Abstract
This study was conducted to clarify the prevalence of common skin diseases and their associated factors among military personnel in Korea. Four dermatologists visited adjacent military units and examined soldiers. A structured questionnaire that included questions about known skin diseases, demographic information, and questions for the Perceived Stress Index was completed for each participant. The soldiers that had been diagnosed with a skin disease answered one additional questionnaire (Skindex-29) which assess the influence of an individual's skin disease on daily life. Of 1,321 soldiers examined, 798 (60.4%) had one or more skin diseases. The three most common skin problems were acne (35.6%), tinea pedis (15.2%) and atopic dermatitis (5.1%). The diseases closely related to the period of military service were acne, tinea pedis, viral warts and corns. The diseases related to the amount of stress were atopic dermatitis, seborrheic dermatitis, and acne. The most troublesome skin diseases were atopic dermatitis, tinea cruris, and seborrheic dermatitis. These results demonstrated that the prevalence of skin disease among military personnel in Korea is very high, and that some of the skin disorders may have a significant influence on their daily lives.
Dermatologic disease is a major source of morbidity for military personnel, either at war or during peace times (1). Several epidemiologic studies regarding the prevalence of common skin diseases in military personnel exist. The proportion of soldiers with dermatologic problems amongst all outpatients was 20% and 12.2% in the southern Pacific during World War II and Vietnam War, respectively (1). In the recent East Timor deployment, it was reported that 25% of medical consultations were for dermatological problems (2). In a military clinic in Oslo, Norway, it was reported that skin disease was the third most common reason for seeking medical attention following upper respiratory disease and the musculoskeletal system during peace time (3).
In general, the spectrum of skin disease in the army is similar to that which exists in general civilian practice; dermatophyte infections, superficial bacterial skin infections, and eczematous dermatitis were among the most common skin complaints (3, 4). However, most of the previous studies only analyzed the number of physician visits. To date, there have been no studies regarding the exact prevalence of common skin diseases and their associated factors among military personnel in the English medical literature. In Korea, military service is compulsory for all healthy young men and provides specific environmental factors, such as a ranked society and communal living in specific places for a few years. These factors might be distinguishing characteristics of army life.
In the current study, our aim was to ascertain the prevalence of common skin diseases and their associated factors among military personnel in Korea and to determine the dermatologic disease-related quality of life (QoL).
The current cross-sectional, point-prevalence study was conducted from April to September 2010. The study used a purposive sampling method to survey soldiers at the corps located in the northern Gyeonggi province, Korea. A total of 1,516 soldiers were enrolled, which is 3.0% of the approximately 50,000 soldiers serving in one corps. We classified every soldier as one of the following five ranks: recruit (rank 0); private (rank 1); private first class (rank 2); corporal (rank 3); and sergeant (rank 4).
The presence of at least three-to-five comedones was required to diagnose acne. To establish a diagnosis of atopic dermatitis, all three of the following criteria had to be met: 1) pruritus; 2) chronic or relapsing history > 6 months; 3) typical morphology and distribution, including acute eczematous changes or chronic lichenification, prurigo, and hyperpigmentation. Keloids were defined as an overgrowth of dense fibrous tissue extending beyond the borders of the injury lasting > 6 months. The diagnosis of bacterial folliculitis encompassed the whole area of the body, such as the scalp, chin, trunk, and extremities. The diagnosis of other dermatitis, warts and corns, pityrosporum versicolor, tinea corporis, tinea pedis, psoriasis, and vitiligo was made first by clinical observation without laboratory examination. KOH examinations or Wood's lamp tests were performed as needed.
On the examination day, all of the soldiers available for physical check-ups were gathered and were fully informed of their enrollment in the study. A dermatology specialist in each military unit conducted the surveys and collected the study questionnaires. All of the participants who gave written consent were monitored by questionnaires. One of the questionnaires included questions pertaining to age, subject identity, and past history of skin diseases. Smoking, rank, and Perceived Stress Scale (PSS), which would be expected to be associated with dermatologic diseases, were also included in the questionnaire. The perceived stress was measured by the PSS, a 14-item self-questionnaire that measures the perception of life stress, including how often subjects perceived their life to be uncontrollable, unpredictable, and overwhelming (5).
After completing the given questionnaire, all of the subjects undressed, with the exception of underwear, and were individually examined in a nursing room. The assessment over the entire body, including the scalp, face, neck, trunk, and extremities was conducted and confirmed by one board-certified dermatologist.
The soldiers who were diagnosed with a skin disease by the dermatologist answered one additional questionnaire (Skindex-29). The Skindex-29 is an extensively studied health-related QoL for dermatologic diseases, and consists of 29 questions covering the burden of symptoms, functioning, and emotional domains, with a five-point Likert scale ("never" to "all the time", with higher scores indicating more severe effects on QoL) (6). The domain scores and an overall score were expressed on a 100-point scale.
The collected data were encoded, registered, and verified in the relevant databases. Soldiers who required further management were referred to the nearby Armed Forces Hospital.
All statistical analyses were performed using SPSS 19.0 (SPSS Inc., Chicago, IL, USA). The prevalence of all skin diseases was reported in percentage proportions, and the 95% confidence interval (95% CI) of the prevalence of each skin disease was estimated from the standard error.
Univariate analysis of current dermatologic conditions was first performed using univariate logistic regression. Then multivariate analysis was performed using logistic regression with adjustment for rank, smoking, and PSS, which are factors presumed to be associated with skin diseases. A P value < 0.05 was considered statistically significant. Odds ratios (ORs) were calculated using 95% CI. The three domains of the Skindex-29 score of each skin disease were reported as the mean and 95% CI.
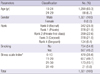
Informed consent was obtained from 91.9% (1,393 of 1,516) of the enrolled soldiers. A total of 1,321 soldiers were examined, for an overall response rate of 94.8% (1,321 of 1,393). Of the remaining 72 soldiers, 23 declined examination and 49 were not available at the time of the examination. According to the commanding officers, the lack of availability or dissent was due to the exclusion of dermatologic conditions. The demographic characteristics of the soldiers who entered the study are summarized in Table 1.
The majority of the soldiers (93.3%) were 19-24 yr of age and all of the soldiers were male.
The overall point prevalence of one or more visible skin conditions was 60.4% (798 of 1,321; 95% CI, 57.6%-63.0%). The prevalence breakdown according to specific skin conditions is shown in Table 2. The most common skin condition was acne, and the point prevalence was 35.7% (95% CI, 33.0%-38.2%). Tinea pedis (15.2%; 95% CI, 13.2%-17.0%) and atopic dermatitis (5.1%; 95% CI, 4.0%-6.3%) were the second and third most common skin diseases, respectively. Viral warts (4.7%), bacterial folliculitis (3.4%), corns (3.0%), tinea cruris (2.7%), and seborrheic dermatitis (2.1%) were relatively common dermatologic conditions.
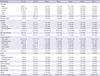
We demonstrated that rank, smoking, and stress scales were factors associated with the eight most common skin diseases using multivariate logistic regression with adjustment for relevant factors (Table 3). We considered five ranks of soldiers for the period of active service, with the intent to adjust the stress of ranks using the PSS index.
The diseases closely related to the period of military service were acne (P = 0.022), tinea pedis (P < 0.000), tinea cruris (P = 0.010), viral warts (P = 0.006) and corns (P = 0.085). None of the diseases was significantly related to smoking. The diseases related to the amount of stress were atopic dermatitis (P = 0.003), seborrheic dermatitis (P = 0.003), and acne (P = 0.047).
The Skindex-29 is a widely accepted dermatology-specific instrument, which is used to compare QoL of skin diseases (5). The overall response rate to the Skindex-29 was 83.0% (662 of 798) in this study. For reliability, we analyzed the Skindex-29 only if the number of subjects who completed the questionnaire was five or more.
Skindex-29 consists of symptoms, functioning, and emotional domains. Although a composite score had not been formerly verified for the validity and meaning of scores, the most overall troublesome skin diseases were atopic dermatitis (29.1; 95% CI, 23.0-35.2), tinea cruris (28.1; 95% CI, 20.7-35.6), and seborrheic dermatitis (26.8; 95% CI, 17.7-36.1). In the symptom domain of the Skindex-29, the skin diseases with the highest scores were atopic dermatitis (38.9; 95% CI, 32.1-46.1), acute urticaria (37.5; 95% CI, 18.7-52.6), and tinea cruris (35.7; 95% CI, 28.2-43.6) (Table 4). In relation to function, atopic dermatitis (20.6; 95% CI, 15.0-26.0), seborrheic dermatitis (19.6; 95% CI, 11.7-27.5) and tinea cruris (19.4; 95%, CI, 12.9-25.6) had the highest scores. In the emotional domain, skin diseases with the highest scores were tinea cruris (29.3; 95% CI, 21.0-37.5), atopic dermatitis (27.8; 95% CI, 21.8-33.5), and seborrheic dermatitis (27.8; 95% CI, 19.0-36.8).
In the current study, the point prevalence of at least one or more skin diseases in military personnel in Korea was 60.4% (95% CI, 57.6%-63.0%). To date, there have been no appropriate epidemiologic studies measuring the prevalence of skin diseases in army personnel. The first Health and Nutrition Examination Survey (HANES I), which was conducted from 1971-1974 in the USA, demonstrated that 312.4 per 1,000 persons (31.2%) in the general population had one or more significant skin conditions, which had been reviewed at least once by a physician (7). A study from Lambeth, UK, which was also conducted in the 1970s, revealed a self-reported frequency of 554.7 per 1,000 people (55.4%) with some type of skin condition (8). The results of the current study showed that skin diseases in military personnel in Korea are as common as in the general population, although the population in the study was limited by age and gender distributions for it to be compared directly with the general population.
Acne (35.7%) was the most common skin disease among the soldiers. Acne is often mistakenly thought to exclusively affect teenagers. However, a significant number of patients continue to experience acne or develop new-onset acne after the teenage years. A study involving the prevalence of acne in adults in Alabama, USA, showed that acne in the 20s was reported by 42.5% of men (9). Another report from Australia revealed that the prevalence of acne was 42.0% in the 20-29 yr old group (10). The current study also showed acne to be a very common skin problem in military personnel in Korea. Moreover, the patients with acne significantly increased as the period of service increased (30.1% in rank 0 to 41.6% in rank 4) and the stress index increased after adjustment (P = 0.047). It might be assumed that the stress from a class society, such as the military, can influence the development or aggravation of acne. The overall prevalence of bacterial folliculitis was 3.5% and was not related to rank, smoking, and the stress index.
Skin fungal infections are also very common in military personnel. Our results showed that the prevalence of tinea pedis, tinea cruris, tinea corporis and onychomycosis in the soldiers was 15.2%, 2.7%, 0.6%, and 0.9%, respectively. Interestingly, the prevalence of tinea pedis significantly increased as the rank increased (P < 0.001). It is likely that the common foot problems observed in the soldiers were mostly related to inappropriate footwear (occlusive leather shoes), foot trauma during increased sports activities, and poor hygiene. It is also possible that living in a group setting and common bathing facilities, which increased the risk of cross-infection, might have aggravated the conditions. In addition, tinea cruris was the second most common fungal infection soldiers acquired, and also increased significantly with rank (P = 0.010). Although the prevalence of tinea cruris was much lower than that of tinea pedis, many patients with tinea cruris complained of the emotional effect of these skin conditions.
In our survey, the prevalence of atopic dermatitis in military personnel in Korea was 5.1%. From a recent study conducted in Korea, the prevalence of atopic dermatitis in male adults was 4.2% (11). According to two recent studies involving Japanese adults, the prevalence of male adults in their 20s was 5.7% and 4.9% (12, 13). Although those who have severe atopic dermatitis are exempted from military duty, there are still many soldiers who suffer from atopic dermatitis. The prevalence of atopic dermatitis significantly correlated with the stress scale (P = 0.003). Moreover, atopic dermatitis was the most troublesome skin disease with respect to symptoms and function. The prevalence of seborrheic dermatitis was 2.1% in the current study, which was similar to the general population (1%-3%) (14). The occurrence of seborrheic dermatitis also correlated with the amount of stress reported (P = 0.003), and this disease significantly influenced the daily lives of soldiers functionally and emotionally. In addition, contact dermatitis (1.7%) and hand dermatitis (1.6%) were not rare in army personnel.
Viral warts and corns were also very common problems in military personnel, and the point prevalences were 4.7% and 3.0%, respectively. Interestingly, the prevalence of viral warts increased significantly with increasing rank (P = 0.006); the high prevalence might be due to sharing common living places and bathing facilities, factors also implicated in tinea pedis. The prevalence of corns increased marginally significantly with the period of service (P = 0.085), and we suggest that this condition is related with poor fitting footwear and frequent military marches.
There were many other skin conditions detected during the examinations, but most of the skin conditions did not occur in sufficient numbers to show a true prevalence. The prevalence of transient skin diseases, such as acute urticaria and insect bite allergies, might be underestimated because of the short duration of symptoms. In contrast, seasonal skin diseases, such as frostbite, would also be underestimated due to the times the examinations were conducted.
Korean military service is compulsory; therefore, studies of people in the military service may provide some information about the general population if the sample population is corrected with respect to age and gender distributions. However, patients who are exempted from military service due to severe skin diseases, such as atopic dermatitis and psoriasis, were not included in this study, and this could be a major limitation in applying the results of our study to the general population. Army life has some unique characteristics, such as a ranked society and communal living, and we earnestly desire to reveal the influence of these factors on skin diseases.
In conclusion, we suggest the prevalence of skin diseases among military personnel in Korea is very high and some of the skin diseases have a significant influence on daily life. Thus, the military authorities should be aware of common skin diseases and prepare countermeasures.
Figures and Tables
Table 3
Odds ratios and 95% confidence intervals for individual skin diseases based on the rank, smoking, and stress scale in 1,321 Korean soldiers

*Multivariable analysis was adjusted for rank, smoking, and stress scale; †Rank 0 was defined as recruit, rank 1 as private, rank 2 as private first class, rank 3 as corporal, and rank 4 as sergeant; ‡The perceived stress of the participants was measured by the Perceived Stress Scale, a 14-item self-questionnaire that measures perception of life stress, including how often subjects perceived their life to be uncontrollable, unpredictable, and overwhelming. OR, odds ratio; CI, confidence interval; ND, not determined.
References
1. Matz H, Orion E, Matz E, Wolf R. Skin diseases in war. Clin Dermatol. 2002. 20:435–438.
2. Lim D. Dermatology in the military: an East Timor study. Int J Dermatol. 2005. 44:304–311.
3. Selvaag E. Skin disease in military personnel. Mil Med. 2000. 165:193–194.
4. Vidmar DA, Harford RR, Beasley WJ, Revels J, Thornton SA, Kao TC. The epidemiology of dermatologic and venereologic disease in a deployed operational setting. Mil Med. 1996. 161:382–386.
5. Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983. 24:385–396.
6. Chren MM, Lasek RJ, Quinn LM, Mostow EN, Zyzanski SJ. Skindex, a quality-of-life measure for patients with skin disease: reliability, validity, and responsiveness. J Invest Dermatol. 1996. 107:707–713.
7. Johnson MT, Roberts J. Skin conditions and related need for medical care among persons 1-74 years. United States, 1971-1974. Vital Health Stat 11. 1978. (212):i–v. 1–72.
8. Rea J, Newhouse M, Halil T. Skin disease in Lambeth. A community study of prevalence and use of medical care. Br J Prev Soc Med. 1976. 30:107–114.
9. Collier CN, Harper JC, Cafardi JA, Cantrell WC, Wang W, Foster KW, Elewski BE. The prevalence of acne in adults 20 years and older. J Am Acad Dermatol. 2008. 58:56–59.
10. Plunkett A, Merlin K, Gill D, Zuo Y, Jolley D, Marks R. The frequency of common nonmalignant skin conditions in adults in central Victoria, Australia. Int J Dermatol. 1999. 38:901–908.
11. Kim MJ, Kang TW, Cho EA, Kim HS, Min JA, Park H, Kim JW, Cha SH, Lee YB, Cho SH, et al. Prevalence of atopic dermatitis among Korean adults visiting health service center of the Catholic Medical Center in Seoul Metropolitan Area, Korea. J Korean Med Sci. 2010. 25:1828–1830.
12. Saeki H, Tsunemi Y, Fujita H, Kagami S, Sasaki K, Ohmatsu H, Watanabe A, Tamaki K. Prevalence of atopic dermatitis determined by clinical examination in Japanese adults. J Dermatol. 2006. 33:817–819.
13. Saeki H, Oiso N, Honma M, Iizuka H, Kawada A, Tamaki K. Prevalence of atopic dermatitis in Japanese adults and community validation of the U.K. diagnostic criteria. J Dermatol Sci. 2009. 55:140–141.
14. Gupta AK, Bluhm R. Seborrheic dermatitis. J Eur Acad Dermatol Venereol. 2004. 18:13–26.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download