Abstract
This study was conducted to examine the nation-wide emergency department (ED) utilization pattern by children in Korea. Most referral hospital EDs provide their essential ED information to the National Emergency Medical Center through the National Emergency Department Information System (NEDIS). We analyzed the NEDIS data on pediatric visits (< 19 yr old) during three years, from June 1, 2008 to May 31, 2010. A total of 2,072,664 children visited 124 EDs during the study period, and this patient population comprised 31.2% of the total ED visits. Male patients with a mean age of 5.44 (± 5.40 SD) yr comprised 59.1% of the ED pediatric visits. Among all age groups, the 1-4-yr-old group was the largest (42.3%). The most common mode of arrival was non-emergency medical service (EMS) (90.7%), and only 4.2% of patients used EMS transport. Common chief complaints in infants were fever (37.4%), whereas many older children presented to the EDs with abdominal pain (15.4%). The ratio of disease versus injury as the cause of ED visits was 2.5:1. Most patients were discharged (81.2%), and 15.3% were admitted. In conclusion, the most common age group who are brought to EDs in Korea is 1 to 4 yr-old young children, and common chief complaints of the visiting children are age-dependent, such as fever in younger children and abdominal pain and headache in older children. We need more improved and organized emergency medicine service system for children in Korea.
The emergency department (ED) is an important entry to hospital-based emergent care for acutely ill and injured children. Pediatric visits to EDs constitute a substantial part of the total ED utilization. In the United States (US), 20.5% of all ED visits in 2005 were for the care of children less than 18 yr of age (1). Although data on pediatric visits to EDs are being collected and accumulated, these data have not been widely studied and reported. Large sample sizes of pediatric visits to the ED have been epidemiologically studied in the US, Canada, Australia, and New Zealand (2-4), but other studies have shown similar results but with small patient populations from a hospital or an institute (5, 6). In other areas of the world, including Korea, these data are lacking, requiring future studies for understanding the pattern of ED utilization.
According to the 'Act on the Emergency Medical Care' in Korea, there are three categories of Korean EDs, ranging from large to small with regard to the size and function of the EDs: 1) regional emergency centers (REC), 2) local emergency centers (LEC), and 3) local emergency institutes (LEI). As of the end of 2010, all RECs (16 of 16) and the majority of LECs (108 of 122) provided their essential ED information to the National Emergency Medical Center (NEMC). The NEMC is a government-funded, national ED control agency, and one of its main roles is to acquire data from patients who visit EDs in order to maintain health care quality and improve the emergency medical service (EMS) system. These data are transferred electronically from the major hospitals to the NEMC via a transfer system called the National Emergency Department Information System (NEDIS). The NEDIS has operated since 2003 with a small number of EDs, and the number of participating hospitals has steadily increased. Since 2006, the NEDIS system has been regarded as a nation-wide reliable source of ED information available to many researchers.
Using the NEDIS data, this epidemiologic study was conducted to examine the pediatric visits to EDs in Korea. Results from this study will be useful for improving the EMS system of each area and in making decisions regarding the appropriate distribution of resources for emergency care of children in Korea.
We conducted a nation-wide, cross-sectional study on the epidemiology of pediatric ED utilization in Korea. We obtained official permission to use the anonymized NEDIS data set from the NEMC. Using the NEDIS data, we analyzed the pediatric visits (< 19 yr old) during three years, from June 1, 2006 to May 31, 2009. Because there was an unusual surge of pediatric ED visits from late autumn of 2009 to the spring of 2010, mainly due to the epidemic of pandemic Influenza A (H1N1) in Korea, we chose to enroll only the data before the surge.
We extracted and analyzed the demographics of the children, including 1) age and sex, 2) arrival and departure time (time, day, season, and year), 3) route of arrival (direct from scene/home, transfer from other outpatient department [OPD] or hospital), and 4) mode of arrival (transport by EMS ambulance, hospital ambulance, other ambulance, police, air transport, or public transport). We divided the subjects into five age groups by years: < 0 (infant), 1-4 (young children), 5-9 (pre and early school age), 10-14 (school age), and 15-18 (adolescence) yr old. We also obtained data on chief complaints, causes of the visits (disease or injury), and outcome of the ED management (discharge, transfer to other hospital, admission, or death).
Length of stay (LOS) was defined as the interval between the arrival time at the ED and the departure time from the ED (discharge, admission, or transfer) in minutes. LOS is widely known to be related to overcrowding of EDs and is consequently influential to the quality of emergency care. Comparing patients within the same variables, we analyzed the factor(s) associated with long or short LOS when the LOSs were clearly described in the NEDIS data set.
Because admitted children presumably had more serious conditions than discharged ones, we focused on admitted patients. We compared the number and rate of admission by each age group and month. The critically ill patient was defined as a child who was dead or admitted to intensive care units, and the number and rate of critically ill patients were measured in each age group. We also performed logistic regression analysis to identify possible demographic factor(s) associated with patient admission. Data regarding critically ill patients are important for providing adequate distribution of advanced resources, such as well-trained personnel and high-end equipment.
Data were presented as discrete and continuous variables using counts and percentages and as means and standard deviations (SDs), respectively. Some data regarding the route and mode of arrival, LOS, and admission were missing, and these missing data were excluded from analysis, as indicated in the text, tables, and figures. We used the chi square test to compare the proportion of disease and injury, according to age group, time, month, and season. We also used ANOVA and post hoc Bonferroni tests to find factors associated with LOS in the ED. We performed a multivariate logistic regression analysis to find factors associated with hospital admission. The Stata/MP12.0 for Windows (Stata Corp., LP, College Station, TX, USA) was used in all analyses, and P value lower than 0.05 was set as statistically significant.
During the study period, a total of 2,072,664 children visited 124 EDs (16 RECs and 108 LECs), comprising 31.2% of all ED visits (6,643,154, including all ages of the pediatric patients). The mean age of these patients was 5.44 ± 5.40 (SD) yr old, and 1,224,747 (59.1%) were males. Of the five age groups, the 1-4-yr-old group was the largest (42.3%), followed by the 5-9-yr-old group (19.4%) and the infant group (15.4%). Most children arrived at the EDs in the evening (from 18:00 to 23:59) or the weekend (Saturday and Sunday, 40.1%), with no apparent seasonal variation.
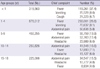
The main route of arrival was directly from the scene/home (90.8%), and the mode of arrival was mainly walk-in (44.8%), followed by private ground transport (31.0%). Only 4.2% of the children were transported to the EDs by government-operated EMS ambulance (Table 1).
In the infant group, the most common chief complaint was fever (37.4%), followed by vomiting (8.0%) and cough (6.7%). With increasing age of the children, the proportion of fever complaints decreased. Abdominal pain was the most common symptom in the 10-14- and 15-18-yr-old groups (16.6%, and 15.5%, respectively; Table 2).
Because the working diagnoses were vague in most cases of the NEDIS data set, the type of visit was divided into two categories: disease or injury. According to this classification, pediatric visits for disease and injury were 71.4% and 28.6%, respectively, resulting in a disease versus injury ratio of 2.5:1. More male than female children visited the EDs due to injury (383,994 vs 208,238). With increasing age of the children, the proportion of visits for injury significantly increased (P < 0.001). The peak time and day of visits for injury were in the afternoon and on Saturday (36.1% and 30.9%, respectively; Table 3).
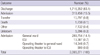
A total of 1,716,352 (83.1%) children were discharged from the EDs, and 319,456 (15.5%) children were admitted. Of the total patients 289,754 (14.1%) and 13,387 (0.7%) were admitted to the general ward and intensive care unit (ICU), respectively. Patients transferred to other hospital were 15,797 (0.8%), and the total number of deaths at the ED was 1,238 (0.1%; Table 4). During the study period, the total number of critically ill patients who died (n = 1,238) or were admitted to the ICU directly from the EDs (n = 13,387) or through the operating theater (n = 900) was 15,525 (0.8%).
The mean LOS for visits caused by disease was significantly longer than that for visits caused by injury (141.8 vs 93.6 min, P < 0.001). Other factors associated with increased LOS were; 1) 15-18-yr-old age group (P < 0.001, compared with all other age groups in a post hoc analysis), and 2) time of visit from 06:00 to 11:59 (P < 0.001, compared with all other time segments in a post hoc analysis). In contrast, factors associated with a short LOS were; 1) visiting time from 18:00 to 23:59 (P < 0.001, compared with all other time segments in a post hoc analysis), and 2) Sunday day of visit (P < 0.001, compared with all other days in a post hoc test).
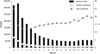
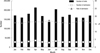
The analysis of admitted patients was performed among subjects for whom data regarding the outcome of the ED management of the admitted patient were available (n = 2,065,271). The number and rate of admitted children by age are summarized in Fig. 1. The infant group showed the highest admission rate (n = 79,705; 25.2%), and the rate decreased to reach the nadir at two years old (n = 27,742; 12.2%). In children 4 yr or older, the admission rate showed a slow and steady increase to the end of the adolescence. However, the monthly variation in the admission rate was not significant (Fig. 2).
We performed a multivariate logistic regression analysis to find the factors associated with admission, and the results are summarized in Table 5. Males were 1.1 times more likely to be admitted compared with females. The possibility of pediatric admission in patients who visited EDs from 0:00 to 05:59 was significantly lower compared to patients who visited during the other time segments. Visits due to injury showed a significantly lower likelihood of admission compared with visits due to disease (odds ratio [OR]=0.32; 95% confidence interval [CI], 0.32-0.33). Among the routes of ED arrival, OR of admission by transfer from other hospitals and outpatient department (OPD) were 6.53 (95% CI, 6.46-6.61) and 9.07 (95% CI, 8.86-9.28), respectively, when compared to direct visits. Visits by EMS ambulance showed 2.46 times higher OR for admission (95% CI, 2.42-2.50), compared with arrival via means other than EMS ambulance.
The analysis of critically ill patients was performed in subjects for whom the outcome of the ED management was known (n = 2,065,271). The total number of critically ill patients was 15,525; and the number and rate of critically ill children by age are summarized in Fig. 3. Similar to the admitted patients, the infant group showed the highest rate of being critically ill (6,949 [2.2%] out of 317,315). At two years of age, the rate was the lowest (491 [0.22%] out of 222,876). The rate slowly increased to peak at 17 yr of age.
In this study, we analyzed epidemiologic data on pediatric utilization of major EDs in Korea. Previous studies on pediatric ED utilization in single institutions in Korea have been conducted and reported (7-9). The current study is the first nation-wide observation on the demographics, arrival at EDs, chief complaints, and outcome of ED management of pediatric patients. Additionally, we elucidated several factors associated with the admission of critically ill children during the 3-yr study period. Similar studies have been reported on data from developed or developing countries; however, nation-wide, multi-year studies on this subject are rare.
This study provides insight into pediatric visits to large EDs in Korea. The results of the study clearly showed 1) more pediatric visits were due to disease than to injury, 2) the chief complaint type was substantially different between age groups, 3) the 1-4-yr-old age group was the most common age group to visit the ED, 4) the admission rate of all pediatric patients was 14.1%, and 5) an average of 14 critically ill children presented to an ED each day.
The data from this study will be useful in designing improved pediatric EMS services in Korea. For example, because the 1-4-yr-old age group with disease is the most common group to present to the ED, this specific group and causative conditions should be a main target of ED preparedness, distribution of ED resources, and education for ED personnel. Moreover, because an average of 14 critically ill patients presented daily to an ED, regionalization of EDs with specialized facilities or equipment should be considered, rather than providing all 124 major EDs in Korea with seldom-used specialized equipment. Further studies on critically ill patients should be conducted to design adequate preparation for true emergent pediatric cases.
In a cornerstone study published in 2005, Alpern et al. (2) reported the epidemiologic data from a 1-yr period on pediatric visits to 25 US EDs (n = 754,004) that participated in the Pediatric Emergency Care Applied Research Network (PECARN). The PECARN group researchers reported the demographic data of pediatric patients, the common diagnoses in EDs and hospital admissions, and the factors associated with admission. In another large-scale study conducted in Australia and New Zealand, the pediatric ED visits were collected from 11 sites (n = 351,440) that participated in the Pediatric Research in Emergency Department International Collaborative (PREDICT) study (4), and the authors reported on the demographics, common diagnoses at EDs, and seasonal variation of the patients. These two studies are important large-scale epidemiologic studies on pediatric ED visits. With over 2 million patients included in this report, the current study is the largest nation-wide analysis of pediatric visits to the ED.
A comparison of our results with those from the PECARN and PREDICT studies revealed some similar and some different results. For example, the admission rate of the children from PECARN and PREDICT studies were 11.6% and 24.0%, respectively, whereas the admission rate in our study was 14.1%. The discrepancies among these data may be due to the different types and number of EDs included in the studies, the different management preferences among caregivers of the three countries, or the different methods of data acquisition and transfer. We believe that the data set derived from EDs in each country or area may result in different results. Therefore, to improve the pediatric EMS services in each country and area, the data collection and analysis should be relevant to the area being serviced. Although a previous study (10) demonstrated that weather was an important factor in pediatric ED visits, this study showed no significant seasonal and monthly variations in the admission rate.
This study has several limitations. First, the data were collected from relatively large-sized EDs, and therefore the generalization of these data to smaller-sized EDs may not be appropriate. However, these data included most of the clinically significant patient issues and can be used to improve EMS services in large EDs in Korea. Second, in contrast to the studies by the PECARN and PREDICT groups, we could only report common chief complaints of the pediatric visits rather than exact clinical diagnoses of the subjects. This drawback is associated with incomplete data entered in the Korean NEDIS. Further studies including more detailed diagnoses at the EDs and at hospital admission are warranted. Third, the NEDIS data set does not provide the level of preparedness of each ED, including personnel and equipment, and therefore, we could not determine the appropriateness of the ED management of the patients. However, this point is beyond the scope and aim of this study, and further studies will be required to examine the preparedness of the EDs. Finally, because the 124 participating EDs used several different triage tools to determine the severity of the pediatric patients' complaints, we were unable to analyze and compare the subgroups categorized by severity.
Conclusively, the most common age group who are brought to EDs in Korea is 1 to 4 yr-old young children, and common chief complaints of the visiting children are age-dependent, such as fever in younger children and abdominal pain and headache in older children. Although the great majority (>85%) of the visiting children can be discharged, as many as 14 critically-ill children are brought to EDs everyday. We need more improved and organized emergency medicine service system for children in Korea.
Figures and Tables
Table 1
Demographic data of children (< 19 yr old) who visited the 124 EDs in Korea from June 1, 2006 to May 31, 2009

ACKNOWLEDGMENTS
All the authors thank those personnel of NEDIS (National Emergency Department Information System) participating institutions who contributed the collection and distribution of national data on pediatric emergency department utilization. We also thank Dr. Jin Hee Lee of Seoul National University Bundang Hospital, Dr. Jin Hee Jung of Inje University Seoul Paik Hospital and for their critical review and comments on our manuscript.
References
1. Nawar EW, Niska RW, Xu J. National Hospital Ambulatory Medical Care Survey: 2005 emergency department summary. Adv Data. 2007. (386):1–32.
2. Alpern ER, Stanley RM, Gorelick MH, Donaldson A, Knight S, Teach SJ, Singh T, Mahajan P, Goepp JG, Kuppermann N, et al. Epidemiology of pediatric emergency medicine research network: the PECARN Core Data Project. Pediatr Emerg Care. 2006. 22:689–699.
3. Li G, Lau JT, McCarthy ML, Schull MJ, Vermeulen M, Kelen GD. Emergency department utilization in the United States and Ontario, Canada. Acad Emerg Med. 2007. 14:582–584.
4. Acworth J, Babl F, Borland M, Ngo P, Krieser D, Schutz J, Pitt R, Cotterell E, Jamison S, Neutze J, et al. Patterns of presentation to the Australian and New Zealand Paediatric Emergency Research Network. Emerg Med Australas. 2009. 21:59–66.
5. Zimmer KP, Walker A, Minkovitz CS. Epidemiology of pediatric emergency department use at an urban medical center. Pediatr Emerg Care. 2005. 21:84–89.
6. Rehmani R, Norain A. Trends in emergency department utilization in a hospital in the Eastern region of Saudi Arabia. Saudi Med J. 2007. 28:236–240.
7. Tchah H, Yun DR. Utilization patterns of pediatric emergency room. J Korean Pediatr Soc. 1989. 32:897–914.
8. Yoo JW, Lee JH. Clinical analysis of pediatric patients who visited a general hospital emergency center. Korean J Pediatr. 2010. 53:314–322.
9. Jeon HJ, Kim SS, Bae HA, Yoo IY. Utilization status of emergency medical service for children. J Korean Acad Child Health Nurs. 2008. 14:5–13.
10. Christoffel KK. Effect of season and weather on pediatric emergency department use. Am J Emerg Med. 1985. 3:327–330.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download