Abstract
The platelet-rich plasma (PRP) has been advocated as a way to introduce increased concentrations of growth factors and other bioactive molecules to injured tissues in an attempt to optimize the local healing environment. A 94-yr-old woman with various comorbidities presented with a two-week history of severe cutaneous ulcer on the left dorsum of foot. It was caused by recurrent mechanical trauma and did not respond to several wound debridement and simple dressings. However, after she was completed on seven times of autologous PRP treatments, we observed complete healing of the skin lesion within 3 months. Herein, we report a case of recalcitrant cutaneous ulcer with various comorbidities and discuss about the promising possibility of autologous PRP as an effective alternative therapeutic modality.
In recent years the problem of "cutaneous ulcers" (venous, arterial, diabetic, and pressure sores) has become increasingly important, in particular because of the progressive increase in the elderly population and, therefore, of chronic disorders (1). Chronic cutaneous ulcers of the comorbid elderly patient tend to resist on standard therapy and therefore the management is difficult, time-consuming and expensive (2). Optimally, a short period of advanced therapy to stimulate healing can result in the transition of an intractable wound to a treatable one, which can then be treated with less expensive, standard care (3).
Platelet-rich plasma (PRP) is an autologous preparation of platelets in concentrated plasma and contains various growth factors. Due to the presence of high concentrations of these growth factors, PRP has been used in a wide variety of surgical procedures and clinical treatments (4).
We herein report a comorbid patient with refractory cutaneous ulcer which did not respond to formal therapeutic methods. The patient was treated with autologous PRP and could achieve complete response of the skin lesion within 3 months.
On November 25, 2011, a 94 yr-old woman was referred for the management of erythematous to violaceous patches with bullae on dorsum of left foot. She repeatedly hit her left foot in which intravenous line was situated with the opposite side for days. She had a various underlying disease including Alzheimer's dementia, angina pectoris, type 2 diabetes, hypertension, chronic kidney disease (stage IV) and was in a bed ridden state. Because of the poor oral intake and noncompliance to the Levin-tube, the percutaneous endoscopic gastrostomy tube had been inserted on her abdomen and only minimal amount of nutrition was maintained.
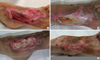
Despite of the daily simple dressing and intermittent debridement about 2 weeks, the status of the wound was deteriorated and advanced to painful ulcerative patches with eschar and granulation tissues (Fig. 1A). The results of the bacterial culture and gram stain were negative.
Autologous PRP were prepared for the alternative management of her worsening wound. 12 mL peripheral autologous blood was obtained and collected into tubes containing acid-citrate-dextrose solution formula (ACD-A) anticoagulant. The citrated blood was centrifuged for 7 min at 2,500 rpm. Subsequently, the yellow plasma (containing buffy coat with platelets) was separated from other components. The upper 3 to 4 mL plasma called platelet poor plasma was removed by micropipette. The remnant PRP was extracted by sleeve filter and mixed with CaCl2. Finally, The CaCl2-activated PRP was topically applied to the ulcerative wound.
The patient underwent a total of 7 PRP treatments over a span of 8 weeks (performed twice a week until 5th treatment and then weekly until 7th treatment). As described above, these treatments involved topically application of activated PRP as well as packing of the wound with aseptic film for the sustained effect of growth factors. The film was removed on next day and the top layer was covered with hydrofoam dressing material until subsequent PRP treatment.
Over the course of the PRP treatment, the wound became noticeably vascularized and filled with granulation tissue. The results of the changes in wound surface area and depth are shown in Fig. 1B-D. The wound was essentially filled in with granulation tissue after seven PRP treatments with only subtle epithelialization of the new tissue remaining. There were neither signs of infection and allergic reaction nor discomfort of the patient during the treatment. After 2 months from the last (7th) treatment, the complete epithelialization was seen and no further simple dressing was required for the wound.
The complete response of the recalcitrant cutaneous ulcer using PRP therapies implies that this stimulation therapy could be an appropriate alternative modality when the degree of healing with conventional treatment appears to be unsatisfactory. The ulcer bed more rapidly demonstrated margin in-growth, granulation tissue development, vascularization and epithelialization (5, 8). These regenerative actions of PRP are the result of three main components. First of all, the growth factors and cytokines released from PRP are able to stimulate the proliferation, migration and differentiation of dermal fibroblasts and endothelial cells. PRP also increased type I collagen and MMPs gene expression, suggesting that PRP also have the potential to promote the tissue remodeling of aged skin (4). The second component is the mesh of fibrin that constitutes the "structure" of the platelet gel: this mesh forms a biological scaffold that helps and guides the migration of the mesenchymal cells, derived from populations of resident stem cells or circulating precursors, from the base and the margins of the wound. The third component is the antibacterial properties of the factors released by the platelets and, probably, by the leucocytes contained in the PRP (1).
On the basis of these molecular understandings, PRP therapy has been successfully used in the treatment of various dermatological defect including pressure ulcer (1, 5), diabetic ulcer (1, 2, 6) vascular ulcers, post-traumatic ulcers (1) and lipodermatosclerosis (7). However, a few studies have reported in the treatment of severe cutaneous ulcers associated with old age, hypomobility and many underlying diseases (2, 9).
This report showed the favorable outcome of the refractory cutaneous ulcer using autologous PRP. Although further studies are required for better understandings of the mechanism, efficacy, and safety of autologous PRP therapy, it could be considered as an effective alternative option for the recalcitrant cutaneous ulcer with various comorbidities.
Figures and Tables
Fig. 1
Initial presentation and subsequent changes of cutaneous ulcer according to autologous PRP treatments. (A) Painful ulcerative patches with eschar and granulation tissues on left dorsum of foot before the 1st PRP treatment on 2011.12.09, (B) at 5th application of PRP on 2011.12.23, (C) at 7th application of PRP on 2012.02.07 and (D) 2 months after the last (7th) PRP on 2012.04.17.
References
1. Bernuzzi G, Tardito S, Bussolati O, Adorni D, Cantarelli S, Fagnoni F, Rossetti A, Azzarone M, Ficarelli E, Caleffi E, et al. Platelet gel in the treatment of cutaneous ulcers: the experience of the immunohaematology and Transfusion Center of Parma. Blood Transfus. 2010. 8:237–247.
2. Orcajo B, Muruzabal F, Isasmendi MC, Gutierrez N, Sanchez M, Orive G, Anitua E. The use of plasma rich in growth factors in the treatment of a severe mal perforant ulcer in the foot of a person with diabetes. Diabetes Res Clin Pract. 2011. 93:e65–e67.
3. De Leon JM, Driver VR, Fylling CP, Carter MJ, Anderson C, Wilson J, Dougherty RM, Fuston D, Trigilla D, Valenski V, et al. The clinical relevance of treating chronic wounds with an enhanced near-physiological concentration of platelet-rich plasma gel. Adv Skin Wound Care. 2011. 24:357–368.
4. Kim DH, Je YJ, Kim CD, Lee YH, Seo YJ, Lee JH, Lee Y. Can platelet-rich plasma be used for skin rejuvenation? Evaluation of effects of platelet-rich plasma on human dermal fibroblast. Ann Dermatol. 2011. 23:424–431.
5. Sell SA, Ericksen JJ, Reis TW, Droste LR, Bhuiyan MB, Gater DR. A case report on the use of sustained release platelet-rich plasma for the treatment of chronic pressure ulcers. J Spinal Cord Med. 2011. 34:122–127.
6. Villela DL, Santos VL. Evidence on the use of platelet-rich plasma for diabetic ulcer: a systemic review. Growth Factors. 2010. 28:111–116.
7. Jeong KH, Shin MK, Kim NI. Refractory lipodermatosclerosis treated with intralesional platelet-rich plasma. J Am Acad Dermatol. 2011. 65:e157–e158.
8. Pallua N, Wolter T, Markowicz M. Platelet-rich plasma in burns. Burns. 2010. 36:4–8.
9. Greppi N, Mazzucco L, Galetti G, Bona F, Petrillo E, Smacchia C, Raspollini E, Cossovich P, Caprioli R, Borzini P, et al. Treatment of recalcitrant ulcers with allogenic platelet gel from pooled platelets in aged hypomobile patients. Biologicals. 2011. 39:73–80.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download