Abstract
The vascular endothelial function is impaired in the very early stage of atherosclerosis in diabetic patients. The goal of this study was to identify the mechanism underlying the improvement in vascular endothelial function by sitagliptin in type 2 diabetes mellitus patients. This study was an open-labeled prospective observational single arm trial. Forty patients were treated with 50 mg of sitagliptin once daily for 12-weeks. The flow-mediated dilation (FMD) and plasma adiponectin were measured at baseline and 12 weeks after initiating treatment. The %FMD was significantly increased after treatment (4.13 ± 1.59 vs 5.12 ± 1.55, P < 0.001), whereas the nitroglycerin-mediated dilation (NMD) did not change. The plasma adiponectin levels significantly increased (13.0 ± 11.3 vs 14.3 ± 12.8, P < 0.001). The changes in the FMD were significantly correlated with those of the plasma adiponectin (r = 0.322, P < 0.05). A multivariate linear regression analysis demonstrated that the improvement in the FMD is associated with the plasma adiponectin (P < 0.05). The treatment of type 2 diabetes mellitus patients with sitagliptin reverses vascular endothelial dysfunction, as evidenced by increase in the FMD, and improvement of the adiponectin levels (UMIN Clinical Trials Registry System as trial ID UMIN000004236).
Diabetes mellitus (DM) is one of the most major risk factors for cardiovascular diseases, primarily as the result of adverse changes in arteries. A key change to arteries with DM that contributes to increased risk of cardiovascular diseases is the development of vascular endothelial dysfunction (1, 2), as indicated by reductions in endothelium-dependent dilation. Identifying the factors related to impaired endothelium-dependent dilation with DM is an important clinical goal because it may lead to effective strategies to prevent and/or treat DM-associated endothelial dysfunction. Ultrasound measurement of flow-mediated vasodilatation (FMD) is the most widely used non-invasive vascular test to evaluate endothelial function (3, 4).
Endothelial function is deteriorated by the attenuation of nitric oxide (NO) production (5, 6) and increased NO inactivation (7) in patients with DM. On the other hand, the impaired endothelial function improves after drug therapy or the correction of lifestyle habits. Therefore, the FMD is a useful parameter to evaluate the vascular function after treatment (8-11).
Inhibiton of dipeptidyl peptidase-4 (DPP-4) is a new mechanism for the treatment of DM that leads to increasing the action of incretins, which are gastrointestinal hormones. Glucagon-like peptide 1 (GLP-1), an incretin family member (12, 13), has been reported to promote insulin secretion in a glucose-dependent manner (14), and to inhibit glucagon secretion (15). GLP-1 improves the postprandial endothelial dysfunction (16) and left ventricular systolic function (17), and has vasodilator effects that are endothelium-dependent (18).
The clinical benefits of DPP-4 inhibitors on vascular function have not been evaluated. Therefore, the aim of this study was to measure the FMD before and after the administration of sitagliptin (a representative DPP-4 inhibitor) in patients with type 2 DM who were complicated with endothelial dysfunction, and to evaluate the impact on their endothelial function. In addition, this study compared the plasma adiponectin and asymmetric dimethylarginine (ADMA) levels, as biochemical markers that reflect the endothelial dysfunction, before and after drug administration.
This study enrolled 40 consecutive subjects > 20 yr of age with type 2 DM and with inadequate glucose control (defined as 6.5% ≤ Hemoglobin A1c [HbA1c] < 10%) even after dietary and exercise therapies for ≥ 8 weeks. The excluded subjects were if they had type 1 DM, were taking pioglitazone (which affects the endothelial function) (19), were insulin dependent, had known impairment of renal function (estimated glomerular filtration rate [eGFR] ≤ 60 mL/min/1.73 m2), had persistent elevations of their serum transaminases, or had DM that was uncontrollable (HbA1C > 10%) by oral medicine.
This study was an open-labeled prospective observational single arm trial. The patients were treated with 50 mg sitagliptin once daily for glycemic control, and were maintained on the same dose throughout the study period (12 weeks). All patients were instructed to continue diet and exercise therapy during the study. Clinical assessments, blood sampling, and evaluations of the endothelial function, carotid intima media thickness (IMT), and brachial ankle pulse wave velocity (ba-PWV) were performed in all patients both before and at 12 weeks after treatment.
The primary endpoint was improvement of the FMD at 12 weeks. Secondary endpoints were changes in the baseline fasting blood glucose, HbA1c, immunoreactive insulin (IRI), homeostasis model assessment (HOMA) index, β-cell function, mean IMT, mean ba-PWV, adiponectin, and ADMA. In addition, the correlation of the FMD with each of those measures was evaluated.
Blood samples were obtained from the antecubital vein after an overnight fast for at least 12 hr. The HbA1c levels were measured by latex agglutination, and the plasma glucose levels were determined by the glucose oxidase method. The serum IRI and lipids levels were measured by an immunoradiometic assay and enzymatic methods, respectively. The HOMA index value was calculated using the formula: (fasting blood glucose [mM] × fasting insulin [mU/L]/22.5). The β-Cell function was assessed using the formula: (20 × fasting insulin [mU/L]/[fasting glucose [mM]-3.5]) (20). The plasma adiponectin and ADMA levels were measured by latex agglutination and high-performance liquid chromatography (HPLC), respectively (SRL, Inc, Tokyo, Japan).
The patients' endothelial function was evaluated by means of the FMD, according to previously published guidelines (21). The subjects could not smoke, eat, or drink anything containing caffeine for 12 hr before the FMD measurement. The FMD was measured between 9 and 10 a.m. before patients had taken any medications.
The subjects were allowed to rest in the supine position at least 15 min before the examination, then the FMD was assessed in each right arm in a quiet, temperature-controlled (25℃) room by using a high-resolution ultrasound device (UNEXEF 18G, UNEX Corporation, Nagoya, Japan). A view of a 5 cm transverse section of the brachial artery was recorded for periods of 30 sec at baseline and during peak reactive hyperemia (after deflation of the blood pressure cuff previously inflated to 50 mmHg above the systolic blood pressure around the forearm for 5 min). The FMD was calculated as the percentage change in the diameter from the baseline value before cuff release to the peak value after cuff release. The endothelium-independent vasodilation was determined by measuring the arterial diameter in response to sublingual administration of 0.5 mg nitroglycerine after resting for at least 15 min. The nitroglycerin-mediated dilation (NMD) was calculated as the increase in the diameter 5 min after administrating nitroglycerine as a percentage of the baseline diameter.
The IMT was measured using the LOGIQ E9 instrument (General Electric Co., Ltd, Tokyo, Japan) with a 7 MHz linear array transducer. The patients were examined in the supine position with their neck extended and the probe was placed parallel to the common carotid artery (CCA). B-mode scans were obtained with electronic calipers. Three points each in the right and left CCA were measured and averaged.
The ba-PWV was measured using a volume-plethysmographic apparatus (from PWV/ABI; Colin Co., Komaki, Japan) with the patient in a supine position after 5 min of rest. This device simultaneously records the phonocardiogram, electrocardiogram, and volume pulse form and arterial blood pressure at both the left and right brachial and ankles. The ba-PWV was calculated by time-phase analysis between the right brachial and volume waveforms at both ankles. The distance between the right brachium and ankle was estimated based on the body height. The mean ba-PWV was used in the analyses because the right and left ba-PWV are significantly correlated (22).
The pulse rate and blood pressures (BP) were measured at rest, simultaneously with the measurement of the ba-PWV. The patients' height and weight were measured at the time of ba-PWV measurement, and the body mass index (BMI: kg/m2) was calculated as an index of obesity. The value for HbA1c (%) was estimated as an NGSP equivalent value (%) calculated by the formula HbA1c (%) = HbA1c (JDS) (%) + 0.4%, considering the relational expression of HbA1c (JDS) (%) measured by the previous Japanese standard substance and measurement methods and HbA1c (NGSP). Hypertension was defined as blood pressures ≥ 140/90 mmHg or the current use of antihypertensive agents. Dyslipidemia was defined as low-density lipoprotein-cholesterol (LDL-C) ≥ 3.62 mM or the current use of lipid-lowering agents. Chronic kidney disease was defined as patients with an eGFR ≤ 60 mL/min/1.73 m2. The eGFR was estimated using the simplified prediction equation derived from the modification of diet in renal disease study (23).
The SPSS ver. 16.0 software program was used for the statistical analysis. Differences between before and after administration were analyzed by employing one-way ANOVA, following unpaired t-test. Quality-assurance methods included previously described written protocols and measurement variability assessments (21). Reproducibility results compared the 3 sonographers' measurements of 20 studies separated by 1 yr. The coefficient of variation (CV) of inter-observer variability in FMD was 7.15%, which is the reasonable data to assess FMD value using edge-detection software compared with the analysis by hand (24). Also, CV of the intra-observer difference in FMD was 5.81%. And CV of inter-measurement variability in FMD was 2.95%. A Pearson's correlation analysis was carried out to determine the correlation of the changes of the FMD with variables such as age, male, smoking, those of fasting blood glucose, HbA1c, IMT, ba-PWV, adiponectin, and ADMA. A multivariate linear regression analysis was carried out using the changes of the FMD as the dependent variables and age, male, smoking, those of fasting blood glucose, HbA1c, IMT, ba-PWV, adiponectin, and ADMA as independent variables. A P value < 0.05 was considered to be significant.
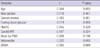
A total of 42 subjects were initially enrolled in this study. Two participants withdrew because of nausea and upper abdominal discomfort during the second week of sitagliptin treatment. The mean age of the remaining 40 participants was 68.9 ± 10.4 yr. The mean duration of diabetes was 4.4 ± 2.0 yr with an HbA1c of 7.3% ± 0.8%. The baseline clinical characteristics of the subjects are summarized in Table 1. Some subjects were on oral antidiabetic agents, including sulfonylureas (n = 13), α-glucosidase inhibitors (n = 10), biguanides (n = 13), and the other 17 were not taking any medicine. The changes in the various biochemical parameters after the 12 weeks treatment are shown in Table 2. The %FMD and FMD/NMD ratio were significantly (P < 0.001) increased, whereas the %NMD did not change (Fig. 1). The HbA1c, fasting blood glucose and ADMA levels were significantly (P < 0.001) decreased by the treatment. In addition, the plasma adiponectin levels were significantly (P < 0.001) increased. On the other hand, the fasting IRI, HOMA index of insulin resistance, carotid IMT and ba-PWV did not change.
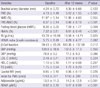
Table 3 shows the univariate correlations between the changes of the FMD and those of various parameters after the 12-week treatment with sitagliptin. The changes in the FMD were significantly (P < 0.05) correlated with those of the plasma adiponectin level (r=0.329; Fig. 2). The changes in the FMD showed no significant correlations with those of fasting blood glucose, HbA1c, ADMA, mean IMT or mean ba-PWV.
A multivariate linear regression analysis was done using the changes of the FMD as dependent variables; the results are listed in Table 4. The changes of the FMD showed a positive association with those of the plasma adiponectin (P = 0.043).
The current findings were that %FMD was increased, NMD did not change, HbA1c and ADMA levels were decreased (P < 0.001), plasma adiponectin levels were increased (P < 0.001) after 12 weeks of treatment. A multivariate linear regression analysis showed that the changes of the FMD had a positive association with those of the changes of the plasma adiponectin. The present study revealed that the sitagliptin reversed endothelial dysfunction (FMD/NMD ratio that indicated the true endothelium function) in type 2 DM patients. This implied that the treatment of type 2 DM patients selectively improved the endothelial function without affecting the vascular smooth muscle function because other vascular factor such as mean IMT, and mean ba-PWV were not changed.
Many reports regarding the relationship between DPP-4 and endothelial function have suggested the potential physiological mechanisms underlying this activity. First, DPP-4 inhibition by sitagliptin may be expected to increase the circulating levels of GLP-1. GLP-1 based therapy improves the postprandial endothelial dysfunction (16, 25, 26). Furthermore, animal studies demonstrate that GLP receptors are located in myocardial, vascular endothelial, and smooth muscle cells, and GLP-1 induces improvements in the cardiac function, as well providing cardioprotective effects, through the elevation of cAMP levels (17, 18). These protective effects are also likely mediated via cAMP-dependent protein kinase A (PKA) activation by sitagliptin (27). Therefore, sitagliptin may increase the cAMP levels, thus leading to a significant regression of arteriosclerotic lesions.
Second, there was a positive correlation between the changes of the FMD and those of the plasma adiponectin level. Adiponectin directly stimulates NO production by endothelial nitric oxide synthase (eNOS). Therefore, the increased adiponectin level likely exerts anti-atherosclerotic effects and improves the insulin resistance (19). The plasma adiponectin level was increased after sitagliptin treatment, thus suggesting that it may have been at least partially responsible for the improved endothelial function as a result of enhanced NO production.
Furthermore, the plasma ADMA level was decreased after sitagliptin treatment in the current study. Elevated levels of ADMA inhibit NO synthesis, and therefore impair the endothelial function and promote atherosclerosis (28). A high plasma concentration of ADMA is associated with the IMT, left ventricular hypertrophy and with increased cardiovascular events, particularly in patients with diabetes. The blood ADMA levels correlate inversely with the vascular endothelial function as evaluated by the FMD (29), and vasodilator responses improve the ADMA levels (30). The current results did not show a negative correlation between the changes of FMD and those of plasma ADMA probably due to small number of subjects or to the short follow-up period. ADMA levels were significantly decreased following treatment, suggesting that it may have a potential effect on the endothelial function in production of NO, will lead to vasodilatation in long term follow-up.
No significant changes in the serum lipid profile were observed after sitagliptin treatment in this study, although an increase in HDL-C and a decrease triglycerides has been reported previously (31). In addition, sitagliptin treatment is associated with a decrease in the BP (32). The BP showed a non-significant reduction in the current study (P = 0.13). These data probably reflects the small number of subjects.
Several studies have shown that the FMD is impaired in diabetic patients (33). Improvement in the FMD by hypoglycemic agents (pioglitazone [19, 34], gliclazide [35], and glimepiride [11]) has been reported, but the impact of DPP-4 inhibitors has rarely been evaluated. Endothelial dysfunction is a marker of the very early stage of atherosclerosis, and a close relationship exists between the endothelial function in the human coronary circulation and peripheral circulation (36). The improvement of the %FMD observed after the 12 weeks of treatment with sitagliptin in the present study might lead to a decrease in cardiovascular events. In fact, the previously published meta-analyses summarizing the effects of DPP-4 inhibitors on major cardiovascular events in phase 2 and 3 studies all suggest that they lead to a lower relative risk compared with placebo or other medications (37, 38).
The limitations of the present study include that it was conducted at a single academic center. This study was done in a single arm. In addition, patients received other medications that may have affected the FMD (e.g. statins, angiotensin converting enzyme inhibitors), but their use was similar between the group at baseline, and patients were requested not to change their medications during the study. In addition, the trial was conducted for only 12 weeks. Furthermore, DPP-4 inhibitor improved endothelial function in relation to the glucose profile, such as fasting blood glucose and HbA1c. Finally, the study did not have a sufficient statistical power to detect any small changes in the HOMA index of insulin resistance due to the relatively small number of patients enrolled, and there were no patients who experienced the primary end-points.
The DPP-4 inhibitor sitagliptin improved vascular endothelial function in Type 2 DM patients. In addition, the changes of the FMD positively correlated with those of the plasma adiponectin. These observations need to be confirmed in large cardiovascular outcome studies with long-term follow up of patients.
Figures and Tables
Fig. 1
Changes of the %FMD, %NMD and FMD/NMD ratio before and after treatment with sitagliptin therapy. (A) Flow mediated dilation (FMD) is significantly improved after 12 weeks. (B) Nitroglycerin-mediated dilation (NMD) is not improved. (C) An improved FMD/NMD ratio implies recovery of specific endothelial dysfunction. Columns are means ± SD. *P < 0.001 vs baseline.
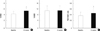
Fig. 2
Univariate correlations between the changes of %FMD (ΔFMD) and those of Δadiponectin, ΔADMA, and ΔHbA1c between baseline and after 12 weeks with sitagliptin therapy in type 2 diabetes.

Table 2
Changes of various parameters in the study patients before and after treatment with sitagliptin
FMD, flow-mediated vasodilatation; NMD, nitroglycerin-mediated dilation; HbA1c, hemoglobin A1c; IRI, immunoreactive insulin; HOMA, homeostasis model assessment; SBP, systolic blood pressures; DBP, diastolic blood pressures; LDL-C, low-density lipoprotein cholesterol; HDL-C, high-density lipoprotein cholesterol; TG, triglyceride; IMT, intima media thickness; ba-PWV, brachial ankle pulse wave velosity; ADMA, asymmetric dimethylarginine; Values are means ± SD.
References
1. Bonetti PO, Lerman LO, Lerman A. Endothelial dysfunction: a marker of atherosclerotic risk. Arterioscler Thromb Vasc Biol. 2003. 23:168–175.
2. Verma S, Anderson TJ. Fundamentals of endothelial function for the clinical cardiologist. Circulation. 2002. 105:546–549.
3. Rossi R, Nuzzo A, Origliani G, Modena MG. Prognostic role of flow-mediated dilation and cardiac risk factors in post-menopausal women. J Am Coll Cardiol. 2008. 51:997–1002.
4. Witte DR, Westerink J, de Koning EJ, van der Graaf Y, Grobbee DE, Bots ML. Is the association between flow-mediated dilation and cardiovascular risk limited to low-risk populations? J Am Coll Cardiol. 2005. 45:1987–1993.
5. Pepine CJ. The impact of nitric oxide in cardiovascular medicine: untapped potential utility. Am J Med. 2009. 122:S10–S15.
6. Goligorsky MS. Endothelial cell dysfunction: can't live with it, how to live without it. Am J Physiol Renal Physiol. 2005. 288:F871–F880.
7. Forstermann U, Munzel T. Endothelial nitric oxide synthase in vascular disease: from marvel to menace. Circulation. 2006. 113:1708–1714.
8. Higashi Y, Sasaki S, Nakagawa K, Ueda T, Yoshimizu A, Kurisu S, Matsuura H, Kajiyama G, Oshima T. A comparison of angiotensin-converting enzyme inhibitors, calcium antagonists, beta-blockers and diuretic agents on reactive hyperemia in patients with essential hypertension: a multicenter study. J Am Coll Cardiol. 2000. 35:284–291.
9. Modena MG, Bonetti L, Coppi F, Bursi F, Rossi R. Prognostic role of reversible endothelial dysfunction in hypertensive postmenopausal women. J Am Coll Cardiol. 2002. 40:505–510.
10. Frick M, Alber HF, Hugel H, Schwarzacher SP, Pachinger O, Weidinger F. Short- and long-term changes of flow-mediated vasodilation in patients under statin therapy. Clin Cardiol. 2002. 25:291–294.
11. Papathanassiou K, Naka KK, Kazakos N, Kanioglou C, Makriyiannis D, Pappas K, Katsouras CS, Liveris K, Kolettis T, Tsatsoulis A, et al. Pioglitazone vs glimepiride: differential effects on vascular endothelial function in patients with type 2 diabetes. Atherosclerosis. 2009. 205:221–226.
12. Holst JJ. The physiology of glucagon-like peptide 1. Physiol Rev. 2007. 87:1409–1439.
13. Miyawaki K, Yamada Y, Yano H, Niwa H, Ban N, Ihara Y, Kubota A, Fujimoto S, Kajikawa M, Kuroe A, et al. Glucose intolerance caused by a defect in the entero-insular axis: a study in gastric inhibitory polypeptide receptor knockout mice. Proc Natl Acad Sci USA. 1999. 96:14843–14847.
14. Vilsboll T, Krarup T, Madsbad S, Holst JJ. Both GLP-1 and GIP are insulinotropic at basal and postprandial glucose levels and contribute nearly equally to the incretin effect of a meal in healthy subjects. Regul Pept. 2003. 114:115–121.
15. Nauck MA, Heimesaat MM, Orskov C, Holst JJ, Ebert R, Creutzfeldt W. Preserved incretin activity of glucagon-like peptide 1 [7-36 amide] but not of synthetic human gastric inhibitory polypeptide in patients with type-2 diabetes mellitus. J Clin Invest. 1993. 91:301–307.
16. Koska J, Schwartz EA, Mullin MP, Schwenke DC, Reaven PD. Improvement of postprandial endothelial function after a single dose of exenatide in individuals with impaired glucose tolerance and recent-onset type 2 diabetes. Diabetes Care. 2010. 33:1028–1030.
17. Zhao T, Parikh P, Bhashyam S, Bolukoglu H, Poornima I, Shen YT, Shannon RP. Direct effects of glucagon-like peptide-1 on myocardial contractility and glucose uptake in normal and postischemic isolated rat hearts. J Pharmacol Exp Ther. 2006. 317:1106–1113.
18. Nystrom T, Gutniak MK, Zhang Q, Zhang F, Holst JJ, Ahren B, Sjoholm A. Effects of glucagon-like peptide-1 on endothelial function in type 2 diabetes patients with stable coronary artery disease. Am J Physiol Endocrinol Metab. 2004. 287:E1209–E1215.
19. Tsuchiya K, Akaza I, Yoshimoto T, Hirata Y. Pioglitazone improves endothelial function with increased adiponectin and high-density lipoprotein cholesterol levels in type 2 diabetes. Endocr J. 2009. 56:691–698.
20. Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC. Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia. 1985. 28:412–419.
21. Corretti MC, Anderson TJ, Benjamin EJ, Celermajer D, Charbonneau F, Creager MA, Deanfield J, Drexler H, Gerhard-Herman M, Herrington D, et al. Guidelines for the ultrasound assessment of endothelial-dependent flow-mediated vasodilation of the brachial artery: a report of the International Brachial Artery Reactivity Task Force. J Am Coll Cardiol. 2002. 39:257–265.
22. Lee JW, Lee HR, Shim JY, Im JA, Kim SH, Choi H, Lee DC. Viscerally obese women with normal body weight have greater brachial-ankle pulse wave velocity than nonviscerally obese women with excessive body weight. Clin Endocrinol (Oxf). 2007. 66:572–578.
23. Levey AS, Bosch JP, Lewis JB, Greene T, Rogers N, Roth D. Modification of Diet in Renal Disease Study Group. A more accurate method to estimate glomerular filtration rate from serum creatinine: a new prediction equation. Ann Intern Med. 1999. 130:461–470.
24. Woodman RJ, Playford DA, Watts GF, Cheetham C, Reed C, Taylor RR, Puddey IB, Beilin LJ, Burke V, Mori TA, et al. Improved analysis of brachial artery ultrasound using a novel edge-detection software system. J Appl Physiol. 2001. 91:929–937.
25. Nikolaidis LA, Mankad S, Sokos GG, Miske G, Shah A, Elahi D, Shannon RP. Effects of glucagon-like peptide-1 in patients with acute myocardial infarction and left ventricular dysfunction after successful reperfusion. Circulation. 2004. 109:962–965.
26. Nikolaidis LA, Elahi D, Hentosz T, Doverspike A, Huerbin R, Zourelias L, Stolarski C, Shen YT, Shannon RP. Recombinant glucagon-like peptide-1 increases myocardial glucose uptake and improves left ventricular performance in conscious dogs with pacing-induced dilated cardiomyopathy. Circulation. 2004. 110:955–961.
27. Ye Y, Keyes KT, Zhang C, Perez-Polo JR, Lin Y, Birnbaum Y. The myocardial infarct size-limiting effect of sitagliptin is PKA-dependent, whereas the protective effect of pioglitazone is partially dependent on PKA. Am J Physiol Heart Circ Physiol. 2010. 298:H1454–H1465.
28. Ueda S, Yamagishi S, Matsumoto Y, Fukami K, Okuda S. Asymmetric dimethylarginine (ADMA) is a novel emerging risk factor for cardiovascular disease and the development of renal injury in chronic kidney disease. Clin Exp Nephrol. 2007. 11:115–121.
29. Boger RH, Bode-Boger SM, Szuba A, Tsao PS, Chan JR, Tangphao O, Blaschke TF, Cooke JP. Asymmetric dimethylarginine (ADMA): a novel risk factor for endothelial dysfunction: its role in hypercholesterolemia. Circulation. 1998. 98:1842–1847.
30. Yilmaz MI, Sonmez A, Saglam M, Yaman H, Cayci T, Kilic S, Eyileten T, Caglar K, Oguz Y, Vural A, et al. Reduced proteinuria using ramipril in diabetic CKD stage 1 decreases circulating cell death receptor activators concurrently with ADMA. A novel pathophysiological pathway? Nephrol Dial Transplant. 2010. 25:3250–3256.
31. Tremblay AJ, Lamarche B, Deacon CF, Weisnagel SJ, Couture P. Effect of sitagliptin therapy on postprandial lipoprotein levels in patients with type 2 diabetes. Diabetes Obes Metab. 2011. 13:366–373.
32. Mistry GC, Maes AL, Lasseter KC, Davies MJ, Gottesdiener KM, Wagner JA, Herman GA. Effect of sitagliptin, a dipeptidyl peptidase-4 inhibitor, on blood pressure in nondiabetic patients with mild to moderate hypertension. J Clin Pharmacol. 2008. 48:592–598.
33. Rossi R, Cioni E, Nuzzo A, Origliani G, Modena MG. Endothelial-dependent vasodilation and incidence of type 2 diabetes in a population of healthy postmenopausal women. Diabetes Care. 2005. 28:702–707.
34. Rizza S, Cardellini M, Porzio O, Pecchioli C, Savo A, Cardolini I, Senese N, Lauro D, Sbraccia P, Lauro R, et al. Pioglitazone improves endothelial and adipose tissue dysfunction in pre-diabetic CAD subjects. Atherosclerosis. 2010. 215:180–183.
35. Chen LL, Yu F, Zeng TS, Liao YF, Li YM, Ding HC. Effects of gliclazide on endothelial function in patients with newly diagnosed type 2 diabetes. Eur J Pharmacol. 2011. 659:296–301.
36. Anderson TJ, Uehata A, Gerhard MD, Meredith IT, Knab S, Delagrange D, Lieberman EH, Ganz P, Creager MA, Yeung AC, et al. Close relation of endothelial function in the human coronary and peripheral circulations. J Am Coll Cardiol. 1995. 26:1235–1241.
37. Schweizer A, Dejager S, Foley JE, Couturier A, Ligueros-Saylan M, Kothny W. Assessing the cardio-cerebrovascular safety of vildagliptin: meta-analysis of adjudicated events from a large Phase III type 2 diabetes population. Diabetes Obes Metab. 2010. 12:485–494.
38. Frederich R, Alexander JH, Fiedorek FT, Donovan M, Berglind N, Harris S, Chen R, Wolf R, Mahaffey KW. A systematic assessment of cardiovascular outcomes in the saxagliptin drug development program for type 2 diabetes. Postgrad Med. 2010. 122:16–27.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download