Abstract
It is well-known that the prevalence of attention deficit hyperactivity disorder (ADHD) is higher in epileptic children than in the general pediatric population. The aim of this study was to compare the accompaniment of ADHD in epileptic children with well-controlled seizures and no significant intellectual disability with that in healthy controls. We included epileptic children between the ages of 6 and 12 yr visiting our clinic for six consecutive months and controls without significant medical or psychiatric illnesses. We excluded patients with intellectual disability or persistent seizures during the recent three months. The diagnosis of ADHD was based on the criteria of the Diagnostic and Statistical Manual of Mental Disorders-IV (DSM-IV). After exclusion of 84 patients, we enrolled 102 (54.8%) children (mean age, 9.4 ± 2.0 yr). Seven (7 of 102, 6.9%) were diagnosed with ADHD. As compared to control group (4 of 110, 3.6%), there was no difference in ADHD accompaniment (P = 0.29). No difference was observed in ADHD accompaniment according to seizure type and epilepsy syndrome. In conclusion, the accompaniment of ADHD in epileptic children with well-controlled seizures and no intellectual disability may not differ from that of the general pediatric population.
It has been generally accepted that the prevalence of attention deficit hyperactivity disorder (ADHD) in the general pediatric population ranges between 3% and 5% (1). A recent review found that the worldwide prevalence rate of ADHD in this population is 5.29% (2). This rate increases when using the criteria of the Diagnostic and Statistical Manual of Mental Disorders-IV (DSM-IV): from 11.4% to 16.1% in the United States and from 2.4% to 19.8% outside of the United States (3). For children with epilepsy, it has been reported that the prevalence of ADHD is much higher than in the general pediatric population, ranging widely between 8% and 77% (4). According to the DSM-IV criteria for ADHD, the diagnosis of ADHD requires that the behaviors of inattention, hyperactivity, or impulsivity be inappropriate for the child's level of development. In addition, the symptoms need to be present before the age of 7 yr and these behaviors should not be attributable to another primary disorder. However, most studies examining the relationship between ADHD and epilepsy have failed to consider whether intellectual disability and uncontrolled seizures could affect the diagnosis of ADHD.
In this study, we compared the accompaniment of ADHD in epileptic children with well-controlled epilepsy and no significant intellectual disability with that in healthy controls. We also investigated whether the accompaniment of ADHD was influenced by the type of seizure or epilepsy syndrome.
We enrolled all epileptic children between the ages of 6 and 12 yr who visited the pediatric epilepsy clinic at Korea University Ansan Hospital between February 1 and July 31, 2011. We excluded patients with significant intellectual disabilities; patients who had a seizure during the recent three months; or patients who were taking any general medical or psychiatric conditions that could potentially compromise their mood or cognition.
Inclusion criteria were as follows: 1) all epileptic children who visited the pediatric epilepsy clinic at Korea University Ansan Hospital between February 1 and July 31, 2011; 2) between the ages of 6 and 12; 3) diagnosed with epilepsy after taking an electroencephalogram (EEG) and brain magnetic resonance imaging (MRI). Patients were further classified into types by a pediatric neurologist.
Exclusion criteria were as follows: 1) intellectual disability: classified as an intelligence quotient (IQ) under 70 using the Korean version of the Wechsler Intelligence Scale for Children-III (K-WISC-III), or by attendance at a special class; 2) any seizure attack during the recent three months; 3) significant general medical or psychiatric condition. Chronic or severe medical condition that could potentially affect the patient's attention or mood, as assessed through medical record review and parent interviews. For seizures, only clinical seizures were assessed, except for patients with absence epilepsy. For patients with absence epilepsy, both clinical and electrographic seizures were assessed.
Normal controls were randomly selected at out-patient clinic of our hospital who visited for acute respiratory illness or acute gastroenteritis. Children who have significant general medical or psychiatric illness that could potentially affect attention or mood were excluded. Age of the children also ranged from 6 to 12 yr.
ADHD diagnosis was based on DSM-IV criteria. To diagnose ADHD, we utilized parent questionnaires based on the DSM-IV criteria, parent interviews, and direct observation of children. If any discrepancies arose, the following tests were performed to confirm the diagnosis of ADHD: K-WISC-III, Projective psychological test, Neuropsychological test, and the Korean version of the Child Behavior Check List (K-CBCL).
Fisher's exact tests were used for comparing accompaniment of ADHD between patients and controls. Chi-square tests were used to determine whether ADHD accompaniment differed according to seizure type or epileptic syndrome. Mann-Whitney U tests and Fisher's exact tests were used to identify differences between patients with and without ADHD. All analyses were performed with SPSS (ver. 19.0; SPSS Inc., Chicago, IL, USA).
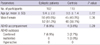
Between February 1 and July 31, 2011, there were 186 epileptic children between the ages of 6 and 12 yr who visited the pediatric epilepsy clinic at Korea University Ansan Hospital. Among these children, 56 (30.1%) were excluded for intellectual disability, and an additional 27 (14.5%) children with no intellectual disability were excluded for uncontrolled seizures. One child (0.5%) was excluded for depressive disorder. Thus, we enrolled 102 (54.8%) patients (age, mean ± SD, 9.4 ± 2.0 yr), of which 50 (49.0%) were boys and 52 were (51.0%) girls. One hundred and ten healthy controls (age, mean ± SD, 9.5 ± 1.4 yr) were included in our study with 45 (40.9%) boys and 65 (59.1%) girls. Table 1 presents the characteristics and comparisons of the enrolled patients and controls.
Among the 102 children enrolled, 7 (6.9%) were diagnosed with ADHD, including 4 boys and 3 girls. All had the combined type of ADHD. Two of these seven (28.6%) children were being medically treated for ADHD during the study. In control group, 4 of 110 (3.6%) children were diagnosed with ADHD (3 combined, 1 inattentive type). There were no differences in ADHD accompaniment, sex and ages between two groups, as shown in Table 1.
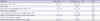
There was no difference in ADHD accompaniment between patients with localization-related and generalized epilepsy, or between different epilepsy syndromes: benign rolandic epilepsy (3 of 33, 9.1%); benign occipital epilepsy (0 of 7); cryptogenic focal epilepsy (2 of 29, 6.9%); symptomatic focal epilepsy (0 of 8); absence epilepsy (0 of 11); other idiopathic generalized epilepsy (2 of 14, 14.3%). There were no ADHD patients in the absence epilepsy group. These data are presented in Table 2.
Table 3 displays the differences between patients with and without ADHD in relation to age, sex, and seizure variables. There were no differences between patients with and without ADHD in seizure variables, such as age, gender, age of seizure onset, history of status epilepticus, number of anti-epileptic drugs, and duration of anti-epileptic drug treatment.
We examined the accompaniment of ADHD in epileptic children with well-controlled epilepsy and no significant intellectual disability. The results showed that 6.9% of epileptic children were accompanied by ADHD when they had normal intelligence and their seizures were well-controlled. In addition, there was no difference in ADHD accompaniment in comparison with healthy controls. Previously-reported ADHD prevalence rates in epileptic patients have been variable, but they have all been higher than ours, ranging from 8% to 77% (4). However, our results showed that children with well-controlled epilepsy and no intellectual disability may have similar rates of ADHD as the control group.
Most previous studies have not considered intellectual disability and seizures as possible confounding factors when assessing ADHD. Both factors can affect a child's attention or behavior, which might explain partly why ADHD prevalence rates have been so high and variable in previous studies. To avoid this problem, we excluded children with intellectual disability or frequent seizures before diagnosing ADHD. To our knowledge, this is the first prospective study to focus on ADHD in epileptic children without intellectual disability or frequent seizures. After controlling for these factors, the ADHD accompaniment was similar to that of the general pediatric population.
It is generally accepted that the combined type of ADHD is the most common type in the general pediatric population (5), while the inattentive type of ADHD may be more common in epileptic children (4). However, after controlling for intellectual disability and frequent seizures, we found that the combined type of ADHD was the most prevalent among children with epilepsy, which was also noted in the control group. It parallels the results reported for the general pediatric population.
In this study, there was no difference in ADHD accompaniments between seizure types. Moreover, no patients with absence epilepsy had well-controlled seizures. Many studies have examined the relationship between ADHD and absence epilepsy. One study found that comorbidities, including cognitive and linguistic problems and ADHD, were related to the duration of the illness and seizure frequency (6). Another study found that the active seizure group was more impatient and less proficient at homework (7). These studies suggest that the seizures themselves could influence the diagnosis of ADHD in absence epilepsy. After controlling seizures, no patients with absence epilepsy had ADHD in our study. In addition, there were no differences between patients with and without ADHD in terms of seizure variables, such as age, gender, age of seizure onset, history of status epilepticus, number of anti-epileptic drugs, and duration of anti-epileptic drug treatment.
Among children with epilepsy, there are some predisposing factors that may induce hyperactivity, inattention, and impulsivity (8). First, an underlying central nervous system (CNS) dysfunction could be a factor. It might be accompanied by genetic defects and manifest as intellectual disability, seizures, and symptoms of inattention, hyperactivity, or impulsivity. Thus, intellectual disability can aggravate the behaviors that characterize ADHD. Among children with intellectual disability, we cannot judge whether or not their behaviors are consistent with their developmental level, yet this information is required in order to assess ADHD using the DSM-IV criteria. Though some reports suggest that treating intellectual disability with CNS stimulants can benefit children with epilepsy by improving the hyperactive and inattentive behaviors usually shown in these patients (9-11), the pharmacologic response is variable, which contrasts with the results for normal children (12). Thus, the symptoms of ADHD that can be observed in children with intellectual disability should be studied separately from those of normal children because they are a different disease entity. Seizure is another factor among children with epilepsy that can induce hyperactivity, inattention, and impulsivity. There are many seizure-related variables including seizure controllability (13). Most importantly, multiple seizures can alter a patient's perception. Considerable evidence suggests that seizure control improves the symptoms of ADHD. For example, seizures or subclinical epileptiform bursts are associated with educational problems, which are improved through seizure control (14). The risk of ADHD increases in children whose seizures are more resistant and whose EEGs show more epileptiform discharges (15). Otherwise, ADHD is more prevalent in new onset idiopathic epilepsy than in healthy controls: 26.4% vs 10%, respectively, in one recent study (16), and 31% vs 6%, respectively, in another (17). However, the results could have been affected by frequent seizures, which are commonly observed in children with new onset epilepsy. After epilepsy surgery, early improvements in attention result directly from the removal of the epileptic focus (18). A ketogenic diet decreased hyperactivity in rats (19). Alertness and memory were improved after control of seizure with vagus nerve stimulation (20). Thus, the combined evidence suggests that clinicians should attempt to consider a patient's epileptic condition when diagnosing ADHD.
Our study has advantages and limitations. The design of our study was prospective and patient recruitment was consecutive. That can be a cross section of the target population. However, the small size of sample can be a possible limitation. Another limitation of the present study is that the diagnosis of ADHD is based on the parent's report and physician's interview.
In conclusion, the accompaniment of ADHD in epileptic children with well-controlled seizures and no intellectual disability may not differ from that of the general pediatric population. When diagnosing children with ADHD in epileptic children, clinicians should first evaluate the children's intelligence before determining whether their behaviors are consistent with their developmental level, and they should also consider frequent seizures as a confounding factor to be controlled prior to ADHD diagnosis, especially in children having absence seizures. Future studies are needed to clarify our results in a larger population.
Figures and Tables
References
1. American Psychiatric Association. Diagnostic and statistical manual of mental disorders: DSM-IV. 1994. 4th ed. Washington DC: American Psychiatric Association.
2. Polanczyk G, de Lima MS, Horta BL, Biederman J, Rohde LA. The worldwide prevalence of ADHD: a systematic review and metaregression analysis. Am J Psychiatry. 2007. 164:942–948.
3. Faraone SV, Sergeant J, Gillberg C, Biederman J. The worldwide prevalence of ADHD: is it an American condition? World Psychiatry. 2003. 2:104–113.
4. Dunn DW, Austin JK, Harezlak J, Ambrosius WT. ADHD and epilepsy in childhood. Dev Med Child Neurol. 2003. 45:50–54.
5. Szatmari P, Offord DR, Boyle MH. Ontario Child Health Study: prevalence of attention deficit disorder with hyperactivity. J Child Psychol Psychiatry. 1989. 30:219–230.
6. Caplan R, Siddarth P, Stahl L, Lanphier E, Vona P, Gurbani S, Koh S, Sankar R, Shields WD. Childhood absence epilepsy: behavioral, cognitive, and linguistic comorbidities. Epilepsia. 2008. 49:1838–1846.
7. Vega C, Vestal M, DeSalvo M, Berman R, Chung M, Blumenfeld H, Spann MN. Differentiation of attention-related problems in childhood absence epilepsy. Epilepsy Behav. 2010. 19:82–85.
8. Hamoda HM, Guild DJ, Gumlak S, Travers BH, Gonzalez-Heydrich J. Association between attention-deficit/hyperactivity disorder and epilepsy in pediatric populations. Expert Rev Neurother. 2009. 9:1747–1754.
9. Aman MG. Stimulant drugs in the developmental disabilities revisited. J Dev Phys Disabil. 1996. 8:347–365.
10. Pearson DA, Santos CW, Roache JD, Casat CD, Loveland KA, Lachar D, Lane DM, Faria LP, Cleveland LA. Treatment effects of methylphenidate on behavioral adjustment in children with mental retardation and ADHD. J Am Acad Child Adolesc Psychiatry. 2003. 42:209–216.
11. Roberts JE, Miranda M, Boccia M, Janes H, Tonnsen BL, Hatton DD. Treatment effects of stimulant medication in young boys with fragile X syndrome. J Neurodev Disord. 2011. 3:175–184.
12. Aman MG, Buican B, Arnold LE. Methylphenidate treatment in children with borderline IQ and mental retardation: analysis of three aggregated studies. J Child Adolesc Psychopharmacol. 2003. 13:29–40.
13. Hermann BP, Whitman S, Hughes JR, Melyn MM, Dell J. Multietiological determinants of psychopathology and social competence in children with epilepsy. Epilepsy Res. 1988. 2:51–60.
14. Marston D, Besag F, Binnie CD, Fowler M. Effects of transitory cognitive impairment on psychosocial functioning of children with epilepsy: a therapeutic trial. Dev Med Child Neurol. 1993. 35:574–581.
15. Bennett-Back O, Keren A, Zelnik N. Attention-deficit hyperactivity disorder in children with benign epilepsy and their siblings. Pediatr Neurol. 2011. 44:187–192.
16. Jones JE, Watson R, Sheth R, Caplan R, Koehn M, Seidenberg M, Hermann B. Psychiatric comorbidity in children with new onset epilepsy. Dev Med Child Neurol. 2007. 49:493–497.
17. Hermann B, Jones J, Dabbs K, Allen CA, Sheth R, Fine J, McMillan A, Seidenberg M. The frequency, complications and aetiology of ADHD in new onset paediatric epilepsy. Brain. 2007. 130:3135–3148.
18. Lendt M, Helmstaedter C, Kuczaty S, Schramm J, Elger CE. Behavioural disorders in children with epilepsy: early improvement after surgery. J Neurol Neurosurg Psychiatry. 2000. 69:739–744.
19. Murphy P, Burnham WM. The ketogenic diet causes a reversible decrease in activity level in Long-Evans rats. Exp Neurol. 2006. 201:84–89.
20. You SJ, Kang HC, Kim HD, Ko TS, Kim DS, Hwang YS, Kim DS, Lee JK, Park SK. Vagus nerve stimulation in intractable childhood epilepsy: a Korean multicenter experience. J Korean Med Sci. 2007. 22:442–445.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download