Abstract
Aneurysms of the major thoracic veins are rare. They are usually asymptomatic and thus treated conservatively. We report an extremely rare case of rapidly progressing superior vena cava (SVC) aneurysm complicated by thrombosis and acute pulmonary thromboembolism (PTE) with right ventricular dysfunction. Thrombolytic therapy for hemodynamically significant acute PTE was harmful to the patient in the present case, because it induced further thrombosis and mobilization of the thrombi within the aneurysm, subsequently causing de novo PTE. Surgical aneurysmectomy combined with pulmonary artery embolectomy would be a treatment of choice in patients with SVC aneurysm complicated by acute PTE.
Aneurysms of the major thoracic veins are rare. Because they are usually asymptomatic, they are diagnosed incidentally during the evaluation of mediastinal widening on chest roentgenography and treated conservatively (1-3). Development of complications such as rupture, venous obstruction, and thrombosis has been described and may require surgery (4-6). We report a 55-yr old male patient with superior vena cava (SVC) aneurysm which showed rapid progression and complicated by thrombosis and hemodynamically significant acute pulmonary thromboembolism (PTE) with review of the literature.
A 55-yr-old male presented with acute chest pain, dyspnea, and hypotension on December 8, 2009. The patient has been followed without any medications for incidentally detected asymptomatic SVC aneurysm for last 2 yr (Fig. 1A), and the size of the SVC aneurysm did not change (Fig. 1B). Chest radiography at admission showed marked widening of the right middle mediastinum due to abnormal soft-tissue density suggesting the rapid expansion of previously noted SVC aneurysm (Fig. 1C). Echocardiography revealed marked enlargement and hypokinesia of the right ventricle (RV) with moderate pulmonary hypertension suggesting acute PE. Chest computed tomographic angiography (CTA) showed about 6.9 × 6.1 × 9.9 cm sized lobulated giant saccular aneurysm originating from mainly SVC and partially involving left brachiocephalic vein with internal thrombi (Fig. 2A). Considerable amounts of thromboembolic filling defects in left pulmonary artery, both left and right lobar, segmental, and subsegmental arteries were also noted (Fig. 2B). Three-dimensional reconstruction with endovascular views showed the giant saccular SVC aneurysm with 4.1 × 3.7 cm sized internal thrombi, and the thrombi protruded into the SVC through the narrow aneurysmal neck (Fig. 2C, D). Venous CTA of the lower extremities and abdominal CTA showed no evidence of deep vein thrombosis or other venous aneurysms. To exclude the possible hypercoagulable status as a cause of pulmonary thromboembolism, the laboratory tests for hypercoagulability was done and revealed no abnormalities. Surgical exclusion of SVC aneurysm with pulmonary embolectomy was planned, but the patient and family refused surgery. Therefore, thrombolytic therapy using recombinant tissue plasminogen activator with the dose of 200 mg was administered intravenously for 2 hr for hemodynamically significant PTE, and the RV function and pulmonary artery pressure was normalized on FU echocardiography. However, the patient complained recurrent chest pain and dyspnea on the next day. FU CTA revealed more decreased amounts of thrombi in the left pulmonary artery and its branches, but the amounts of thrombi in the SVC aneurysm, SVC, right pulmonary artery and its branches were increased. Mobilization of thrombi from the SVC aneurysm due to thrombolytic therapy was the possible cause of recurrent PTE, and it was expected that further embolization of thrombi would be fatal to the patient. Therefore, surgical treatment was strongly recommended. Resection of SVC aneurysm and pulmonary artery embolectomy were performed successfully. At surgery, femoral arterial and venous cannulation was done to prepare for accidental rupture of aneurysm during sternotomy. After dissection of the aneurysm, the other venous cannulation at the innominate vein and isolation of the proximal and distal portion of the aneurysm was done. Under cardiopulmonary bypass, aneurysmal wall was opened longitudinally after snaring of proximal and distal portion of the aneurysm and innominate vein. Aenurysm which contained fresh thrombi was thin-walled and had relatively normal venous endothelium grossly (Fig. 3A), and the histopathologic examination showed compatible findings of true aneurysm (Fig. 3B). Thin-walled aneurysmal wall was completely resected and subsequent reconstruction of the superior vena cava was performed with glutaraldehyde fixed autologuous pericardium that was already harvested. Outer surface of the pericardium was buttressed with Dacron to prevent potential formation of pseudoaneurysm. A transverse arteriotomy was made in the pulmonary trunk to the left main pulmonary artery and another incision was made in the right main pulmonary artery, and the fresh and organized thrombi were gently extracted. Following the successful surgical management, the mediastinal widening on chest radiography was normalized (Fig. 1D) and the patient was recovered without any postoperative events. The patient was discharged and treated by anticoagulation with warfarin for 6 months to achieve complete resolution of the possible remained pulmonary arterial thrombi.
Aneurysms of the major thoracic veins are rare and usually asymptomatic, even though several complications including aneurysmal rupture, thrombosis, or venous obstructions have been reported (4-6). However, the development of acute PTE associated with thrombosed venous aneurysms, like the present case, is extremely rare. There had been only 2 cases of acute PTE caused by thrombosis of the major intrathoracic venous aneurysms in the literature (7, 8).
The present case gives several important messages in the treatment of asymptomatic or complicated intrathoracic venous aneurysms. First, although the SVC aneurysm did not produce any kind of symptoms or size change for 2 yr, the present case showed sudden rapid growing of the aneurysms with internal thrombus formation. Therefore, the benefit of surgical therapy to prevent the developments of fatal complications should be considered in saccular SVC aneurysm at the time of diagnosis, even in asymptomatic cases. In case of fusiform SVC aneurysm, conservative management is recommended in the general consensus. Second, long-term anticoagulation with warfarinization might be considered to prevent aneurysmal thrombosis and subsequent PTE, especially in a fusiform aneurysm. In case of saccular aneurysm, however, rupture of the aneurysm is the major complication in addition to thromboembolism. In case of rupture during anticoagulation, it can be a disaster. Therefore, the benefit of anticoagulation should be counter-balanced by the risk of rupture. Third, surgical aneurysmectomy and pulmonary artery embolectomy would be a treatment of choice in patients with SVC aneurysm complicated by thrombosis and massive PE as discussed in the previous reports (4-8).
In conclusion, we report a very rare case of SVC aneurysm which showed rapid expansion and complicated by thrombosis. The acute RV dysfunction may be caused by massive PTE from the thrombosed SVC aneurysm and improved by surgical aneurysmectomy and embolectomy.
Figures and Tables
Fig. 1
Serial radiographic changes of the superior vena cava (SVC) aneurysm. Chest radiography at 2 yr ago (A) and 1 month (B) ago revealed the SVC aneurysm without any changes in size. The SVC aneurysm was markedly increased in size on chest radiography at admission (C) and disappeared after surgery (D).
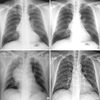
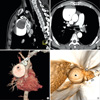
Fig. 2
Multiplanar reformat images (A, B) and three-dimensional volume rendered images (C, D) of chest computed tomographic angiography demonstrated the superior vena cava (SVC) aneurysm with internal thrombi (★) protruding into the SVC through the narrow neck (arrow head in A and D) and pulmonary arterial embolism (arrow heads in B).
References
1. Schatz IJ, Fine G. Venous aneurysms. N Engl J Med. 1962. 266:1310–1312.
2. Rappaport DC, Ros PR, Moser RP Jr. Idiopathic dilatation of the thoracic venous system. Can Assoc Radiol J. 1992. 43:385–387.
3. Koga S, Ikeda S, Sanuki Y, Ninomiya A, Izumikawa T, Miyahara Y, Kohno S. A case of asymptomatic fusiform aneurysm of the superior vena cava detected by magnetic resonance imaging. Int J Cardiol. 2006. 113:e39–e41.
4. Taira A, Akita H. Ruptured venous aneurysm of the persistent left superior vena cava. Angiology. 1981. 32:656–659.
5. Pasic M, Schöpke W, Vogt P, von Segesser L, Schneider J, Turina M. Aneurysm of the superior mediastinal veins. J Vasc Surg. 1995. 21:505–509.
6. Gomez MA, Delhommais A, Presicci PF, Besson M, Roger R, Alison D. Partial thrombosis of an idiopathic azygos vein aneurysm. Br J Radiol. 2004. 77:342–343.
7. Ream CR, Giardina A. Congenital superior vena cava aneurysm with complications caused by infectious mononucleosis. Chest. 1972. 62:755–757.
8. Nakamura Y, Nakano K, Nakatani H, Fukuda T, Honda K, Homma N. Surgical exclusion of a thrombosed azygos vein aneurysm causing pulmonary embolism. J Thorac Cardiovasc Surg. 2007. 133:834–835.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download