Abstract
The aim of this study was to assess the prevalence of diabetes and to study the effects of excess growth hormone (GH) on insulin sensitivity and β-cell function in Korean acromegalic patients. One hundred and eighty-four acromegalic patients were analyzed to assess the prevalence of diabetes, and 52 naïve acromegalic patients were enrolled in order to analyze insulin sensitivity and insulin secretion. Patients underwent a 75 g oral glucose tolerance test with measurements of GH, glucose, insulin, and C-peptide levels. The insulin sensitivity index and β-cell function index were calculated and compared according to glucose status. Changes in the insulin sensitivity index and β-cell function index were evaluated one to two months after surgery. Of the 184 patients, 17.4% were in the normal glucose tolerance (NGT) group, 45.1% were in the pre-diabetic group and 37.5% were in the diabetic group. The insulin sensitivity index (ISI0,120) was significantly higher and the HOMA-IR was lower in the NGT compared to the diabetic group (P = 0.001 and P = 0.037, respectively). The ISI0,120 and disposition index were significantly improved after tumor resection. Our findings suggest that both insulin sensitivity and β-cell function are improved by tumor resection in acromegalic patients.
Glucose homeostasis abnormalities such as impaired glucose intolerance (IGT) and diabetes mellitus frequently affect acromegalic patients. The prevalence of IGT or diabetes mellitus differs widely between studies due to differences in patient numbers and ethnicity (1-3).
Impaired glucose metabolism in acromegalic patients is frequently associated with hyperinsulinemia (4, 5). It has been suggested that impaired glucose metabolism is mediated by growth hormone (GH)-induced insulin resistance. Several studies have suggested that insulin resistance contributes to abnormal glucose tolerance in acromegalic patients (6-8), but Kasayama et al. (9) reported that impaired β-cell function is important in determining the glucose tolerance status in acromegalic patients, and Kinoshita et al. (10) reported that once β-cell function is impaired, abnormal glucose metabolism persists even after patients have been cured of acromegaly. Therefore, both insulin resistance and pancreatic β-cell dysfunction appear to be involved in the pathogenesis of glucose homeostasis abnormalities in acromegalic patients. Furthermore, some studies have reported a direct correlation between plasma GH levels and the degree of glucose intolerance (11, 12).
The aim of this study was to assess the prevalence of diabetes, impaired fasting glucose (IFG) and IGT in Korean patients with acromegaly and to study the changes in insulin sensitivity and β-cell function index with a reduction in excess GH after tumor resection.
Our study included 184 acromegalic patients who had been diagnosed with acromegaly at Samsung Medical Center between 1996 and 2009. The prevalence of diabetes was assessed in these patients. Patients were classified as having a normal glucose tolerance (NGT, fasting plasma glucose [FPG] < 100 mg/dL and 2-hr glucose post-prandial glucose [PPG] < 140 mg/dL), IFG (FPG 100-125 mg/dL), IGT (PPG 140-199 mg/dL) and diabetes (FPG ≥ 140 mg/dL and/or PPG ≥ 200 mg/dL) according to the American Diabetes Association diagnostic criteria (13).
Diagnosis of active acromegaly was based on characteristic clinical findings, plasma GH elevated above 1 µg/L during the 75 g oral glucose tolerance test (OGTT) and plasma insulin-like growth factor-1 (IGF-1) elevated above the normal range for age and sex. During the OGTT, glucose and GH levels were measured before ingestion and at 30, 60, 90, and 120 min thereafter, and insulin and C-peptide levels were measured before ingestion and then at 30 and 120 min. All measurements were performed prior to any therapeutic intervention. Completely cured acromegaly was defined as a GH less than 1 µg/L during the OGTT. Disease duration was evaluated by patient interview.
Several models were used to estimate insulin sensitivity and secretion using plasma glucose and insulin concentrations measured during the OGTT. For basal insulin secretion and insulin resistance, the homeostasis model assessment of β-cell function (HOMA-β) and insulin resistance (HOMA-IR) were calculated (15). ISI0,120 is a formula for the insulin sensitivity index (ISI), and was calculated as follows: {75,000 + (glucose0min [mg/dL] - glucose120min [mg/dL]) × 0.19 × body weight (kg)/[120 × log(insulin0min [µU/mL] + insulin120min [µU/mL])/2 × (glucose0min [mg/dL] + glucose120min [mg/dL)/2]} (16). The disposition index (DI) was calculated as the insulinogenic index multiplied by ISI0,120. The DI has been proposed as a measurement of the ability of β-cells to compensate for insulin resistance (17). Lower DI values indicate an inability of β-cells to secrete enough insulin at that particular level of insulin resistance. We also calculated the first and second phase of insulin secretion. First-phase insulin secretion = 1,283 + 1.829 × insulin30min (pM/L) - 138.7 × glucose0min (mM/L) + 3.772 × insulin0min (pM/L) and second-phase insulin secretion = 287 + 0.4164 × insulin30min (pM/L)-26.07 × glucose30min (mM/L) + 0.9226 × insulin0min (pM/L) (18).
Of the 184 acromegalic patients, 35 patients with known diabetes and 44 patients lacking laboratory data for insulin and C-peptides were excluded from the analysis of insulin sensitivity and β-cell function. Of the 105 acromegalic patients, 80 patients underwent the 75 g OGTT one to two months after the transsphenoidal surgery. Fifty-two patients were included in the final analysis to assess changes in insulin sensitivity and β-cell function after tumor resection.
Data are presented as the mean ± standard deviation (SD) or median (25th percentile to 75th percentile). A chi-square with Fisher's exact test or the Kruskal-Wallis test was used to detect differences between the groups. Wilcoxon's signed-rank test was used to assess changes after tumor resection and Spearman's correlation analysis was used to assess correlations. Statistical analysis was performed using PASW 18.0 software (SPSS Inc., Chicago, IL, USA). For all statistical analyses, a P value < 0.05 (two-sided) was considered statistically significant.
Of the 184 acromegalic patients, 69 patients (37.5%) were diabetics (including those who were previously known diabetics), 43 patients (23.4%) were IGT, 16 patients (8.7%) were IFG, 23 patients (13.0%) were combined IGT and IFG, and 32 patients (17.4%) were NGT.
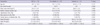
We re-categorized the 184 patients into three groups (NGT, pre-diabetic [IFG + IGT] and diabetic). The clinical characteristics of all 184 patients are shown in Table 1. The diabetic patients were significantly older than the pre-diabetic and the NGT patients.
Fifty-two patients were included for the final analysis to assess changes in insulin sensitivity and β-cell function after tumor resection. Twelve patients (23.1%) were diabetic, 27 patients (51.9%) were pre-diabetic and 13 patients (25.0%) were classified as having a NGT. The median age was 40 yr (30-51). The median basal GH, nadir GH, and IGF-1 levels were 16.9 µg/L (9.0-26.9), 13.0 µg/L (5.7-26.9) and 1,051.8 (851.9-1,353.9), respectively. Body mass index (BMI) was 26.1 ± 2.6 kg/m2.
Serum glucose levels after the ingestion of 75 g of glucose were significantly higher in patients with diabetes (P = 0.001) (Fig. 1). Serum C-peptide levels at 0 min of the OGTT were higher in the diabetic group compared to the pre-diabetic group (P = 0.028), and serum C-peptide levels at 120 min of the OGTT were higher in the diabetic group when compared to the NGT group (P = 0.023). There were no significant differences in family history of diabetes, sex or the presence of hypertension among the three groups (Table 2). There were also no significant differences in basal GH, nadir GH, or IGF-1 between the three groups.
Hypocortisolism was present in 28 (64.3%) patients before tumor resection and in 15 (28.8%) patients after tumor resection. Hypothyroidism was present in three (5.8%) patients before tumor resection and in one (1.9%) patient afterwards. The prevalence of hypocortisolism and hypothyroidism was not significantly different between groups.
The insulin sensitivity index, ISI0,120, was significantly higher and HOMA-IR was significantly lower in the NGT group compared to the pre-diabetic and diabetic groups (Fig. 2). HOMA-β did not differ significantly between the groups (P = 0.116). The first-phase insulin secretion was significantly higher in the NGT group compared to the pre-diabetic and diabetic groups (Fig. 2). The second-phase insulin secretion was not different among the three groups (P = 0.062). The DI also was markedly decreased in the diabetic group as compared to the NGT group (P = 0.009).
The nadir GH, basal GH and IGF-1 levels did not correlate with the DI, HOMA-β, or the first or second phase insulin secretion indexes. The IGF-1 level correlated with HOMA-IR (r = 0.416, P = 0.002), the basal insulin level (r = 0.406, P = 0.003), and the basal C-peptide level (r = 0.381, P = 0.005). HOMA-IR was positively correlated with HOMA-β (r = 0.369, P = 0.007), and the first and second phases of insulin secretion (r = 0.359, P = 0.014 and r = 0.383, P = 0.009, respectively).
Normalization of excess GH (< 1 µg/L) occurred in 26 patients (50%). There were significant improvements in the average levels of basal GH (16.9 [9.0-26.9] vs 1.8 [0.4-4.3], P = 0.001), nadir GH (13.0 [5.7-26.9] vs 0.6 [0.1-2.4], P = 0.001) and IGF-1 (1,051.8 [851.9-1,353.9] vs 423.8 [269.3-636.0], P = 0.001) after tumor resection.
Of the 13 NGT patients, 10 retained a NGT status and 3 patients became pre-diabetic after the surgery. Of the 27 pre-diabetic patients, 18 patients achieved a NGT status, while the rest 9 remained in a pre-diabetic state after the surgery. Of the 12 diabetes patients, 7 patients attained a NGT status, 4 patients became pre-diabetic and 1 patient remained diabetic after the surgery. With the exception of the three NGT patients who were reclassified as being pre-diabetic after the surgery, all glucose levels at 0, 30, 60, 90, and 120 min were significantly improved after tumor resection, regardless of the extent of tumor resection, glucose concentration or the presence of other hormone deficiencies (Fig. 3). We noted significant improvements in HOMA-IR, ISI0,120 and DI one to two months after surgery. There were significant decreases in the first-phase insulin secretion (1,315.9 [868.8-2,258.8] vs 1,114.5 [839.0-2,258.8] P = 0.007) and secondphase insulin secretion indexes (354.2 [251.0-568.1] vs 301.2 [232.3-408.5] P = 0.003). However, there were no significant improvements in HOMA-β after the surgery (Fig. 3).
The improvements in HOMA-IR, ISI0,120 and DI occurred in both the completely and incompletely cured groups. The group of patients that still had a nadir GH level elevated above 1 µg/L also showed improvements in HOMA-IR [3.9 (2.7-4.9) vs 2.0 (1.2-3.1), P = 0.001], ISI0,120 [0.31 (0.12-0.61) vs 1.48 (0.89-2.43), P = 0.001] and DI [0.23 (0.06-0.45) vs 1.77 (1.40-2.09), P = 0.001]after the surgery.
Of the 184 acromegalic patients in this study, only 17.4% of patients had a normal glucose status. The prevalence of diabetes was 37.5%, including those who were previously known diabetic patients, which is much higher than that seen in the general Korean population (9.1%) (19). A previous study reported that the prevalence of diabetes and IGT varied widely from 19% to 56% and from 16% to 46%, respectively (1, 3). This study sample had a higher prevalence of glucose intolerance than that reported in previous studies (12, 20), which could be partly attributed to the difference in diagnostic criteria used in our study (NGT, FPG < 100 mg/dL) compared to previous studies (NGT, FPG < 110 mg/dL) (9, 11).
The clinical risk factors for glucose intolerance in acromegaly are known to be a prolonged duration of disease, a family history of diabetes, age and the presence of macroadenoma (1, 2). Age differed significantly between the diabetic and pre-diabetic or NGT groups in our study (Table 1). However, other factors did not significantly affect glucose intolerance.
We assessed insulin sensitivity and β-cell function according to glucose status. Kasayama et al. (9) reported that insulin sensitivity is reduced to a similar extent in acromegalic patients regardless of glucose status, and that impaired β-cell function determined the glucose status in acromegalic patients. Kinoshita et al. (10) also reported that the parameters of insulin resistance did not differ significantly according to glucose status. However, our study showed that both insulin sensitivity and β-cell function, as measured by ISI0,120 and the first phase of insulin secretion index, were lower in the diabetic patients compared to the NGT patients. This suggests that impaired β-cell function, with reduced insulin sensitivity, occurs during the development of glucose intolerance from NGT to hyperglycemia in acromegalic patients. In the pre-diabetic state, there was a significant decrease in the ISI0,120 and the DI. However, the HOMA-IR and HOMA-β did not differ between the NGT and pre-diabetic groups. Furthermore, HOMA-β was not significantly different between the NGT and diabetic groups. This suggests that the ISI0,120 and the first-phase insulin secretion index are more useful methods than HOMA analysis in evaluating insulin sensitivity and β-cell function in acromegalic patients (Fig. 2).
Of the 52 patients, 26 (50%) achieved normalization of GH and IGF-1 levels after surgery. There were no differences in the levels of GH and IGF-1 according to glucose status, which is consistent with the findings of previous studies (2, 9). However, IGF-1 levels were correlated with HOMA-IR and fasting insulin, similar to what was shown in previous studies (12, 21).
One to two months after the trans-sphenoidal surgery, patients showed significant improvements in serum nadir GH and IGF-1 levels, as well as in ISI0,120, HOMA-IR, and the DI. Wasada et al. (7) and Moller et al. (8) also reported that insulin sensitivity improved two to four months after surgery, and even within two weeks of the surgery. Insulin sensitivity improved in both the completely and incompletely cured groups in our study. Kinoshita et al. (10) reported that improving insulin resistance contributes to the restoration of normal glucose metabolism. They also reported that postoperative values of insulin resistance were similar between NGT and IGT/diabetic groups, and that HOMA-β was significantly lower in the IGT/diabetic group.
In most of our patients, all glucose levels during the OGTT were significantly improved after tumor resection, regardless of the extent of tumor resection, glucose concentration or the presence of other hormone deficiencies. These improvements can be explained by the improvements in both insulin resistance and β-cell function. The insulin secretion indexes, both first-and second-phase were decreased with improvements in insulin resistance after tumor resection. However, the DI, which is a measure of pancreatic function, improved after tumor resection, suggesting that not only insulin resistance, but also the ability of β-cells to compensate for particular level of insulin resistance improved after tumor resection.
There were still significant differences in the DI (2.02 ± 0.66 vs 1.49 ± 0.46, P = 0.001) between patients who recovered NGT after the surgery (n = 28) and patients who retained a pre-diabetic/diabetic status after the surgery (n = 14), and there were no differences in HOMA-β, ISI0,120, or the first-or second-phase insulin secretion indexes among the groups (data not shown)
contrary to the study by Kinoshita et al. (10).
GH is known to stimulate the proliferation of pancreatic β-cells and enhances insulin secretion (22, 23). However, when there is an excess of GH, glucose intolerance develops. The exact mechanism underlying a decreased insulin secretion index or increased insulin resistance is not fully understood in acromegalic patients. However, there have been several studies regarding the mechanism of increased insulin resistance in acromegalic patients. Hansen et al. reported that GH results in insulin resistance by altering the function at the post-binding stage, and in vitro observations revealed that GH decreases insulin binding at high concentrations of insulin (24, 25).
This study is limited in that the analyses were done retrospectively and only 52 patients were analyzed for the effects of surgery on insulin sensitivity and β-cell function. In addition, changes in insulin sensitivity and insulin secretion were not observed over the course of time. Thus, a longitudinal prospective study with long-term follow-up is required.
In summary, both insulin sensitivity and β-cell function decreased in diabetic acromegalic patients. Insulin sensitivity and the functionality of the pancreas, as measure by the DI, improved after the tumor resection. Thus, we conclude that both insulin sensitivity and β-cell function are improved by a decrease in excess GH, which contribute to improvements in glucose status after tumor resection in acromegalic patients.
Figures and Tables
Fig. 1
Results of the 75 g oral glucose tolerance test according to glucose status for 52 acromegalic patients.

Fig. 2
Insulin sensitivity index and β-cell function index between the diabetic, pre-diabetic, and normal glucose tolerance groups among 52 acromegalic patients. (A) ISI0,120, (B) HOMA-IR, (C) HOMA-β, (D) first phase of insulin secretion and (E) disposition index in the NGT, pre-diabetic and diabetic groups. Analysis was performed by the Kruskal-Wallis test. Data are the mean ± SD. NGT, normal glucose tolerance; NS, not significant.

Fig. 3
Change in glucose status, insulin sensitivity and β-cell function after tumor resection: (A) glucose status, (B) HOMA-IR, (C) ISI0,120, (D) HOMA-β, (E) first-phase insulin secretion, (F) second-phase insulin secretion and (G) disposition index. NGT, normal glucose tolerance; NS, not significant. Analysis was performed by Wilcoxon's signed rank test.

References
1. Kreze A, Kreze-Spirova E, Mikulecky M. Risk factors for glucose intolerance in active acromegaly. Braz J Med Biol Res. 2001. 34:1429–1433.
2. Espinosa-de-los-Monteros AL, González B, Vargas G, Sosa E, Mercado M. Clinical and biochemical characteristics of acromegalic patients with different abnormalities in glucose metabolism. Pituitary. 2011. 14:231–235.
3. Biering H, Knappe G, Gerl H, Lochs H. Prevalence of diabetes in acromegaly and Cushing syndrome. Acta Med Austriaca. 2000. 27:27–31.
4. Beck P, Schalch DS, Parker ML, Kipnis DM, Daughaday WH. Correlative studies of growth hormone and insulin plasma concentrations with metabolic abnormalities in acromegaly. J Lab Clin Med. 1965. 66:366–379.
5. Trimble ER, Atkinson AB, Buchanan KD, Hadden DR. Plasma glucagon and insulin concentrations in acromegaly. J Clin Endocrinol Metab. 1980. 51:626–631.
6. Foss MC, Saad MJ, Paccola GM, Paula FJ, Piccinato CE, Moreira AC. Peripheral glucose metabolism in acromegaly. J Clin Endocrinol Metab. 1991. 72:1048–1053.
7. Wasada T, Aoki K, Sato A, Katsumori K, Muto K, Tomonaga O, Yokoyama H, Iwasaki N, Babazono T, Takahashi C, Iwamoto Y, Omori Y, Hizuka N. Assessment of insulin resistance in acromegaly associated with diabetes mellitus before and after transsphenoidal adenomectomy. Endocr J. 1997. 44:617–620.
8. Møller N, Schmitz O, Jøorgensen JO, Astrup J, Bak JF, Christensen SE, Alberti KG, Weeke J. Basal- and insulin-stimulated substrate metabolism in patients with active acromegaly before and after adenomectomy. J Clin Endocrinol Metab. 1992. 74:1012–1019.
9. Kasayama S, Otsuki M, Takagi M, Saito H, Sumitani S, Kouhara H, Koga M, Saitoh Y, Ohnishi T, Arita N. Impaired beta-cell function in the presence of reduced insulin sensitivity determines glucose tolerance status in acromegalic patients. Clin Endocrinol (Oxf). 2000. 52:549–555.
10. Kinoshita Y, Fujii H, Takeshita A, Taguchi M, Miyakawa M, Oyama K, Yamada S, Takeuchi Y. Impaired glucose metabolism in Japanese patients with acromegaly is restored after successful pituitary surgery if pancreatic {beta}-cell function is preserved. Eur J Endocrinol. 2011. 164:467–473.
11. Coculescu M, Niculescu D, Lichiardopol R, Purice M. Insulin resistance and insulin secretion in non-diabetic acromegalic patients. Exp Clin Endocrinol Diabetes. 2007. 115:308–316.
12. Stelmachowska-Banaś M, Zdunowski P, Zgliczynski W. Abnormalities in glucose homeostasis in acromegaly. Does the prevalence of glucose intolerance depend on the level of activity of the disease and the duration of the symptoms? Endokrynol Pol. 2009. 60:20–24.
13. American Diabetes Association. Standards of medical care in diabetes: 2010. Diabetes Care. 2010. 33:S11–S61.
14. Phillips DI, Clark PM, Hales CN, Osmond C. Understanding oral glucose tolerance: comparison of glucose or insulin measurements during the oral glucose tolerance test with specific measurements of insulin resistance and insulin secretion. Diabet Med. 1994. 11:286–292.
15. Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC. Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia. 1985. 28:412–419.
16. Gutt M, Davis CL, Spitzer SB, Llabre MM, Kumar M, Czarnecki EM, Schneiderman N, Skyler JS, Marks JB. Validation of the insulin sensitivity index (ISI(0,120)): comparison with other measures. Diabetes Res Clin Pract. 2000. 47:177–184.
17. Bergman RN, Ader M, Huecking K, Van Citters G. Accurate assessment of beta-cell function: the hyperbolic correction. Diabetes. 2002. 51:S212–S220.
18. Stumvoll M, Mitrakou A, Pimenta W, Jenssen T, Yki-Järvinen H, Van Haeften T, Renn W, Gerich J. Use of the oral glucose tolerance test to assess insulin release and insulin sensitivity. Diabetes Care. 2000. 23:295–301.
19. Choi YJ, Kim HC, Kim HM, Park SW, Kim J, Kim DJ. Prevalence and management of diabetes in Korean adults: Korea National Health and Nutrition Examination Surveys 1998-2005. Diabetes Care. 2009. 32:2016–2020.
20. Jaffrain-Rea ML, Moroni C, Baldelli R, Battista C, Maffei P, Terzolo M, Correra M, Ghiggi MR, Ferretti E, Angeli A, Sicolo N, Trischitta V, Liuzzi A, Cassone R, Tamburrano G. Relationship between blood pressure and glucose tolerance in acromegaly. Clin Endocrinol (Oxf). 2001. 54:189–195.
21. Puder JJ, Nilavar S, Post KD, Freda PU. Relationship between disease-related morbidity and biochemical markers of activity in patients with acromegaly. J Clin Endocrinol Metab. 2005. 90:1972–1978.
22. Nielsen JH, Galsgaard ED, Møldrup A, Friedrichsen BN, Billestrup N, Hansen JA, Lee YC, Carlsson C. Regulation of beta-cell mass by hormones and growth factors. Diabetes. 2001. 50:S25–S29.
23. Rosenfalck AM, Maghsoudi S, Fisker S, Jørgensen JO, Christiansen JS, Hilsted J, Vølund AA, Madsbad S. The effect of 30 months of low-dose replacement therapy with recombinant human growth hormone (rhGH) on insulin and C-peptide kinetics, insulin secretion, insulin sensitivity, glucose effectiveness, and body composition in GH-deficient adults. J Clin Endocrinol Metab. 2000. 85:4173–4181.
24. Hansen I, Tsalikian E, Beaufrere B, Gerich J, Haymond M, Rizza R. Insulin resistance in acromegaly: defects in both hepatic and extrahepatic insulin action. Am J Physiol. 1986. 250:E269–E273.
25. Muggeo M, Bar RS, Roth J, Kahn CR, Gorden P. The insulin resistance of acromegaly: evidence for two alterations in the insulin receptor on circulating monocytes. J Clin Endocrinol Metab. 1979. 48:17–25.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download