Abstract
It is difficult to differentiate pathogens responsible for pneumonia or colonization in patients with an endotracheal tube or in patients that have undergone tracheostomy. We evaluated the clinical usefulness of quantitative endotracheal aspirates cultures and sought to determine the result threshold level for positivity. The authors performed this retrospective cohort study between December 1, 2004 and January 31, 2006. Forty-five suspected pneumonia patients admitted to an intensive care unit (ICU) with quantitative bronchoalveolar lavage (BAL) and endotracheal aspirate (EA) culture results were enrolled. Using a threshold of 105 cfu/mL, 10 of the 45 (22.2%) quantitative EA cultures were positive, as compared with 7 (15.6%) BAL cultures. When BAL culture findings were used as the reference, the sensitivity and specificity of quantitative EA cultures were 85.7% and 89.5%, respectively, at a threshold of 105 cfu/mL, and 85.7% and 94.7%, respectively, at a threshold of 106 cfu/mL. Of the 10 EA culture positive patients, 2 patients with a result of -105 cfu/mL were BAL culture negative. The quantitative EA culture is a useful non-invasive tool for the diagnosis of pneumonia pathogens. It is suggested that a threshold level of 106 cfu/mL is appropriate.
The accurate diagnosis of newly developed pneumonia is difficult in patients with an endotracheal tube or tracheostomy (1), since many other conditions, such as, tracheobronchitis (2), pulmonary edema, and atelectasis, can mimic pneumonia. Therefore bacteriologic tests are necessary to confirm pneumonia; Infectious Diseases Society of America/American Thoracic Society (IDSA/ATS) guideline is that samples of lower respiratory tract secretions should be obtained from all patients with suspected hospital acquired pneumonia (HAP) which should be collected before antibiotic changes. Samples can include an endotracheal aspirate, bronchoalveolar lavage sample, or protected specimen brush sample (2).
But qualitative endotracheal aspirate (EA) culture cannot differentiate colonization from infection (3, 4). Although quantitative culture of bronchoalveolar lavage (BAL) fluid obtained by bronchoscopy can accurately diagnose pneumonia, this procedure is invasive and cannot be utilized in some patients, especially in those who are critical (5-12).
Quantitative EA culture is non-invasive, easily learnt, and cheaper than quantitative BAL fluid culture (4, 13); and previous results have suggested that EA can be used as a substitute for BAL in quantitative cultures (4). However, this issue is controversial and result thresholds have not been determined. Furthermore, little data is available on quantitative EA cultures in Korea, or on the clinical applications of this methodology. Accordingly, we evaluated the clinical usefulness of quantitative EA cultures in intensive care unit (ICU) patients with pneumonia, and sought to determine the result threshold level for positivity.
We performed this retrospective cohort study between December 1, 2004 and January 31, 2006. Patients with an endotracheal tube or tracheostomy suspected of having pneumonia admitted to medical ICU at the Asan Medical Center were enrolled whose EA sample was collected within 2 days of a BAL sample. Patients with community acquired, hospital acquired, and health care associated pneumonia were included, as were immunocompromised or immunocompetent patients, who had previously received antibiotics. However, patients a with lower clinical pulmonary infection score (CPIS) of < 6 or with an interval between BAL fluid and EA sampling of > 48 hr were excluded.
We evaluated patient demographic data, hospital courses, microbiologic results, the use of antibiotics, and radiographic changes. Acute physiology and chronic health evaluation (APACHE) II scores were determined at ICU admission, and CPIS scores on the first and third days after the onset of hospital acquired pneumonia.
EA samples with > 10 epithelial cells per low power field on a Gram stained slide of a direct smear were rejected as inadequate for culture. EA cultures were quantified using calibrated loops. Briefly, each 1 microliter of EA itself and 100-fold diluted EA were evenly streaked with 1 microliter-disposable plastic loop on entire surface of a chocolate agar plate, a sheep blood agar plate, and a MacConkey agar plate. Plates are incubated overnight in a 5% CO2 atmosphere at 35℃. Colonies were then counted and bacterial concentrations (cfu/mL) were calculated. Microorganisms with counts > 104 cfu/mL were submitted for identification and antimicrobial susceptibility testing. If no growth was detected on any plate, the incubation was extended for 24 hr.
Statistical analysis was performed using SPSS version 10.0 (SPSS, Chicago, IL, USA). Results are expressed as means ± SDs. The chi-square test was used to compare proportions. Threshold levels of 105, 106, and 107 cfu/mL were used to evaluate quantitative EA culture positivity, but quantitative BAL culture positivity was defined as 104 cfu/mL, which is an established threshold level. Sensitivity, specificity, and the predictive values of quantitative EA cultures were calculated at each of the three threshold levels. Kappa analysis was used to determine concordance rates between quantitative EA and BAL culture results.
A total of 45 patients (32 men, 13 women, mean age 63.4 ± 13.2 yr) were enrolled. Patient demographic data is provided in Table 1. Twenty-eight patients had hospital acquired pneumonia and 17 had community acquired pneumonia (CAP). Their underlying diseases included malignancy, chronic lung disease, rheumatologic disease, and others. The majority of patients (n = 36) were immunocompromised, and 17 of these had previously received chemotherapeutic agents, corticosteroids, or immunosuppressive agents. The major cause of ICU admission was respiratory failure and hypoxemia. Total patients' mean APACHE II score at ICU admission was 29.4 ± 7.3. In patients with hospital acquired pneumonia, mean CPIS scores on days 1 and 3 after pneumonia onset were 8.7 ± 2.0 and 8.5 ± 2.0, respectively.
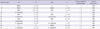
Table 2 shows the hospital courses of the patients. Mean length of ICU stay was 29.8 ± 26.8 days and mean duration of mechanical ventilation was 26.4 ± 25.3 days. The average time between BAL and EA sampling was 0.2 ± 0.9 days. Using a threshold of 105 cfu/mL, 10 (22.2%) quantitative EA cultures were positive, as compared with 7 (15.6%) BAL cultures (Table 3). Six of the 7 patients with a positive BAL cultures had a positive EA culture. Of the 10 EA culture (+) patients, 2 patients with 105 cfu/mL had all BAL culture (-), and of the 8 EA culture (+) patients (at a threshold of 106 cfu/mL), 6 were BAL culture (+).
We calculated the diagnostic efficiencies of quantitative EA culture at each threshold level. When BAL culture findings were used as reference, the sensitivity and specificity of quantitative EA culture at a threshold of 105 cfu/mL were 85.7% and 89.5%, respectively and at a threshold of 106 cfu/mL, these were 85.7% and 94.7%, respectively (Table 4). Kappa analysis showed that the concordance rate of the two diagnostic methods was best at a quantitative EA culture threshold of 106 cfu/mL. The area under the ROC curve of quantitative EA culture at this threshold was 0.902 (Fig. 1).
After obtaining culture results, antibiotic regimens were altered in 19 (42%) of the 45 patients. In 16 (36%) patients, antibiotics were deescalated and these included 12 patients on vancomycin because of a lack of evidence of methicillin-resistant Staphylococcus aureus infection. When we evaluated positivity rates with respect to time of antibiotic use before BAL, we observed higher positivity rate in patients who had received antibiotics for 7 days or longer (P = 0.017).
This study shows that quantitative endotracheal aspirate culture is a useful non-invasive tool for the diagnosis of pneumonia pathogens in critically ill patients. Our findings suggest that a threshold level of 106 cfu/mL is appropriate because at this level excellent concordance was found with quantitative BAL culture results.
Ventilator associated pneumonia (VAP) or severe CAP is difficult to diagnosis in ICU patients with an endotracheal tube or a tracheostomy. It is associated with high mortality and morbidity rates (14). Thus, early and accurate diagnosis and appropriate empirical antibiotic treatment are important outcome variables (14).
Many clinical conditions mimic pneumonia in these patients, which in practice, means that microbiologic evaluations are required for the diagnosis of pneumonia. However, it is difficult to obtain specimens from the lower respiratory tract without contamination by colonizing bacteria. Therefore culture results are invariably often difficult to interpret. Since qualitative cultures are unable to distinguish between pathogens and colonizing bacteria, the concept of quantitative culture was developed based on BAL, protected specimen brush (PSB), blinded protected telescoping catheter, and EA cultures (15-21).
Quantitative EA cultures are straightforward, cheap, easily performed, and non-invasive and have been shown to be useful in Western countries (22-26). Previous studies included comparative evaluations of the accuracy of quantitative EA cultures for the diagnosis of VAP versus other diagnostic methods, such as, autopsy specimen, BAL, or PSB culture, or clinical methods (22, 24-28). In general, each of these methods is of clinical value, primarily because of the invasive nature of bronchoscopy (5-12), but their sensitivities and specificities vary. Additionally positivity thresholds are controversial, 105 cfu/mL (22, 26, 29), or 106 cfu/mL (24, 25, 27).
No reference autopsy specimen was available for this study. Therefore we used quantitative BAL cultures and clinical diagnosis as diagnostic standards to confirm the presence of pneumonia.
When we compared the sensitivity, specificity, and concordance of quantitative EA and quantitative BAL culture, we found that the optimal quantitative EA culture threshold level was 106 cfu/mL.
Furthermore, in patients with hospital acquired pneumonia, we also used CPIS (30). No patient with HAP had a CPIS score of < 6 on day 1 and 3 after pneumonia onset, so this study showed high specificity (94.7%) than previous studies that did not use it (24, 25, 27).
When 104 cfu/mL was used as a cutoff value for quantitative BAL cultures, we found that 15.6% of BAL cultures were positive, which is lower than previous studies. This may have been low because we do not routinely perform quantitative BAL culture in critically ill patients with suspected pneumonia. We performed quantitative BAL culture in ICU patients with a poor clinical response to a previous empirical regimen or atypical clinical symptoms or signs. So we might enrolled many difficult patients to diagnose or patients suspected of having an atypical pathogens. Furthermore, many of the cultured bacteria were drug resistant organisms. These may be partially explained by culture positivity rate was high in patients with prolonged antibiotic use rather than short term antibiotic use. Only one CAP patient showed positive EA culture and the others were HAP patients. We had more HAP patients (HAP 28/CAP 17 patients) and most of CAP patients received antibiotics initiation before BAL. When we included in patients with HAP only, EA and BAL culture rates were 32.1% and 25% respectively.
In our cohort, the antibiotic regimen was changed in 19 patients, including 12 maintained on antibiotics after vancomycin discontinuance, and these actions were taken based on our quantitative culture results. Thus, quantitative EA culture is likely to reduce antibiotic use.
Several study limitations should be borne in mind. First, this was not a randomized controlled study. Besides BAL was not performed routinely in all patients with pneumonia or in patients that responded well to antibiotics due to its invasiveness. Accordingly, this study was performed in patients who had contracted a difficult pathogen to diagnose. In addition, we also included many patients who had been previously treated with antibiotics, and we enrolled community and hospital acquired pneumonia cases.
Summarizing, quantitative EA cultures are useful non-invasive diagnostic tool in critically ill patients with an endotracheal tube or tracheostomy suspected of having pneumonia especially in HAP. It is also suggested that the appropriate threshold level for quantitative EA culture is 106 cfu/mL.
Figures and Tables
Table 2
Patient characteristics at ICU admission, clinical pulmonary infection score (CPIS) on days 1 and 3 after pneumonia onset in patients with hospital acquired pneumonia and hospital courses (days)

AUTHOR SUMMARY
Usefulness of Quantitative Endotracheal Aspirate Cultures in Intensive Care Unit Patients with Suspected Pneumonia
Yoon Mi Shin, Yeon-Mok Oh, Mi Na Kim, Tae Sun Shim, Chae-Man Lim, Sang Do Lee, Younsuck Koh, Woo Sung Kim, Dong Soon Kim and Sang-Bum Hong
This study shows that quantitative endotracheal aspirate culture is a useful non-invasive tool for the diagnosis of pneumonia pathogens in critically ill patients. A threshold level of 106 cfu/mL is appropriate because excellent concordance with quantitative BAL culture results was found.
References
1. Baughman RP. Diagnosis of ventilator-associated pneumonia. Microbes Infect. 2005. 7:262–267.
2. American Thoracic Society. Infectious Diseases Society of America. Guidelines for the management of adults with hospital-acquired, ventilator-associated, and healthcare-associated pneumonia. Am J Respir Crit Care Med. 2005. 171:388–416.
3. Lambotte O, Timsit JF, Garrouste-Orgeas M, Misset B, Benali A, Carlet J. The significance of distal bronchial samples with commensals in ventilator-associated pneumonia: colonizer or pathogen? Chest. 2002. 122:1389–1399.
4. Albert S, Kirchner J, Thomas H, Behne M, Schur J, Brade V. Role of quantitative cultures and microscopic examinations of endotracheal aspirates in the diagnosis of pulmonary infections in ventilated patients. J Hosp Infect. 1997. 37:25–37.
5. Tsai SH, Cohen SS, Fenger EP. Bronchial perforation as a complication of bronchoscopy. Am Rev Tuberc. 1958. 78:106–110.
6. Prakash UB, Offord KP, Stubbs SE. Bronchoscopy in North America: the ACCP survey. Chest. 1991. 100:1668–1675.
7. Jolliet P, Chevrolet JC. Bronchoscopy in the intensive care unit. Intensive Care Med. 1992. 18:160–169.
8. Valentine VG, Rizk NW, Hancock EW. A complication during bronchoscopy. Hosp Pract (Off Ed). 1993. 28:22. 27.
9. Pereira W, Kovnat DM, Khan MA, Iacovino JR, Spivack ML, Snider GL. Fever and pneumonia after flexible fiberoptic bronchoscopy. Am Rev Respir Dis. 1975. 112:59–64.
10. Kiss K, Pápai Z, Szima B, Kis S, Strausz J. Fiberoptic bronchoscopy in intensive care units. Orv Hetil. 1996. 137:1689–1691.
11. Hammer DL, Aranda CP, Galati V, Adams FV. Massive intrabronchial aspiration of contents of pulmonary abscess after fiberoptic bronchoscopy. Chest. 1978. 74:306–307.
12. Friedman RL. Selective pneumothorax: a complication of bronchoscopy. Dis Chest. 1955. 27:213–215.
13. Bergmans DC, Bonten MJ, De Leeuw PW, Stobberingh EE. Reproducibility of quantitative cultures of endotracheal aspirates from mechanically ventilated patients. J Clin Microbiol. 1997. 35:796–798.
14. Chastre J, Fagon JY. Ventilator-associated pneumonia. Am J Respir Crit Care Med. 2002. 165:867–903.
15. Brun-Buisson C, Fartoukh M, Lechapt E, Honoré S, Zahar JR, Cerf C, Maitre B. Contribution of blinded, protected quantitative specimens to the diagnostic and therapeutic management of ventilator-associated pneumonia. Chest. 2005. 128:533–544.
16. Clec'h C, Jauréguy F, Hamza L, Karoubi P, Fosse JP, Hamdi A, Vincent F, Gonzalez F, Cohen Y. Agreement between quantitative cultures of postintubation tracheal aspiration and plugged telescoping catheter, protected specimen brush, or BAL for the diagnosis of nosocomial pneumonia. Chest. 2006. 130:956–961.
17. Cook D, Mandell L. Endotracheal aspiration in the diagnosis of ventilator-associated pneumonia. Chest. 2000. 117:4 Suppl 2. 195S–197S.
18. Elatrous S, Boukef R, Ouanes Besbes L, Marghli S, Nooman S, Nouira S, Abroug F. Diagnosis of ventilator-associated pneumonia: agreement between quantitative cultures of endotracheal aspiration and plugged telescoping catheter. Intensive Care Med. 2004. 30:853–858.
19. Fangio P, Rouquette-Vincenti I, Rousseau JM, Soullié B, Brinquin L. Diagnosis of ventilator-associated pneumonia: a prospective comparison of the telescoping plugged catheter with the endotracheal aspirate. Ann Fr Anesth Reanim. 2002. 21:184–192.
20. Fujitani S, Yu VL. Diagnosis of ventilator-associated pneumonia: focus on nonbronchoscopic techniques (nonbronchoscopic bronchoalveolar lavage, including mini-BAL, blinded protected specimen brush, and blinded bronchial sampling) and endotracheal aspirates. J Intensive Care Med. 2006. 21:17–21.
21. Papazian L, Thomas P, Garbe L, Guignon I, Thirion X, Charrel J, Bollet C, Fuentes P, Gouin F. Bronchoscopic or blind sampling techniques for the diagnosis of ventilator-associated pneumonia. Am J Respir Crit Care Med. 1995. 152:1982–1991.
22. el-Ebiary M, Torres A, González J, de la Bellacasa JP, García C, Jiménez de Anta MT, Ferrer M, Rodriguez-Roisin R. Quantitative cultures of endotracheal aspirates for the diagnosis of ventilator-associated pneumonia. Am Rev Respir Dis. 1993. 148:1552–1557.
23. Michel F, Franceschini B, Berger P, Arnal JM, Gainnier M, Sainty JM, Papazian L. Early antibiotic treatment for BAL-confirmed ventilator-associated pneumonia: a role for routine endotracheal aspirate cultures. Chest. 2005. 127:589–597.
24. Marquette CH, Georges H, Wallet F, Ramon P, Saulnier F, Neviere R, Mathieu D, Rime A, Tonnel AB. Diagnostic efficiency of endotracheal aspirates with quantitative bacterial cultures in intubated patients with suspected pneumonia. Comparison with the protected specimen brush. Am Rev Respir Dis. 1993. 148:138–144.
25. Torres A, Martos A, Puig de la Bellacasa J, Ferrer M, el-Ebiary M, González J, Gené A, Rodríguez-Roisin R. Specificity of endotracheal aspiration, protected specimen brush, and bronchoalveolar lavage in mechanically ventilated patients. Am Rev Respir Dis. 1993. 147:952–957.
26. Sauaia A, Moore FA, Moore EE, Haenel JB, Kaneer L, Read RA. Diagnosing pneumonia in mechanically ventilated trauma patients: endotracheal aspirate versus bronchoalveolar lavage. J Trauma. 1993. 35:512–517.
27. Jourdain B, Novara A, Joly-Guillou ML, Dombret MC, Calvat S, Trouillet JL, Gibert C, Chastre J. Role of quantitative cultures of endotracheal aspirates in the diagnosis of nosocomial pneumonia. Am J Respir Crit Care Med. 1995. 152:241–246.
28. Marquette CH, Copin MC, Wallet F, Neviere R, Saulnier F, Mathieu D, Durocher A, Ramon P, Tonnel AB. Diagnostic tests for pneumonia in ventilated patients: prospective evaluation of diagnostic accuracy using histology as a diagnostic gold standard. Am J Respir Crit Care Med. 1995. 151:1878–1888.
29. Wu CL, Yang Dle, Wang NY, Kuo HT, Chen PZ. Quantitative culture of endotracheal aspirates in the diagnosis of ventilator-associated pneumonia in patients with treatment failure. Chest. 2002. 122:662–668.
30. Singh N, Rogers P, Atwood CW, Wagener MM, Yu VL. Short-course empiric antibiotic therapy for patients with pulmonary infiltrates in the intensive care unit. A proposed solution for indiscriminate antibiotic prescription. Am J Respir Crit Care Med. 2000. 162:505–511.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download