Abstract
We evaluated risk factors for neutropenic fever and febrile prolonged neutropenia during vincristine-including chemotherapy to treat HIV-related lymphoma to investigate whether protease inhibitor (PI) treatment is associated with infectious complications due to drug interactions with chemotherapeutic agents. We included all HIV patients who received chemotherapy including vincristine for lymphoma at a single referral center in 1999-2010. Neutropenic fever was defined as absolute neutrophil count < 500 cells/µL with body temperature over 38℃; and prolonged neutropenia was defined if it persisted over 7 days. CODOX-M/IVAC and Stanford regimens were considered high-risk regimens for prolonged neutropenia. We analyzed 48 cycles of chemotherapy in 17 HIV patients with lymphoma. There were 22 neutropenic fever and 12 febrile prolonged neutropenia events. In multivariate analysis, neutropenic fever was associated with old age and low CD4 cell count, but not with PI use or ritonavir-boosted PI use. Low CD4 cell count and high-risk regimens were associated with febrile prolonged neutropenia. Neutropenic fever and febrile prolonged neutropenia is associated with old age, low CD4 cell count, and high-risk regimens, but not PI use, in HIV patients undergoing chemotherapy including vincristine for lymphoma.
Lymphoma is an important malignancy in the morbidity and mortality of HIV patients, although its incidence began to decrease after the introduction of combined antiretroviral therapy (1). HIV patients may be more susceptible than non-HIV patients to infectious complications following chemotherapy for lymphoma. However, risk factors for infectious complications with neutropenia after chemotherapy have not been well defined in HIV patients with lymphoma.
Protease inhibitors (PIs) may be associated with febrile neutropenia via interactions with vinca alkaloid-based drugs in chemotherapy regimens for lymphoma, because vinca alkaloid is the substrate for cytochrome P450 3A4 isoenzyme, and PIs are potent inhibitors of this isoenzyme (2). The results of some studies suggest that vinblastine may cause severe neutropenia by interacting with PIs (3-5). However, there are no data about risk factors for neutropenic complications in HIV patients receiving a vincristine-containing regimen for lymphoma. Furthermore, there is controversy as to whether PI use should be avoided in HIV patients receiving chemotherapy for lymphoma.
The purpose of this study was to evaluate risk factors for neutropenic fever and febrile prolonged neutropenia in HIV patients receiving chemotherapy including vincristine for lymphoma.
We retrospectively identified all HIV patients who received chemotherapy with a vincristine-containing regimen for lymphoma from 1999 through 2010 in Seoul National University Hospital (Korea), a 1,500-bed tertiary-care university hospital. Antiretroviral regimens were determined independently by attending physicians. The PIs used were lopinavir/ritonavir, atazanavir, and nelfinavir. Other antiretroviral drugs used were the nonnucleoside reverse transcriptase inhibitor efavirenz and nucleoside analog reverse transcriptase inhibitors including lamivudine, stavudine, zidovudine, didanosine, and abacavir. Granulocyte colony-stimulating factor was not used routinely during chemotherapy.
Neutropenic fever was defined as absolute neutrophil count < 500 cells/µL on two occasions with axillary temperature over 38℃ for ≥ 1 hr. Prolonged neutropenia was defined if neutropenia persisted for ≥ 7 days (6-8). Severe neutropenia is defined as absolute neutrophil count < 100 cells/µL (9). Bone marrow involvement of lymphoma was defined as the presence of malignant lymphoma cells in bone marrow biopsy specimens.
Among the chemotherapeutic regimens, CODOX-M/IVAC (cyclophosphamide, doxorubicin, vincristine, methotrexate, leucovorin/ifosfamide, etoposide, and cytarabine) and the Stanford regimen (cyclophophamide, doxorubicin, vincristine, prednisone, L-asparaginase, and intrathecal methotrexate) were considered to be high-risk regimens for severe neutropenia. Mild-to-moderate regimens included C-MOPP (cyclophophamide, vincristine, procarbazine, and prednisone), COPBLAM (cyclophophamide, vincristine, prednisone, bleomycin, doxorubicin, and procarbazine), CHOP (cyclophosphamide, doxorubicin, vincristine, and prednisone), R-CHOP (rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisone), MOD (high-dose methotrexate, vincristine, and procarbazine), R-MOD (rituximab, high-dose methotrexate, vincristine, and procarbazine), and CVP (cyclophosphamide, vincristine, and prednisone).
CD4 cell counting was performed using whole blood stained with murine antihuman monoclonal antibodies to CD4 (Tetraone; Beckman Coulter, High Wycombe, UK). HIV viral load was measured in plasma using assays with a lower limit of detection of 50 HIV-1 copies/mL (Chron Diagnostics, Halstead, UK).
All statistical analyses were performed with SPSS software, version 19.0 (SPSS, Chicago, IL, USA). To identify risk factors associated with neutropenic fever and febrile illness with prolonged neutropenia, a generalized estimate equation was used, because of a possible clustering effect caused by patients receiving multiple cycles of chemotherapy. In univariate analysis, variables included age, CD4 cell count, high-risk regimen for severe neutropenia, bone marrow involvement of lymphoma, prophylactic use of trimethoprim/sulfamethoxazole, zidovudine use, and PI use. Multivariate models included variables for which the P value was < 0.1 in univariate analysis. P values of < 0.05 were considered statistically significant.
During the study period, there were 26 HIV patients with lymphoma. Of these, nine patients did not receive chemotherapy; three of these patients had Burkitt's lymphoma, two had diffuse large B cell lymphoma, one had plasmoblastic lymphoma, and three had primary central nervous system lymphoma. In the 17 HIV patients who received chemotherapy, we analyzed a total of 48 cycles of chemotherapy; eight of these patients had Burkitt's lymphoma, seven had diffuse large B cell lymphoma, one had Hodgkin's lymphoma, and one had T lymphoblastic lymphoma.
All of the patients were male, and the median age was 40 yr (interquartile range [IQR], 37-47 yr). The baseline median CD4 cell count was 181 cells/µL (IQR, 63-297 cells/µL). Eleven (41%) patients received antiretroviral therapy with PI-based regimens. The stage of lymphoma was as follows; four patients with stage I lymphoma, two with stage III and ten with stage IV, respectively (Table 1).
There were 22 (46%) events of neutropenic fever and 12 (25%) of febrile prolonged neutropenia (range, 7-15 days). Univariate analyses revealed that febrile neutropenia was associated with old age, low CD4 cell counts, and high-risk regimens, and febrile prolonged neutropenia was associated with low CD4 cell counts and high-risk regimens (Table 2). Use of zidovudine or trimethoprim/sulfamethoxazole or bone marrow involvement of lymphoma was not associated with neutropenic fever or febrile prolonged neutropenia (data not shown).
Multivariate analyses revealed that neutropenic fever was associated with old age (adjusted odds ratio [aOR], 2.03; 95% confidence interval [CI], 1.41-2.92) and low CD4 cell count (aOR 0.95; 95% CI, 0.91-1.00), while it was not associated with PI use (aOR, 0.84; 95% CI, 0.37-1.94) or ritonavir-boosted PI use (aOR 1.34; 95% CI, 0.50-3.61). Low CD4 cell count (aOR, 1.06; 95% CI, 1.01-1.12) and high-risk regimens (aOR 46.9; 95% CI, 4.22-521.89) were associated with febrile illness with prolonged neutropenia.
In this study, old age and a low CD4 cell count were risk factors for the development of neutropenic fever in HIV patients receiving chemotherapy including vincristine for lymphoma. In addition, low CD4 cell counts and high-risk chemotherapeutic regimens for severe neutropenia were associated with febrile illness with prolonged neutropenia.
To our knowledge, this is the first study to evaluate risk factors for neutropenic complications in HIV patients receiving chemotherapy for lymphoma. The results of this study, which focused on the effect of drug interactions between vincristine and PIs, suggest that it is not always necessary to avoid PI treatment during chemotherapy including vincristine for lymphoma, because PI use was neither associated with neutropenic fever nor with febrile, prolonged neutropenia.
There are several factors that could explain why this study did not find any association between PI use and neutropenia during chemotherapy including vincristine, despite theoretical interactions between PI and vincristine. First, chemotherapeutic agents other than vincristine may have complex interaction with antiretroviral agents, including PIs. The toxicity of some chemotherapeutic agents such as ifosfamide and doxorubicin may be decreased by interactions with PIs, while the toxicity of other agents like vincristine and etoposide may increase with concomitant use of PIs (10). The effect of interactions between PI and vincristine could be tempered by complex interactions of the other chemotherapeutic agents with PI. Second, because this study included diverse chemotherapeutic regimens for several classes of lymphoma, differences among the chemotherapeutic regimens could influence the study results. Classifying the chemotherapeutic regimens into high- or low-to-moderate risk regimens may be an oversimplification. Finally, the patient number in this study might be too small to detect the effects of interactions between PIs and chemotherapeutic agents.
In our study, a low CD4 cell count was associated with the development of both neutropenic fever and febrile prolonged neutropenia during chemotherapy for lymphoma in HIV patients. There was a similar report of a correlation between a low CD4 cell count and the risk of chemotherapy toxicity in HIV-positive patients with cancer before the introduction of combined antiretroviral therapy (11). In one report, a CD4 cell count of < 450/µL was an independent risk factor for febrile neutropenia and early death due to infection in patients receiving chemotherapy (12).
The type and intensity of the chemotherapy regimen is also an important factor associated with the development of neutropenic events (13, 14). Our data also showed that regimens associated with a high risk for severe neutropenia were a significant risk factor for febrile illness with prolonged neutropenia. In the present study, old age was another risk factor for neutropenic fever following chemotherapy for lymphoma. This finding can be partly explained by the fact that older patient is generally more susceptible to infection.
This study has some limitations. First, a small number of the patients at a single center were included. Second, the diverse chemotherapeutic regimens used in several types of lymphoma might interfere with the conclusions. Finally, the antiretroviral regimens used could influence on the interaction between PI and chemotherapeutic agents.
In conclusion, neutropenic fever and febrile prolonged neutropenia is associated with old age, low CD4 cell count, and high-risk regimens, but not PI use, in HIV patients receiving chemotherapy including vincristine for lymphoma. Our findings suggest that more meticulous medical attention should be paid to neutropenic complications in HIV patients with these risk factors. This study does not support that the idea that PIs should be avoided routinely during chemotherapy for lymphoma.
Figures and Tables
Table 1
Clinical characteristics of 17 HIV patients with lymphoma
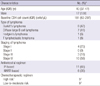
*Number (%) of patients unless otherwise indicated; †High-risk regimen for severe neutropenia included CODOX-M/IVAC and Stanford regimen; ‡Two patients underwent both high- and low-to-moderate risk regimens. IQR, interquartile range; PI, protease inhibitor; NNRTI, nonnucleoside reverse transcriptase inhibitor.
References
1. Bedimo R, Chen RY, Accortt NA, Raper JL, Linn C, Allison JJ, Dubay J, Saag MS, Hoesley CJ. Trends in AIDS-defining and non-AIDS-defining malignancies among HIV-infected patients: 1989-2002. Clin Infect Dis. 2004. 39:1380–1384.
2. Antoniou T, Tseng AL. Interactions between antiretroviral and antineoplastic drug therapy. Clin Pharmacokinet. 2005. 44:111–145.
3. Kotb R, Vincent I, Dulioust A, Peretti D, Taburet AM, Delfraissy JF, Goujard C. Life-threatening interaction between antiretroviral therapy and vinblastine in HIV-associated multicentric Castleman's disease. Eur J Haematol. 2006. 76:269–271.
4. Makinson A, Martelli N, Peyrière H, Turriere C, Le Moing V, Reynes J. Profound neutropenia resulting from interaction between antiretroviral therapy and vinblastine in a patient with HIV-associated Hodgkin's disease. Eur J Haematol. 2007. 78:358–360.
5. Martin P, Leonard JP, Coleman M, Furman RR. Durable complete remissions in HIV-associated Hodgkin lymphoma after treatment with only one cycle of chemotherapy complicated by sepsis. Clin Lymphoma Myeloma. 2009. 9:247–249.
6. Jun HX, Zhixiang S, Chun W, Reksodiputro AH, Ranuhardy D, Tamura K, Matsumoto T, Lee DG, Purushotaman SV, Lim V, et al. Clinical guidelines for the management of cancer patients with neutropenia and unexplained fever. Int J Antimicrob Agents. 2005. 26:S128–S132.
7. Bodey GP, Buckley M, Sathe YS, Freireich EJ. Quantitative relationships between circulating leukocytes and infection in patients with acute leukemia. Ann Intern Med. 1966. 64:328–340.
8. Lee DG, Kim SH, Kim SY, Kim CJ, Park WB, Song YG, Choi JH. Evidence-based guidelines for empirical therapy of neutropenic fever in Korea. Korean J Intern Med. 2011. 26:220–252.
9. Freifeld AG, Bow EJ, Sepkowitz KA, Boeckh MJ, Ito JI, Mullen CA, Raad II, Rolston KV, Young JA, Wingard JR. Infectious Diseases Society of America. Clinical practice guideline for the use of antimicrobial agents in neutropenic patients with cancer: 2010 Update by the Infectious Diseases Society of America. Clin Infect Dis. 2011. 52:427–431.
10. Spano JP, Costagliola D, Katlama C, Mounier N, Oksenhendler E, Khayat D. AIDS-related malignancies: state of the art and therapeutic challenges. J Clin Oncol. 2008. 26:4834–4842.
11. Ozer H, Armitage JO, Bennett CL, Crawford J, Demetri GD, Pizzo PA, Schiffer CA, Smith TJ, Somlo G, Wade JC, et al. American Society of Clinical Oncology Growth Factors Expert Panel. 2000 update of recommendations for the use of hematopoietic colony-stimulating factors: evidence-based, clinical practice guidelines. J Clin Oncol. 2000. 18:3558–3585.
12. Borg C, Ray-Coquard I, Philip I, Clapisson G, Bendriss-Vermare N, Menetrier-Caux C, Sebban C, Biron P, Blay JY. CD4 lymphopenia as a risk factor for febrile neutropenia and early death after cytotoxic chemotherapy in adult patients with cancer. Cancer. 2004. 101:2675–2680.
13. Moreau M, Klastersky J, Schwarzbold A, Muanza F, Georgala A, Aoun M, Loizidou A, Barette M, Costantini S, Delmelle M, et al. A general chemotherapy myelotoxicity score to predict febrile neutropenia in hematological malignancies. Ann Oncol. 2009. 20:513–519.
14. Pettengell R, Bosly A, Szucs TD, Jackisch C, Leonard R, Paridaens R, Constenla M, Schwenkglenks M. Multivariate analysis of febrile neutropenia occurrence in patients with non-Hodgkin lymphoma: data from the INC-EU Prospective Observational European Neutropenia Study. Br J Haematol. 2009. 144:677–685.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download