the presence of smear-negative pulmonary tuberculosis in a West African city. Int J Tuberc Lung Dis. 2002. 6:592–598.
36. Lee KS, Hwang JW, Chung MP, Kim H, Kwon OJ. Utility of CT in the evaluation of pulmonary tuberculosis in patients without AIDS. Chest. 1996. 110:977–984.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download