Abstract
The aim of this study was to elucidate the epidemiology of traumatic head injury (THI) among Korean children. A prospective, in-depth trauma survey was conducted in five teaching hospitals. Data from all of the children who attended the emergency department (ED) were analyzed. From June 2008 to May 2009, 2,856 children with THI visited the 5 EDs. The average age of the subjects was 5.6 (SD ± 4.9) yr old, and 1,585 (55.5%) were 0-4 yr old. The male-to-female ratio was 2.3 to 1 (1,979 vs 877). Consciousness levels of the subjects were classified according to the Glasgow Coma Scale (GCS), and 99.1%, 0.6%, and 0.4% were determined as mild, moderate, or severe injury, respectively, according to the GCS categorization. Most injuries occurred at home (51.3%), and the most common mechanism of injury was collision (43.2%). With regard to outcome, 2,682 (93.9%) patients were sent home, and 35 (1.2%) were transferred to another hospital. A total of 133 (4.7%) patients were hospitalized, and 38 (1.3%) underwent surgery. The incidence and characteristics of pediatric THI in Korea are affected by sex, location and injury mechanism.
Although pediatric mortality caused by infection and malnutrition has decreased remarkably through improved public hygiene and nutrition, pediatric disability and death due to injury have increased substantially (1-3). In developed countries, trauma is known as the leading cause of disability and death among children, accounting for approximately 1/3 of all deaths in children aged 0-14 yr old (4-7). In Korea, the rate of mortality due to injury in children has also exceeded that of disease (8, 9). Traumatic head injury (THI) is one of the most common injuries associated with disability and is a leading cause of non-fatal injury in children (9, 10).
Although the majority of patients with head trauma have a minor injury that requires no specific therapy, a small number have clinically significant intracranial injury. Because problems such as thinking and memory disturbance resulting from mild head injury are often not visible, and public awareness about THI is limited, THI is frequently referred to as the "silent epidemic." THI is an important public health problem in terms of the possible complications of recovery and the resultant medical cost (9-13).
Because the majority of THI patients visit an emergency department (ED) for initial evaluation and management, a large number of previous studies on the epidemiology of THI patients have been conducted in the ED. In the United States, nationwide ED-based surveys have been conducted by the Centers for Disease Control and Prevention (CDC) to determine the epidemiological characteristics of THI patients (14). In Korea, studies on the basic data of THI patients are limited, with the exception of some studies of hospitalized THI patients in a single institution (15-18). We conducted this study to examine the demographic and clinical characteristics of pediatric THI through the analysis of ED-based, multicenter surveillance in Korea.
This study was conducted at five tertiary academic EDs (Seoul National University Hospital, Seoul National University Boramae Medical Center, Ilsan Hospital of Dongguk University, Jeju University Hospital and Gyeongsang National University Hospital) that comprise the 'Traumatic Brain Injury Network (TBIN) in Korea'. The TBIN is a consortium of clinical investigators who made a voluntary commitment to conduct collaborative, multicenter, clinical research regarding traumatic brain injury in Korea. Three were urban EDs with 30,000 to 50,000 annual visits each, and two were suburban EDs with 20,000 annual visits each. Prospective analysis of ED-based injury and in-depth investigation of injured patients presenting to the participating EDs were conducted during the period from June 1st, 2008 to May 31st, 2009. We reviewed data from active surveys and abstracts and analyzed data from all of the children (aged 0-18 yr) who visited the EDs of the 5 hospitals.
Registry data collected by 'TBIN' included demographic factors (age and gender of the subjects, time and place of injury, time and season of ED visits), clinical evaluation (cause of injury, presenting symptoms, level of consciousness), radiologic evaluation (radiological examinations, types of head injuries), and outcomes (discharge, transfer, hospitalization, surgery, and death).
All items of registry were classified based on the International Classification of External Causes of Injuries (ICECI) proposed by the World Health Organization (WHO) (19). In-depth surveillance data of THI patients was first collected by general practitioners and corrected by specialists in emergency medicine. Types of THI of children were identified by the International Classification of Disease-10th revision (ICD-10) discharge codes, as follows: 'open head wound' (S01.0-09), 'fracture of the skull and facial bones' (S02.0-.9), 'sprain and strain of joints and ligaments of other and unspecified parts of the head' (S03.5), 'intracranial injury' (S06.0-.9), 'crushing injury of the head' (S07.0-.9), 'traumatic amputation of part of the head' (S08.0-.9), and 'other and unspecified injuries of the head' (S09.0-.9).
The enrolled children were divided into 4 age brackets: 0-4 yr, 5-10 yr, 10-14 yr, and 15-18 yr. The severity of injury was classified into 3 groups in accordance with the Glasgow Coma Scale (GCS). Scores of 'mild', 'moderate', and 'severe' were used for GCS scores of 13-15, 9-12, and 3-8, respectively.
Statistical analysis was performed using SPSS software (version 17.0, Chicago, IL, USA) for the comparison of discrete-type variables using the Pearson square test and cascading type variables using the t-test and one-way ANOVA. The trend between age and usage of the head CT examination was estimated using a linear-by-linear association test. A P value < 0.05 was deemed statistically significant.
In total, injury surveillance data from 27,407 patients from June 2008 to May 2009 were investigated; 8,744 (31.9%) of these patients were children under the age of 19 yr. Among injured children, 2,856 children (32.7%) suffered from THI; 321 patients (11.2%) were transferred to participating hospitals from other medical institutions (Fig. 1).
The average age of patients was 5.6 ± 4.9 yr, and the male-to-female ratio was 2.3:1. Age distribution was as follows: 1,585 (55.5%) patients aged 0-4 yr, 713 (24.9%) patients aged 5-9 yr, 286 (18.9%) patients aged 10-14 yr, and 272 (9.5%) patients aged 15-18 yr. As age increased, male dominance was more obvious (P < 0.001) (Fig. 2).
When the day was divided to 'daytime' (08:00-16:00), 'afternoon/evening' (16:00-24:00), and 'night/morning' (24:00-08:00), 1,122 children (39.2%) incurred injuries during the daytime, 1,561 (54.7%) during the afternoon/evening, and 173 (6.0%) during the night/morning, illustrating that the majority of injuries occurred during the afternoon/evening. The 2-hr time interval with the highest frequency of occurrence was the 19:00-21:00 interval, accounting for 484 injuries (16.9%). On a monthly basis, there was no difference in the frequency of pediatric THI. There was no seasonal variation when spring (March to May; 749, 26.2%), summer (June to August; 690, 24.2%), autumn (September to November; 714, 25.0%), and winter (December to February; 703, 24.6%) were compared (P = 0.280).
Most injuries (1,465, 51.3%) occurred at home, followed by roads (444, 15.6%), playground/culture facilities (343, 12.0%), and school/educational facilities (241, 8.4%). Injuries at home were further divided according to specific locations. The most common location of injuries at home was the bedroom (661, 23.1%), followed by the living room (465, 16.3%), bathroom (115, 4.0%), garden (72, 2.5%), and kitchen (57, 2.0%). The younger the age of the subjects, the more injuries occurred at home. THI at home occurred in 1,112 (70.2%), 255 (35.8%), 58 (20.3%), and 40 (14.7%) children who were 0-4, 5-9, 11-14, and 15-18 yr old, respectively. Although the largest number of home THIs occurred in the bedroom and living room, the bathroom was the most common location for children aged 5-9 yr old (83, 11.6%). In addition, different age brackets showed different place-predominance, with a higher ratio of injuries at school among children aged 5-9 yr old (15.1%), a higher ratio of injuries at sports-related facilities among children aged 10-14 yr old (36.0%), and a higher ratio of injuries related to roads among children aged 15-18 yr (38.6%) (P < 0.001, Fig. 3).
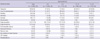
Common symptoms following THI included headache (182, 6.4%), loss of consciousness (97, 4.4%), vomiting (80, 2.8%), dizziness (58, 2.0%), and amnesia (48, 1.7%). The most frequent physical finding was scalp laceration in 512 children (17.9%) followed by scalp hematoma (137, 4.8%) (Table 1). The majority of children (2,829, 99.0%) visiting the ED with THI were classified as mild according to GCS score, while 16 patients (0.6%) were grouped as moderate, and 11 patients (0.4%) were classified as having severe head injury (Fig. 1).
With regard to the mechanism of injury, collision was the most common type (1,235, 43.2%) involved, followed by falls (1,105, 38.7%), motor vehicle collisions (MVC) (243, 8.5%), and injuries by sharp objects (186, 6.5%). As the subjects' age increased, injuries due to falls decreased, whereas the number of individuals injured by MVC and sharp objects increased. Collision (44.3%) and MVC (26.4%) were the main cause of injury among children aged 15-18 yr old (Fig. 4). Among MVC victims, the prevalence of subtype also differed. Car and pedestrian accidents were the most prevalent in the 0-4 yr age bracket (63.0%) and 5-9 yr age bracket (42.2%), respectively. Bicycle accidents and motorcycle accidents were more common among children aged 10-14 yr (31.4%) and 15-18 yr (61.1%), respectively.
A total of 1,072 (37.5%) and 633 (22.2%) subjects underwent simple skull X-ray and head CT, respectively. Skull X-ray examinations were performed in 599 (55.9%) children who were 0-4 yr old, 255 (23.8%) in the 5-9 yr age bracket, 116 (10.8%) in the 10-14 yr bracket, and 30 (11.0%) in the 15-18 yr bracket. Head CT was performed for 241 (38.1%) children in the age 0-4 yr age bracket, 152 (24.0%) in the 5-9 yr age bracket, 136 (21.5%) in the 10-14 yr bracket, and 144 (22.7%) in the 15-18 yr bracket. There was a positive linear relationship between age and use of the head CT examination (linear-by-linear association test, P < 0.001, Pearson correlation coefficient r = 0.255).
Among children who underwent each radiological evaluation, clinically significant lesions were detected in 56 (5.2%) and 92 (14.5%) by skull radiography and head CT, respectively. Rates of positive findings by head CT in each age bracket were 36/241 (14.9%), 28/152 (18.4%), 10/116 (8.6%), and 18/112 (16.1%) in the age ranges of 0-4, 5-9, 10-14, and 15-18 yr, respectively. The most frequently found radiologic abnormality was skull fracture (97, 3.4%), followed by epidural hemorrhage (25, 0.9%), subdural hemorrhage (25, 0.8%), subarachnoid hemorrhage (19, 0.7%), and brain edema (12, 0.4%).
Among enrolled children, 2,682 (93.9%) were discharged from the ED, 35 (1.2%) were transferred to another hospital, and 133 (4.7%) were hospitalized, including 25 admissions to the intensive care unit (ICU). Hospitalization rates for each age bracket were 19 (1.2%), 37 (5.2%), 22 (7.7%), and 55 (20.2%) in the 0-4, 5-9, 10-14, and 15-19 yr age brackets, respectively (P < 0.001). Rates of admission to the ICU in each age bracket were 2/1,585 (0.1%), 8/713 (1.1%), 6/286 (2.1%), and 9/272 (3.3%), respectively (P < 0.001). A total of 38 patients (1.3%) underwent surgical interventions and 19 patients (50.0%) underwent emergency operations.
Population-based data on THI in Korea are critical to understanding the impact of the THI epidemic on the Korean population. This report presents some epidemiologic data on ED visits, hospitalizations, and deaths of pediatric patients with THI. These data answer a wide range of important questions regarding how many pediatric THIs occur each year in Korea, who is affected, and how these THIs occur. The report is intended as a reference for policymakers, service providers, educators, researchers, advocates, and others interested in learning more about the impact of pediatric THI in Korea.
In this study, the age distribution of THI was aggregated in the younger age bracket, with more than half of subjects in the 0-4 yr old bracket. The gender ratio of the study showed male predominance and an increasing likelihood of male predominance in each age bracket as age increased. These findings coincide with the results of preceding reports (10, 20, 21). The daily distribution of THI followed a certain temporal pattern. A majority of injuries occurred in the afternoon/evening, similar to the pattern observed in the largest age bracket (children 0-4 yr old). The oldest children showed the highest prevalence of night/early daytime injury (53, 19.5%). Regarding seasonal variation, pediatric injuries have been assumed to occur mainly in summer due to the increased extent of activity, especially outdoor activity; however, no seasonal variation was observed in this study.
Our data confirmed that the home was the most common location of pediatric THI, as shown in previous studies (22, 23). With increasing age, the rate of injury at home tended to decrease, whereas the frequency of injuries outside the home (roads and playground/culture facilities) increased. This finding is believed to be associated with increasing engagement in outdoor activities among older children. We also analyzed the spatial trend of injuries in each age bracket. In all age brackets, the bedroom and living room were common locations of THI; however, in the 5-9 yr old age bracket, the bathroom was the most frequently reported location. This finding could be explained by the fact that interest in the surroundings and activities increases rapidly in this age bracket; however, there is also a relative lack of sense of balance and coordination, resulting in slipping injuries.
Based on a large study by the CDC of the US in 2000 (10), 98% of THI victims who visited the ED had a 'mild' form of THI. The most common cause of injury among 'mild' patients included 'falls' (28%), followed by MVC (20%), collision (19%), miscellaneous (13%), and assault (11%). The results from another study of hospitalized patients with traumatic head injury, conducted in the San Diego area (24), showed that the most common mechanism was MVC (37%), followed by falls (24%) and sports and leisure activities (21%). Previous two studies in Korea, which were based on hospitalized patients with traumatic head injury, demonstrated that pedestrian traffic accidents were the most common cause of injury (15, 16). In our study, most children (99.1%) were grouped as having mild THI, and the most common causes of injury among 'mild' patients were 'collision' and 'falls'. In cases with GCS scores of less than 12 points, MVC (44.4%) was the most common mechanism, followed by falls (37%) and collision (14.8%), which is a trend similar to that observed among research studies on hospitalized patients. Although falls are the most common cause of injury in non-fatal injuries according to the US CDC (10), the frequency of falls decreases with age, whereas MVC frequency increases with age. Similarly, in this study, the rate of occurrence of MVC among children aged 15-19 yr old was 3 times the rate observed in the youngest age bracket.
In an analysis of data from the National Hospital Ambulatory Care Survey (NHAMCS), in the US, the use of head CT increased from 12.8% to 22.4% from 1995 to 2003, and head CT was used more frequently in the older age brackets (25). In this study, the rate of head CT (22.2%) was relatively low compared to that determined by previous studies (28.6%-52.8%) (25-27). Children who had sustained multiple traumas were enrolled in the NHAMCS survey (25) and redefined and purified minor head injury patients were enrolled in the other two studies (26, 27). If we had excluded children with trivial causes of head injury such as ground-level falls or walking or running into stationary objects, the rate of CT examination might be similar to the data of the previous studies.
The appropriate use of CT has been an important healthcare issue because ionizing radiation from CT scans can cause lethal malignancies, especially in the more radiosensitive pediatric population. A recent estimate of the risk of developing cancer after one cranial CT scan depended on the age of the child at the time of the scan but ranged from 1:2,000 to 1:5,000 (28). There were numerous decision-making rules (26, 27) to decrease the usage of head CT, but their application to the Korean children may be quite different from that of other countries due to certain characteristics of Korean parents and unique characteristics of the medical insurance system. Further study is needed to identify the reason for relatively frequent usage of head CT among Korean children.
According to reports published by the US CDC in 2000 (10) and previous studies (12, 13, 25), a great majority of pediatric ED visitors with THI had mild conditions that did not require special treatment. However, in 4.5%-8.5% of children, there was a need for hospitalization; 3%-5% and 0.06% of children suffered significant and fatal injuries, respectively. In this study, 133 (4.7%) of the children were hospitalized and 38 (1.39%) of the children underwent surgery. Two children (0.06%) died prior to their arrival at the ED. One child was a 5 yr old boy who was involved in a pedestrian MVC; the other was a 15 yr old boy who was injured in a residential fire. Among the 34 children transferred to other hospitals, two children with critical brain injuries required emergency surgery.
In the case of THI data published by the US CDC in 2000 (10), the hospitalization rate and extent of severity of injury were highest among children aged 15-19 yr, while prevous Korean studies reported the highest hospitalization rate among children aged 5-9 yr (15, 16). In our study, the hospitalization rate and surgical procedure rate increased with age. Accordingly, about 20% of children in the 15-18 yr age bracket were hospitalized, with 5.9% undergoing surgery. This could be related to the fact that MVC accounts for a greater proportion of injuries as age increases in Korea.
This study has several limitations. First, although we reviewed the ED-based survey data from five referral hospitals, the included subjects represent only a proportion of children with THI in Korea. However, because data were collected from diverse areas of the country and the differences among data from participating hospitals were negligible, we believe that this study is representative of the nationwide characteristics of pediatric THI. Based on the results of this study, a national survey is highly warranted.
Second, even though there were some items in the registry such as ICISS (International Classification of disease-9 based Injury Severity Score), main department of admission and coexisting injuries, which could indicate potential reasons for hospitalization or operations, there were some difficulties in determining whether those decisions were made due to the THI itself or due to coexisting injuries.
Third, the survey data included small numbers of specialized items for young infants, especially those younger than 2 yr old. In the case of children under the age of 2 yr, who have open anterior fontanelle and lack communication skills, previous studies have shown different mechanisms and clinical features, compared with children over the age of two (29, 30). Accordingly, there are several items that should be added in the examination of infants. The preparation of more specialized registry items for further study is desirable.
In conclusion, this study is the first to analyze the epidemiology of pediatric patients with THI in Korea. The key patient group visiting the ED with THI was boys aged 0-4 yr old. More than half of injuries occurred in the afternoon/evening hours, with the highest burden between the hours of 19:00-21:00. Despite a significant trend of injury due to collision and falls in young children, injuries on the road due to MVC increased in frequency with increasing age. The majority of patients were sent home after ED management. Regarding hospitalization, the rate of hospitalization was highest among children aged 15-18 yr old. With regard to THI among children, the methods for coping with and treating injury as well as methods for the prevention of injury should differ according to the age of the patient. The characterization of THI in this population will provide the basis for further investigations and identify the optimal focus for preventative measures.
Figures and Tables
References
1. Nagaraja J, Menkedick J, Phelan KJ, Ashley P, Zhang X, Lanphear BP. Deaths from residential injuries in US children and adolescents, 1985-1997. Pediatrics. 2005. 116:454–461.
2. National vital statistics report. National Center for Health Statistics. accessed on 16 March 2011. Available at http://www.cdc.gov/nchs/data/nvsr/nvsr59/nvsr59_04.pdf.
3. A league table of child deaths by injury in rich countries. UNICEF. accessed on 6 February 2011. Available at http://www.unicef-irc.org/publications/pdf/repcard2e.pdf.
4. Web-based injury statistics query and reporting system. National Center for Injury Prevention and Control. accessed on 6 September 2009. Available at http://webappa.cdc.gov/sasweb/ncipc/leadcaus10.html.
5. Bayreuther J, Wagener S, Woodford M, Edwards A, Lecky F, Bouamra O, Dykes E. Pediatric trauma: injury pattern and mortality in the UK. Arch Dis Child Educ Pract Ed. 2009. 94:37–41.
6. Krug EG, Sharma GK, Lozano R. The global burden of injuries. Am J Public Health. 2000. 90:523–526.
7. Sosin DM, Sniezek JE, Waxweiler RJ. Trends in death associated with traumatic brain injury, 1979 through 1992. Success and failure. JAMA. 1995. 273:1778–1780.
8. Annual report on the cause of death statistics, 2009. Korean Statistical Information Service. accessed on 18 July 2011. Available at http://www.bokjiro.go.kr/data/statusView.do?board_sid=297&data_sid=213671.
9. Park HS, Koh SB, Lee BE. Health and Human Services Report 2006. Construction of national system for child injury and safety statistics.
10. Traumatic brain injury in the United States: assessing outcomes in children. National Center for Injury Prevention and Control. accessed on 18 July 2011. Available at http://www.cdc.gov/traumaticbraininjury/assessing_outcomes_in_children.html.
11. Schwartz L, Taylor HG, Drotar D, Yeates KO, Wade SL, Stancin T. Long-term behavior problems following pediatric traumatic brain injury: prevalence, predictors, and correlates. J Pediatr Psychol. 2003. 28:251–263.
12. Langlois JA, Rutland-Brown W, Thomas KE. The incidence of traumatic brain injury among children in the United States: differences by race. J Head Trauma Rehabil. 2005. 20:229–238.
13. Schneier AJ, Shields BJ, Hostetler SG, Xiang H, Smith GA. Incidence of pediatric traumatic brain injury and associated hospital resource utilization in the United States. Pediatrics. 2006. 118:483–492.
14. Traumatic brain injury in the united state: emergency department visits, hospitalization, and deaths. National Center for Injury Prevention and Control. accessed on 18 July 2011. Available at http://www.cdc.gov/ncipc/pub-res/tbi_in_us_04/tbi%20in%20the%20us_jan_2006.pdf.
15. Ryu MS, Lee KS. Traumatic brain injury in children. J Korean Child Neurol Soc. 2006. 14:87–93.
16. Lee KW, Hwang SK, Sung JK, Hamm IS, Park YM, Kim SL. Pediatric head injury. J Korean Neurosurg Soc. 1999. 28:42–47.
17. Youn S, Lee MA, Kim HM, Cha BH. The incidence and risk factors of post-traumatic seizure in children. Korean J Pediatr. 2004. 47:1198–1204.
18. Kim JK, Park JY, Cho TH, Kwon TH, Lim DJ, Chung YK, Lee KC, Lee HK. Clinical features and prognostic factors of head injury in less than two year old children. J Korean Neurosurg Soc. 1998. 27:625–631.
19. Testing ICECI: review and filed testing. Amsterdam: Consumer Safety Institute; September 2004. WHO-ICECI Coordination and Maintenance Group. accessed on 18 July 2011. Available at http://www.rivm.nl/who-fic/ICECIeng.htm.
20. Dunning J, Daly JP, Malhotra R, Stratford-Smith P, Lomas JP, Lecky F, Batchelor J, Mackway-Jones K. Children's Head Injury Algorithm for the Identification of Significant Clinical Events Study. The implications of NICE guidelines on the management of children presenting with head injury. Arch Dis Child. 2004. 89:763–767.
21. Berry JG, Jamieson LM, Harrison JE. Head and traumatic brain injuries among Australian children, July 2000-June 2006. Inj Prev. 2010. 16:198–202.
22. Shudy M, de Almeida ML, Ly S, Landon C, Groft S, Jenkins TL, Nicholson CE. Impact of pediatric critical illness and injury on families: a systematic literature review. Pediatrics. 2006. 118:S203–S218.
23. Hawkins ER, Brice JH, Overby BA. Welcome to the world: findings from an emergency medical services pediatric injury prevention program. Pediatr Emerg Care. 2007. 23:790–795.
24. Kraus JF, Fife D, Cox P, Ramstein K, Controy C. Incidence, severity and external causes of pediatric head injury. Am J Dis Child. 1986. 140:687–693.
25. Blackwell CD, Gorelick M, Holmes JF, Bandyopadhyay S, Kuppermann N. Pediatric head trauma: changes in use of computed tomography in emergency departments in the United States over time. Ann Emerg Med. 2007. 49:320–324.
26. Kuppermann N, Holmes JF, Dayan PS, Hoyle JD Jr, Atabaki SM, Holubkov R, Nadel FM, Monroe D, Stanley RM, Borgialli DA, Badawy MK, Schunk JE, Quayle KS, Mahajan P, Lichenstein R, Lillis KA, Tunik MG, Jacobs ES, Callahan JM, Gorelick MH, Glass TF, Lee LK, Bachman MC, Cooper A, Powell EC, Gerardi MJ, Melville KA, Muizelaar JP, Wisner DH, Zuspan SJ, Dean JM, Wootton-Gorges SL. Pediatric Emergency Care Applied Research Network (PECARN). Identification of children at very low risk of clinically important brain injuries after head trauma: a prospective cohort study. Lancet. 2009. 374:1160–1170.
27. Osmond MH, Klassen TP, Wells GA, Correll R, Jarvis A, Joubert G, Bailey B, Chauvin-Kimoff L, Pusic M, McConnell D, Nijssen-Jordan C, Silver N, Taylor B, Stiell IG. Pediatric Emergency Research Canada (PERC) Head Injury Study Group. CATCH: a clinical decision rule for the use of computed tomography in children with minor head injury. CMAJ. 2010. 182:341–348.
28. Brenner DJ, Hall EJ. Computed tomography: an increasing source of radiating exposure. N Engl J Med. 2007. 357:2277–2284.
29. Berney J, Favier J, Froidevaux AC. Paediatric head trauma: estimate risk of influence of age and sex. I. Epidemiology. Childs Nerv Syst. 1994. 10:509–516.
30. Duhaime AC, Alario AJ, Lewander WJ, Schut L, Sutton LN, Seidl TS, Nudelman S, Budenz D, Hertle R, Tsiaras W, Loporchio S. Head injury in very young children: mechanism, injury type, and ophthalmologic findings in 100 hospitalized patient younger than 2 years of age. Pediatrics. 1992. 90:179–185.




 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download