Abstract
The demographics and prognosis of non-small cell lung cancer patients have changed during the last few decades. We conducted this study to assess the change in demographics and prognosis in resected non-small cell lung cancer patients during a 20-yr single-institution study in Korea. We retrospectively reviewed the medical records of 2,076 non-small cell lung cancer patients who underwent pulmonary resection between 1990 and 2009. Their clinical characteristics and survival were analyzed over a five-year period. With time, the proportions of female, adenocarcinoma, stage IA, and lobectomy patients increased, whereas the proportions of male, squamous cell carcinoma, stage IIIA, and pneumonectomy patients decreased. These demographic changes caused improved prognosis. The five-year survival rate of all patients was 53.9%. The five-year survival rate increased from 31.9% in 1990-1994, to 43.6% in 1995-1999, 51.3% in 2000-2004, and 69.7% in 2005-2009 (P < 0.001). In conclusion, among patients with resected non-small cell lung cancer, the proportions of female, adenocarcinoma, stage IA, and lobectomy patients have increased, and the five-year survival rate has gradually improved during the last 20 yr in Korea.
Lung cancer is the leading cause of cancer deaths in the Western world as well as in Korea (1-3). Non-small cell lung cancer (NSCLC) constitutes more than 80% of lung cancer cases, and surgery remains the only potentially curative treatment for early stage lung cancer. During the last few decades, the clinical profile of NSCLC patients who are candidates for surgical resection has changed dramatically. According to the Japanese Joint Committee for Lung Cancer Registration (JJCLCR), the proportions of patients who are female, have stage IA disease, and have adenocarcinoma have increased, and the five-year survival rate has gradually improved from 47.2% in 1989, to 52.6% in 1994, to 61.4% in 1999, and to 69.6% in 2004 (4-7). As such, it is important to understand the demographics, tumor-related background, and the prognosis by related factors and stage. In addition, determining trends in those parameters will be helpful in developing nation-specific strategies for lung cancer treatment. In this study, we analyzed 20 yr of single-institution data to identify the recent surgical outcomes and trends related to non-small cell lung cancer surgery in Korea.
We reviewed the records of 2,076 patients with NSCLC who underwent pulmonary resection at our institute from January 1990 to December 2009. Pathological staging was based on the 2009 TNM classification system (8). Tumor histology was categorized according to the World Health Organization classification. Lymph node status was assessed according to the system defined by Mountain and Dresler (9). Lobectomy and systematic lymph node dissection were the procedures of choice, regardless of clinical stage. Patients with stage I-IIIA disease were indicated for surgical resection. All patients were followed either until death or the last follow-up date (December 1, 2011).
The duration of survival was defined as the interval between the date of surgery and either the date of death or the last follow-up date. Survival curves were estimated using the Kaplan-Meier method, and differences in survival were assessed by the log-rank test. In the analysis of pathologic stage and survival, the patients (n = 169) who received induction treatment were excluded. A P value less than 0.05 was considered significant. The data were analyzed using SPSS for Windows (Statistical Package for the Social Sciences, SPSS Inc. Chicago, IL, USA).
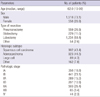
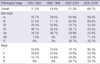
The 2,076 patients included 558 females and 1,518 males with a median age of 62 yr (range, 10 to 90 yr). The median follow-up time was 37.3 months (range, 0 to 261.9 months). All patient characteristics are summarized in Table 1. The overall five-year survival rate was 53.9%. The five-year survival rate was 85.6% for stage IA, 71.7% for IB, 48.4% for IIA, 46.2% for IIB, 33.1% for IIIA, 5.2% for stage IIIB, and 17.1% for stage IV.
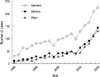
In the time period from 1990 to 2009, the proportion of patients with pathologic stage I disease increased from 16.6% (5/30) in 1990 to 58.2% (131/225) in 2009. In terms of lung cancer subtype, the proportion of adenocarcinomas increased annually from 33.3% (10/30) in 1990 to 64.0% (144/225) in 2009 (Fig. 1), while the proportion of squamous cell carcinomas decreased annually from 56.6% (17/30) in 1990 to 30.2% (68/225) in 2009. This shift in the distribution of tumor subtypes was prominent after the mid-2000s.
Patients were divided into the following four groups based on their year of surgery: 1990-1994, 1995-1999, 2000-2004, and 2005-2009. The mean age of the patients at the time of the operation increased over time. The proportions of female, adenocarcinoma, lobectomy, and pathologic stage Ia patients increased. The proportions of male, squamous histology, pneumonectomy and stage IIIa patients decreased over time (Table 2).
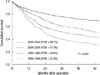
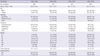
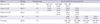
The overall five-year survival rate of all patients was 53.9%. The overall survival rate improved over time, increasing from 31.9% in 1990-1994, to 43.6% in 1995-1999, to 51.3% in 2000-2004, and to 69.7% in 2005-2009 (P < 0.001, Fig. 2). This tendency was similar for every pathologic stage. The five-year survival rate increased from 85.7% in 1990-1995 to 89.2% in 2005-2009 for stage IA, from 57.5% to 83.6% for stage IB, from 25.0% to 55.3% for stage IIA, from 48.1% to 49.5% for stage IIB, from 16.3% to 53.9% for stage IIIA, from 7.1% to 11.5% for IIIB, and from 0% to 32.7% for stage IV (Table 3).
The demographics and prognoses of non-small cell lung cancer patients undergoing surgery at a single Korean institution have changed over the last 20 yr. The proportions of patients who are female, underwent lobectomy, have stage IA disease, and have adenocarcinoma have increased, and the five-year survival rate has gradually improved from 31.9% in 1990-1994 to 43.6% in 1995-1999, to 51.3% in 2000-2004, and to 69.7% in 2005-2009.
The lung cancer incidence in Western countries (North America, Western Europe, Australia) has stabilized over the past decades (10). However, there have been major shifts in the frequencies of the various histological types of lung cancer, with significant increases in the incidence of adenocarcinoma, and a corresponding decrease in the incidence of squamous cell cancer. For example, registry data from the USA indicated that the ratio of squamous carcinomas to adenocarcinomas was approximately 17:1, and by 1995 these two histological types of cancer were nearly equal in incidence. Although lung cancer data are not extensively available for Asian populations, the same pattern of change has been observed (11). In Taiwan, a study of over 10,000 cases over the period from 1970 to 1993 showed that the incidence of squamous carcinoma decreased from 46.4% to 36.2% in men, whereas adenocarcinoma increased from 30% to 36% in men and from 50.7% to 64.8% in women, such that adenocarcinoma has now become the most common cancer cell type (12). Similar patterns were found in Singapore, Korea, Hong Kong and Japan (13-16). This study also showed a similar pattern with surgically resected lung cancer cases and this shift in the distribution of cancer types was prominent after the mid-2000s (Fig. 1).
The prognosis of surgical resection of NSCLC was not promising. Despite "curative resection," more than 70% of patients with NSCLC in one study experienced recurrence (17). The five-year survival rate after resection was 42.6% according to Naruke et al. (18) and 41.4% according to van Rens et al. (19). However, it is not surprising that postoperative survival is changing with each decade based on the date of resection, histology, and the distribution of stages.
There have been a few reports focusing on the change in surgical results over time (Table 4). Koike et al. (20) divided the dates of resection into three periods and reported that the proportion of stage IA cases increased and that the five-year survival rate improved over time (33.7% in 1963-1977, 51.8% in 1978-1986, and 58.4% in 1987-1992). Fang and coworkers (21) compared the NSCLC surgical results from four periods: 1960s, 1970s, 1980s, and 1990s. They reported that the five-year survival rate improved with some influencing factors, such as the rate of postoperative complications, lymph node dissection, and combination therapy. Yoshino and coworkers (22) compared the surgical results for NSCLC resected in the three decades from 1975 to 1998 and reported that the five-year survival rates improved (30.3% in the 1970s, 41.6% in the 1980s, and 50.1% in the 1990s) due to an increasing number of female patients with adenocarcinoma, more frequent detection of early disease, and effective elimination of unresectable cases.
The Japanese Joint Committee for Lung Cancer Registration (JJCLCR) reported that the proportions of patients who are female, have stage IA disease, and have adenocarcinoma have increased, and the five-year survival rate has gradually improved, from 47.2% in 1989, to 52.6% in 1994, to 61.4% in 1999, and to 69.6% in 2004 (4-7). In this study, the postoperative five-year survival rate in Korea improved from 31.9% in 1990-1994, to 43.6% in 1995-1999, to 51.3% in 2000-2004, and to 69.7% in 2005-2009, mainly due to increased proportions of female patients, pathologic stage IA cases and decreased pneunonectomy cases. The prognosis for this surgical result is similar to that in the JJCLCR reports, and has changed more dramatically due to the prominent change in demographics after the mid-2000s. The recent favorable surgical outcomes including those presented by the JJCLCR and in this report suggest that good surgical results for NSCLC have been achieved.
With regard to the change in the five-year survival rate according to sub-staging groups, the data are not sufficient to fully evaluate the prognosis of all stages in each period due to the relatively small number of cases from our single institution. However, the trend of improvement in survival rate was noted in all subgroups. This improvement in each stage is likely due to a decreased mean tumor size (from 4.5 cm in 1990-1994 to 3.4 cm in 2005-2009), decreased proportion of pneumonectomy cases, standardization of adjuvant chemotherapy, increased proportion of female patients, and increased proportion of adenocarcinoma, which is a good target for recently developed chemotherapy.
To the best of our knowledge, this is the first report from Korea assessing the recent trends in demographics and prognoses for resected NSCLC cases. In conclusion, the clinical profiles of resected non-small cell lung cancer have changed in the last 20 years in Korea. The proportions of female, stage IA, lobectomy, and adenocarcinoma patients have increased, and the five-year survival rate has gradually improved from 31.9% in 1990-1994, to 43.6% in 1995-1999, to 51.3% in 2000-2004, and to 69.7% in 2005-2009.
Figures and Tables
Fig. 1
Number of NSCLC patients with resection, adenocarcinoma and stage I according to time. The proportion of patients with pathologic stage I disease and adenocarcinoma increased from 16.6% (5/30) and 33.3% (10/30), respectively, in 1990 to 58.2% (131/225) and 64.0% (144/225), respectively, in 2009 (NSCLC: non-small cell lung cancer).
ACKNOWLEDGMENT
All the work was performed at the Yonsei University College of Medicine, Seoul, Korea. The authors do not have actual or potential conflicts of interest.
References
1. Jemal A, Siegel R, Xu J, Ward E. Cancer statistics, 2010. CA Cancer J Clin. 2010. 60:277–300.
2. National Cancer Information center. Cancer statistics, 2009. accessed on December 30, 2011. Available at http://www.cancer.go.kr/ncic/cics_f/02/022/index.html.
3. Jung KW, Park S, Kong HJ, Won YJ, Boo YK, Shin HR, Park EC, Lee JS. Cancer statistics in Korea: incidence, mortality, survival, and survival in 2006-2007. J Korean Med Sci. 2010. 25:1113–1121.
4. Shirakusa T. Postoperative results under the new stage classification of lung cancer: the additional reports for those of JACS in 1996. Kyobu Geka. 2000. 53:894–898.
5. Goya T, Asamura H, Yoshimura H, Kato H, Shimokata K, Tsuchiya R, Sohara Y, Miya T, Miyaoka E. Japanese Joint Committee of Lung Cancer Registry. Prognosis of 6644 resected non-small cell lung cancers in Japan: a Japanese lung cancer registry study. Lung Cancer. 2005. 50:227–234.
6. Asamura H, Goya T, Koshiishi Y, Sohara Y, Eguchi K, Mori M, Nakanishi Y, Tsuchiya R, Shimokata K, Inoue H, et al. A Japanese Lung Cancer Registry study: prognosis of 13,010 resected lung cancers. J Thorac Oncol. 2008. 3:46–52.
7. Sawabata N, Miyaoka E, Asamura H, Nakanishi Y, Eguchi K, Mori M, Nomori H, Fujii Y, Okumura M, Yokoi K. Japanese Joint Committee for Lung Cancer Registration. Japanese Lung Cancer Registry Study of 11,663 surgical cases in 2004: demographic and prognosis changes over decade. J Thorac Oncol. 2011. 6:1229–1235.
8. Goldstraw P, Crowley J, Chansky K, Giroux DJ, Groome PA, Rami-Porta R, Postmus PE, Rusch V, Sobin L. International Association for the Study of Lung Cancer International Staging Committee. Participating Institutions. The IASLC Lung Cancer Staging Project: proposals for the revision of the TNM stage groupings in the forthcoming (seventh) edition of the TNM Classification of malignant tumours. J Thorac Oncol. 2007. 2:706–714.
9. Mountain CF, Dresler CM. Regional lymph node classification for lung cancer staging. Chest. 1997. 111:1718–1723.
10. Devesa SS, Bray F, Vizcaino AP, Parkin DM. International lung cancer trends by histologic type: male: female differences diminishing and adenocarcinoma rates rising. Int J Cancer. 2005. 117:294–299.
11. Lam WK, White NW, Chan-Yeung MM. Lung cancer epidemiology and risk factors in Asia and Africa. Int J Tuberc Lung Dis. 2004. 8:1045–1057.
12. Perng DW, Perng RP, Kuo BI, Chiang SC. The variation of cell type distribution in lung cancer: a study of 10,910 cases at a medical center in Taiwan between 1970 and 1993. Jpn J Clin Oncol. 1996. 26:229–233.
13. Seow A, Duffy SW, Ng TP, McGee MA, Lee HP. Lung cancer among Chinese females in Singapore 1968-1992: time trends, dialect group differences and implications for aetiology. Int J Epidemiol. 1998. 27:167–172.
14. Choi JH, Chung HC, Yoo NC, Lee HR, Lee KH, Choi W, Lim HY, Koh EH, Kim JH, Roh JK. Changing trends in histologic types of lung cancer during the last decade (1981-1990) in Korea: a hospital-based study. Lung Cancer. 1994. 10:287–296.
15. Lam KY, Fu KH, Wong MP, Wang EP. Significant changes in the distribution of histologic types of lung cancer in Hong Kong. Pathology. 1993. 25:103–105.
16. Morita T. A statistical study of lung cancer in the annual of pathological autopsy cases in Japan, from 1958 to 1997, with reference to time trends of lung cancer in the world. Jpn J Cancer Res. 2002. 93:15–23.
17. Westeel V, Choma D, Clément F, Woronoff-Lemsi MC, Pugin JF, Dubiez A, Depierre A. Relevance of an intensive postoperative follow-up after surgery for nonsmall cell lung cancer. Ann Thorac Surg. 2000. 70:1185–1190.
18. Naruke T, Tsuchiya R, Kondo H, Asamura H. Prognosis and survival after resection for bronchogenic carcinoma based on the 1997 TNM-staging classification: the Japanese experience. Ann Thorac Surg. 2001. 71:1759–1764.
19. van Rens MT, de la Rivière AB, Elbers HR, van Den Bosch JM. Prognostic assessment of 2,361 patients who underwent pulmonary resection for non-small cell lung cancer, stage I, II, and IIIA. Chest. 2000. 117:374–379.
20. Koike T, Terashima M, Takizawa T, Haga M, Kurita Y, Yokoyama A, Misawa H. The influence of lung cancer mass screening on surgical results. Lung Cancer. 1999. 24:75–80.
21. Fang D, Zhang D, Huang G, Zhang R, Wang L, Zhang D. Results of surgical resection of patients with primary lung cancer: a retrospective analysis of 1,905 cases. Ann Thorac Surg. 2001. 72:1155–1159.
22. Yoshino I, Baba H, Fukuyama S, Kameyama T, Shikada Y, Tomiyasu M, Suemitsu R. A time trend of profile and surgical results in 1,123 patients with non-small cell lung cancer. Surgery. 2002. 131:S242–S248.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download