Abstract
Whether arterial conduits are superior to venous grafts in coronary artery bypassing has been debated. The aim of this study was to investigate clinical outcomes after total arterial revascularization versus conventional coronary bypassing using both arterial and venous conduits in isolated three-vessel coronary disease. Between 2003 and 2005, 503 patients who underwent isolated coronary artery bypass grafting for three-vessel coronary disease were enrolled. A total of 117 patients underwent total arterial revascularization (Artery group) whereas 386 patients were treated with arterial and venous conduits (Vein group). Major adverse outcomes (death, myocardial infarction, stroke and repeat revascularization) were compared. Clinical follow-up was complete in all patients with a mean duration of 6.1 ± 0.9 yr. After adjustment for differences in baseline risk factors, risks of death (hazard ratio [HR] 0.96; 95% confidence interval [CI] 0.51-1.82, P = 0.90), myocardial infarction (HR 0.20, 95% CI 0.02-2.63, P = 0.22), stroke (HR 1.29, 95% CI 0.35-4.72, P = 0.70), repeat revascularization (HR 0.64, 95% CI 0.26-1.55, P = 0.32) and the composite outcomes (HR 0.83, 95% CI 0.50-1.36, P = 0.45) were similar between two groups. Since the use of veins does not increase the risks of adverse outcomes compared with total arterial revascularization, a selection of the conduit should be more liberal.
Although the internal thoracic artery (ITA) has been regarded as the graft of choice for left anterior descending artery (LAD) bypass during coronary artery bypass grafting (CABG) (1), there have been debates over which conduits are best fitted as second and third grafts for non-LAD bypass. Unlike several reports supporting the superior patency of arterial grafts over venous grafts (2-4), a recent prospective randomized study showed that the selection of arterial or venous graft for the second graft has not affected patency beyond 5 yr (5). In a clinical perspective that the purpose of CABG is to relieve ischemic symptoms and to improve survival, evidences are poor with regard to the selection of optimal second and third grafts for non-LAD bypass relating to clinical outcomes (6).
Therefore, the aim of the study was to investigate mid-term clinical outcomes after total arterial revascularization versus conventional coronary bypassing using both arterial and venous conduits in three-vessel coronary disease.
All patients undergoing CABG are prospectively registered in the Asan Medical Center database (Seoul, Korea). This registry prospectively contains patient baseline characteristics, results of cardiac evaluations, detailed information on surgery, and perioperative complications. Between January 2003 and December 2005, 1,495 patients underwent CABG. Of them, 503 patients who underwent primary isolated CABG for three-vessel coronary disease were enrolled in the study. A total of 117 patients underwent total arterial revascularization strategy (Artery group) whereas 386 patients were treated with conventional strategy using both arterial and venous conduits (Vein group). The endpoints of the study were defined as death, myocardial infarction, stroke and repeat revascularization.
All CABGs were performed by experienced cardiac surgeons, each of whom performs 100 CABGs annually. Off-pump or conventional on pump CABG was performed at the discretion of the attending surgeon, with off-pump CABG usually performed when severe atherosclerosis was suspected along the ascending aorta and the aortic arch. Off-pump CABG was performed using one of several commercially available, suction-based, cardiac positioning and coronary artery-stabilizing devices. Conventional on pump CABG was performed using standard techniques that used roller-head pumps, membrane oxygenators, cardiotomy suction, arterial filters, cold antegrade blood cardioplegia, and moderate systemic hypothermia.
The use of total arterial grafting or conventional strategies depended on the number of distal targets requiring grafting and degree of proximal stenosis of target coronary arteries, but ultimately it was finally decided at the attending surgeon's preference. For the revascularization of the right coronary artery territory, the saphenous was proximally anastomosed to the ascending aorta in the vein group. In the artery group, the right coronary artery territory was revascularized with the radial artery which was anastomosed to left ITA or the aorta, if the length was long enough. If the length of the radial artery graft was not enough to reach the right coronary system, right ITA or gastroepiploic artery was used. Diltiazem was used routinely to avoid arterial graft spasm intraoperatively and postoperatively. The radial artery was preferentially used to target vessels with proximal stenosis of 80% or greater.
Categorical variables are presented as frequencies and percentages, and were compared using the chi-square test or Fisher's exact test. Continuous variables are expressed as mean ± SD or medians with ranges, and compared using the Student's unpaired t-test.
Kaplan-Meier curves were employed to delineate time related mortality, freedom from reintervention or major cerebrovascular events. Stratified survival curves were plotted to explore unadjusted differences for variables of interest (log-rank test).
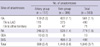
To reduce the effect of treatment selection bias and potential confounding, we performed adjustment for the differences in the baseline characteristics by use of propensity score analysis (7). The propensity scores were estimated without regard to outcome variables, with multiple logistic regression analysis. Prespecified covariates listed in Table 1 were included in the full non-parsimonious models for total arterial revascularization versus conventional coronary bypass surgery. The discrimination and calibration abilities of the propensity score model were assessed by means of C statistics and the Hosmer-Lemeshow test. The model had C statistic of 0.722 and a Hosmer-Lemeshow goodness-of-fit P value of 0.121, indicating the model was well calibrated with strong discrimination.
Cox regression or multiple logistic regression models were used to compare time related outcomes (survival, freedom from reintervention, freedom from major cerebrovascular event) or binary outcomes (early complications), respectively, with the inclusion of the treatment option (total arterial revascularization versus conventional coronary bypass surgery) and the propensity score as potential predictors of outcomes.
All reported P values were two-sided, and a value of P < 0.05 was considered statistically significant. SAS software, version 9.1 (SAS Institute, Cary, NC, USA) and SPSS version 12 were used for the statistical analysis.
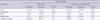
Baseline characteristics of the entire cohort are shown in Table 1. Patients in the Artery group were less likely to have hypertension and chronic renal failure, and were more likely to undergo off-pump surgery. Mean numbers of distal anastomoses were 3.4 ± 0.8 in the Artery group and 3.8 ± 1.0 in the Vein group (P < 0.001). In the Vein group, mean number of distal anastomoses using vein graft was 1.3 ± 0.6 (Median 1, range 1-4). The numbers of distal anastomses using vein grafts were one in 289 (74.9%), two in 82 (21.2%), three in 9 (2.3%) and four in 5 (1.3%). The vein grafts were used for right coronary artery territory bypassing in 351, and for left circumflex or ramus intermedius territories in 53. Propensity score matching yielded 102 pairs of patients in which there were no significant differences in baseline characteristics between the two groups including the mean number of distal anastomoses (Table 2 and 3).
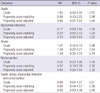
Clinical follow-up was complete in all patients (100%) with a mean follow-up duration of 6.1 ± 0.9 yr, during which there were 60 deaths, 25 reinterventions, 3 non-fatal myocardial infarctions, 18 strokes. Ninety patients experienced at least one of the major adverse events during follow-up (Table 4). There were no significant differences in the rates of death, reintervention, myocardial infarction, stroke and the composite outcomes between the Artery and the Vein groups in crude and propensity score matched comparisons (Table 4).
Twenty-five repeat-revascularizations included one case of redo-CABG (saphenous vein graft revision immediately after the operation) and 24 cases of percutaneous coronary intervention. When the myocardial ischemic events (reintervention and myocardial infarction, n = 26; two patients had both events) were analyzed according to the conduits used for bypassing, they were left ITA problem in 6 (out of 561 left ITA grafts, 1.1%), radial artery problems in 11 (out of 774 radial arteries, 1.4%), saphenous vein grafts problems in 5 (out of 498, 1.0%) and non-target territory problems in 4 (right coronary artery in 3, obtuse marginal artery in 1).
Kaplan-Meier curves for overall survival, freedom from reintervention and event-free survival in propensity score matched patients are shown in Fig. 1, and there were no significant differences in the rates of events between the two groups.
After adjustment, risks of death (hazard ratio [HR] 0.96; 95% confidence interval [CI] 0.51-1.82, P = 0.90), myocardial infarction (HR 0.20, 95% CI 0.02-2.63, P = 0.22), stroke (HR 1.29, 95% CI 0.35-4.72, P = 0.70), repeat revascularization (HR 0.64, 95% CI 0.26-1.55, P = 0.32) and the combined risk of death, myocardial infarction, stroke or repeat revascularization (HR 0.83, 95% CI 0.50-1.36, P = 0.45) were similar between the Artery group and the Vein group. For the 102 propensity score-matched pairs, similar results were obtained for all clinical endpoints (Table 5).
The present study showed that conventional coronary artery surgery in three-vessel coronary disease, compared with total arterial revascularization, demonstrated similar risks of death, myocardial infarction, stroke, reintervention and composite outcomes. In this study, we included three-vessel disease only because the importance of second and third grafts can be magnified in this subset of coronary diseases. In order to obtain mid-term clinical outcomes over 5 yr, patients enrollments were confined to those who underwent surgery before the end of 2005.
The goals of coronary artery bypass graft surgery are relief of ischemic symptoms, prevention of myocardial pumping failure and prolongation of the patient's survival. For decades, arterial grafts have been reported to have better patency rate and superior clinical results compared to venous conduits (8-10). Since the long-term survival depends on the patency of graft vessel after CABG, the excellent long-term patency and survival of left ITA (11) arguably encouraged the use of arterial graft such as radial artery, gastroepiploic artery and right ITA rather than vein graft and led to the enthusiasm to achieve total arterial revascularization. Radial artery graft shows more than 90% patency rate at 1 yr and 5 yr compared to about 85% of vein graft for left circumflex coronary artery (2, 3). It also demonstrated about 85% of patency rate at 5 yr for left circumflex coronary artery and right coronary artery (8-10). On the other hand, Hayward et al. showed that there was no difference in 5 yr patency rates between radial artery graft and saphenous vein graft (90.0% vs 87.0%) (5). Khot and co-workers reported that radial artery graft revealed lower patency rate than saphenous vein graft for left circumflex coronary artery and right coronary artery (12). Furthermore, in a study evaluating post-CABG symptomatic patients with conventional angiography, about 75% patency rate of radial artery graft was reported at mean follow-up of 27.1 months (4). Another study also demonstrated that the patency rate of radial artery graft in symptomatic patient was as low as 60% (13).
The use of bilateral ITA showed superior patency rate and survival rate than the use of radial artery graft and saphenous vein graft in triple vessel disease (14, 15). However, harvesting of bilateral ITA is technically demanding, time consuming and may cause sternal wound infection. And recent multi-center randomized trial revealed that the use of bilateral ITA were associated sternal wound reconstruction, but did not have advantages compared to the use of single ITA, in terms of myocardial infarction (2.0% vs 2.0%), cerebrovascular accident (1.5% vs 1.8%), and revascularization at 1 yr (1.8% vs 1.3%) (16). Since this report is limited by only 1-yr follow-up results, long-term follow-up data are expected to be reported.
Unlike previous studies demonstrated that superior patency rate and clinical outcomes of arterial graft (2-4), our study showed that conventional strategy using both arterial and venous conduits showed similar risks of death and major adverse outcomes on mid-term follow-up compared with total arterial revascularization for isolated three-vessel disease. We thought that many factors contributed to this result. Although radial artery graft shows superior patency rate to saphenous vein graft (2, 3, 8-10), if angiographic string sign was included in patency rate, saphenous vein graft was not inferior to radial artery graft (3).
Compromising patency rate of vein graft is due to high rate of intermediate and late graft failure, which comes from intimal and medial hyperplasia, particularly at the proximal and distal anastomosis site (17, 18). There have been advances in drug therapy, such as the use of statin medications, which may decrease the vein graft failure (19-21). Procedural factors such as less manipulation, no pressure dilatation of vein graft or no tough technique also improved a quality of vein graft, which may result in similar clinical outcomes compared with artery graft in this study.
This study is subject to the limitations inherent in retrospective work with observational data. The non-randomized design may have affected the results because of unmeasured confounders, procedure bias or detection bias, even with the use of propensity score matching. This study is not an 'intention-to-treat' based comparison and graft patency was not considered.
The concept of total arterial revascularization has been based on superior graft patency rate of arterial graft rather than venous graft on angiographic data ground. However, in clinical perspective, our results showed similar risks of death and major adverse outcomes on mid-term follow-up between two groups. Since the use of veins does not increase the risks of adverse outcomes compared with total arterial revascularization, a selection of the conduit should be more liberal.
Figures and Tables
Fig. 1
There were no significant differences in survival rate, freedom from reintervention and event-free survival rate between the Artery and the Vein groups in propensity score matched population. (A) Survival rate. (B) Freedom from reintervention. (C) Event-free survival rate.

References
1. Cameron A, Davis KB, Green G, Schaff HV. Coronary bypass surgery with internal-thoracic-artery grafts--effects on survival over a 15-year period. N Engl J Med. 1996. 334:216–219.
2. Collins P, Webb CM, Chong CF, Moat NE. Radial artery versus saphenous vein patency randomized trial: five-year angiographic follow-up. Circulation. 2008. 117:2859–2864.
3. Desai ND, Cohen EA, Naylor CD, Fremes SE. A randomized comparison of radial-artery and saphenous-vein coronary bypass grafts. N Engl J Med. 2004. 351:2302–2309.
4. Maniar HS, Sundt TM, Barner HB, Prasad SM, Peterson L, Absi T, Moustakidis P. Effect of target stenosis and location on radial artery graft patency. J Thorac Cardiovasc Surg. 2002. 123:45–52.
5. Hayward PA, Gordon IR, Hare DL, Matalanis G, Horrigan ML, Rosalion A, Buxton BF. Comparable patencies of the radial artery and right internal thoracic artery or saphenous vein beyond 5 years: results from the Radial Artery Patency and Clinical Outcomes trial. J Thorac Cardiovasc Surg. 2010. 139:60–65.
6. Eagle KA, Guyton RA, Davidoff R, Edwards FH, Ewy GA, Gardner TJ, Hart JC, Herrmann HC, Hillis LD, Hutter AM Jr, et al. ACC/AHA 2004 guideline update for coronary artery bypass graft surgery: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to Update the 1999 Guidelines for Coronary Artery Bypass Graft Surgery). Circulation. 2004. 110:e340–e437.
7. D'Agostino RB Jr. Propensity score methods for bias reduction in the comparison of a treatment to a non-randomized control group. Stat Med. 1998. 17:2265–2281.
8. Acar C, Ramsheyi A, Pagny JY, Jebara V, Barrier P, Fabiani JN, Deloche A, Guermonprez JL, Carpentier A. The radial artery for coronary artery bypass grafting: clinical and angiographic results at five years. J Thorac Cardiovasc Surg. 1998. 116:981–989.
9. Possati G, Gaudino M, Alessandrini F, Luciani N, Trani C, Cellini C, Canosa C, Di Sciascio G. Midterm clinical and angiographic results of radial artery grafts used for myocardial revascularization. J Thorac Cardiovasc Surg. 1998. 116:1015–1021.
10. Taggart DP, D'Amico R, Altman DG. Effect of arterial revascularisation on survival: a systematic review of studies comparing bilateral and single internal mammary arteries. Lancet. 2001. 358:870–875.
11. Loop FD, Lytle BW, Cosgrove DM, Stewar RW, Goormastic M, Williams GW, Golding LA, Gill CC, Taylor PC, Sheldon WC, et al. Influence of the internal-mammary-artery graft on 10-year survival and other cardiac events. N Engl J Med. 1986. 314:1–6.
12. Khot UN, Friedman DT, Pettersson G, Smedira NG, Li J, Ellis SG. Radial artery bypass grafts have an increased occurrence of angiographically severe stenosis and occlusion compared with left internal mammary arteries and saphenous Vein Grafts. Circulation. 2004. 109:2086–2091.
13. Weinschelbaum EE, Macchia A, Caramutti VM, Machain HA, Raffaelli HA, Favaloro MR, Favaloro RR, Dulbecco EA, Abud JA, Laurentiis MD, et al. Myocardial revascularization with radial and mammary arteries: initial and mid-term results. Ann Thorac Surg. 2000. 70:1378–1383.
14. Tatoulis J, Buxton BF, Fuller JA. The right internal thoracic artery: the forgotten conduit--5,766 patients and 991 angiograms. Ann Thorac Surg. 2011. 92:9–17.
15. Navia D, Vrancic M, Vaccarino G, Piccinini F, Raich H, Florit S, Thierer J. Total arterial off-pump coronary revascularization using bilateral internal thoracic arteries in triple-vessel disease: Surgical technique and clinical outcomes. Ann Thorac Surg. 2008. 86:524–530.
16. Taggart DP, Altman DG, Gray AM, Lees B, Nuqara F, Yu LM, Campbell H, Flather M. Randomized trial to compare bilateral vs. single internal mammary coronary artery bypass grafting: 1-year results of the Arterial Revascularisation Trial (ART). Eur Heart J. 2010. 31:2470–2481.
17. Motwani JG, Topol EJ. Aortocoronary saphenous vein graft disease. Pathogenesis, predisposition and prevention. Circulation. 1998. 97:916–931.
18. Campeau L. Lipid lowering and coronary bypass graft surgery. Curr Opin Cardiol. 2000. 15:395–399.
19. Kulik A, Ruel M. Statins and coronary artery bypass graft surgery: preoperative and postoperative efficacy and safety. Expert Opin Drug Sa. 2009. 8:559–571.
20. Shukla N, Angelini GD, Wan I, Jeremy JY. Potential role of nitroaspirins in the treatment of vein graft failure. Ann Thorac Surg. 2003. 75:1437–1442.
21. Wan S, Yim A, Shukla N, Johnson JL, Angelini GD, Jeremy JY. Nitric oxide donating aspirin (NCX 4016) inhibits neointimal thickening in a pig model of saphenous vein into carotid artery interposition grafting: a comparison with aspirin and morpholinosydnonimine. J Thorac Cardiovasc Surg. 2007. 134:1033–1039.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download