Abstract
Heart transplantation is now regarded as the treatment of choice for end-stage heart failure. To improve long-term results of the heart transplantation, we analyzed causes of death relative to time after transplantation. A total of 201 consecutive patients, 154 (76.6%) males, aged ≥ 17 yr underwent heart transplantation between November 1992 and December 2008. Mean ages of recipients and donors were 42.8 ± 12.4 and 29.8 ± 9.6 yr, respectively. The bicaval anastomosis technique was used since 1999. Mean follow up duration was 6.5 ± 4.4 yr. Two patients (1%) died in-hospital due to sepsis caused by infection. Late death occurred in 39 patients (19.4%) with the most common cause being sepsis due to infection. The 1-, 5-, and 10-yr survival rates in these patients were 95.5% ± 1.5%, 86.9% ± 2.6%, and 73.5% ± 4.1%, respectively. The surgical results of heart transplantation in adults were excellent, with late mortality due primarily to infection, malignancy, and rejection. Cardiac deaths related to cardiac allograft vasculopathy were very rare.
Heart failure is related primarily to advanced age (1, 2). The number of patients with end-stage heart failure has been increasing due to increasing mean life expectancy. Heart transplantation has become the treatment of choice for patients with end-stage heart failure. Tremendous advances in immunosuppression, rejection control, and infection control have improved the results of heart transplantation (3). Currently, the operative mortality rate is 5%-10% and the 1-yr survival rate is as high as 85%, with survival thereafter decreasing linearly (3.4% per year). The most common causes of death in the first 30 days after transplantation are graft failure, multi-organ failure, and infection, with infection, graft failure, and acute rejection being the most common causes of death within 1 yr of transplant. After 1 yr, cardiac allograft vasculopathy and malignancy are the most common causes of death (4).
Most of these studies, however, have been performed in Western countries and little is known about postoperative mortality in Asian countries. In our institute, the first heart transplant was performed in 1992, with more than 200 adult heart transplantations performed since then. To improve the long-term survival of adult heart transplant recipients, it is important to determine the causes of death relative to time after transplant. We therefore analyzed the causes of death among patients undergoing heart transplantation at our institute according to post-operative period.
Between November 1992 and December 2008, 201 adult patients (aged ≥ 17 yr) underwent orthotopic heart transplantation. We excluded patients who underwent re-transplantation.
The annual number of operations has been increasing, except around the time of settlement of Korea Organization of National Organ Service in 2000 (Fig. 1). The mean age of recipients was 42.8 ± 12.4 yr and 154 (76.6%) were male. Almost all patients were NYHA functional class III (n = 99) or IV (n = 100), except for two patients who were diagnosed with cardiac tumors. Three patients underwent kidney transplantation concomitantly. Two patients were being treated preoperatively with mechanical assistance devices (extracorporeal membrane oxygenation: ECMO and ventricular assist device: VAD).
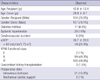
The most common diagnoses requiring heart transplantation were dilated cardiomyopathy (n = 142, 70.6%), ischemic cardiomyopathy (n = 22, 10.9%), and hypertrophic cardiomyopathy (n = 7, 3.5%). Preoperative demographic and diagnostic data are summarized in Table 1.
In the early part of the study period, from November 1992 to December 1998, all operations were performed according to the standard technique as described by Lower et al. (5). Operative procedures of our institute were described in the previous report (6). Since January 1999, we have used the bicaval technique described by Saram and colleagues (7, 8). Overall, the standard technique was used in 53 patients and the bicaval technique in 148. Myocardial protection of the donor heart was performed by infusion of 2,000 mL of 4℃ Custodiol® HTK solution. The harvested heart was rinsed in Custodiol® HTK solution and transported in the same solution in an ice box. Mean ischemic time was 132 ± 52 min.
From November 1992 to June 1999, the preoperative immunosuppressive protocol, used in 60 patients, consisted of induction with cyclosporine 3-5 mg/kg and azathioprine 2-3 mg/kg per os (PO). After June 1999, the preoperative immunosuppressive protocol, used in 141 patients, consisted of anti-IL2 receptor monoclonal antibody (anti-IL2R mAb), mycophenolate mofetil 1.5-2.0 g PO and administration of cyclosporine 3 mg/kg PO. Cyclosporine was withheld if serum creatinine (Cr) concentration was greater than 1.5 mg%. Intraoperatively, methylprednisolone 500 mg intravenous (IV) was routinely injected immediately before release of the aorta clamp. Postoperatively, patients were treated with mycophenolate mofetil 1-3 g/day and anti-IL2 R mAb to maintain a WBC count of 4,000-6,000/µL. Postoperatively, cyclosporine trough levels were maintained during the first year at 300-400 ng/mL by an enzyme-multiplied immunoassay (EMI) method and at 150-200 ng/mL thereafter. The initial postoperative dose of prednisone was 1 mg/kg/day, decreasing to 0.25 mg/kg/day at 1 month and to 0.1 mg/kg/day at 6 months.
Patients negative for HBsAg and HBsAb received HBV vaccination preoperatively. Patients also received pneumococcal vaccination routinely, with postoperative sulfamethoxazole and trimethoprim administration throughout the first year if tolerated. Recipients positive for cytomegalovirus (CMV) IgG received ganciclovir IV for 4 weeks as CMV prophylaxis. If the recipient CMV was IgG(-) but the donor CMV was IgG(+), recipients were administered IV ganciclovir for 4 weeks and then switched to oral ganciclovir 1.0 g three times a day for another 2-3 months. All patients received annual influenza vaccination.
Endomyocardial biopsy was performed to confirm acute rejection. Biopsies were taken every week for 1 month, every month for 3 months, and at 6 months and 1 and 2 yr.
Cardiac allograft vasculopathy (CAV) was evaluated by coronary angiography and recently by concomitant intravascular ultrasonography (IVUS). Of the 201 patients, 188 (93.5%) had undergone at least one coronary angiogram (CAG), with the last CAG performed at a mean 4.9 ± 3.6 yr (range, 1.0-14.5 yr) after transplantation. CAG was performed after more than 5 yr in 63 (31.3%) patients.
At our institute, a single expert cardiologist has been involved in both immediate postoperative and long-term management. This cardiologist selected the postoperative immunosuppression and infection protocols and hemodynamic monitoring for each patient. Follow-up was possible in all patients; mean follow-up duration was 6.5 ± 4.4 yr.
Data are expressed as mean ± standard deviation for continuous variables, as numbers with percentage for categorical variables. Overall survival rate was estimated by the Kaplan-Meier method, and inter-group comparisons were performed using the log-rank test. A P value <0.05 was considered significant. All statistical analyses were performed using SPSS version 14.0 (Korean version; SPSS, Inc., Chicago, IL, USA).
Two patients (1%) died in-hospital. One patient was a 57-yr-old male diagnosed with dilated cardiomyopathy who underwent transplantation using the standard technique. Postoperatively, he experienced acute renal failure due to cyclosporine toxicity and underwent hemodialysis. Endomyocardial biopsies at 10 and 17 days showed no evidence of acute rejection. Postoperative echocardiography showed normal left and right ventricular function. At 16 days, he developed left lower lobe pneumonia, which progressed rapidly. The patient died 20 days postoperatively due to septic shock.
The second patient was a 41-yr-female who had Child class C cardiac cirrhosis and azotemia. She underwent transplantation using the bicaval technique, with a total ischemia time of 103 min. She experienced biventricular failure postoperatively, for which, on day 2, an intra-aortic balloon counterpulsation (IABP) was inserted and continuous veno-veno hemodialysis was applied. Her heart function recovered and the IABP was removed 3 days later. However, she developed aspergillosis and bacterial pneumonia. Despite aggressive medical management, this patient died 65 days after the operation.
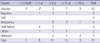
After discharge, 39 patients died. Their causes of death relative to postoperative period are summarized in Table 2.
Between 1 month and 1 yr, eight patients died, including those who died in-hospital. The most common cause of death was graft failure (n = 4). In addition, two patients died due to acute respiratory distress syndrome caused by pneumonia, one patient died due to hepatic failure caused by the hepatitis B virus, and one patient committed suicide due to financial problems.
Between 1 yr and 5 yr, malignancy was diagnosed in two patients, one each with renal cell cancer and Kaposi's sarcoma. Two patients experienced graft failure and four showed rejection of donor organs due to non-compliance with medical treatment. One patient committed suicide and three died due to sepsis caused by infection.
Between 5 yr and 10 yr, three patients died due to malignancy, including two with T-cell lymphoma and one with lung cancer. One died due to organ rejection, one due to fat embolism after total hip replacement, and seven due to infection, including meningitis in one patient, peritoneal dialysis infection in one, and pneumonia in five. One patient died due to unknown causes.
After 10 yr, one patient died due to multiple myeloma and two died due to infection-related causes, one each from pneumonia and herpes zoster infection. The other two patients died due to unknown causes.
Overall survival rates were 95.5% ± 1.5% at 1 yr, 86.9% ± 2.6% at 5 yr, 73.5% ± 4.1% at 10 yr, and 61.6% ± 5.8% at 12 yr (Fig. 2A).
The operative mortality rate among our patients was excellent, especially when compared with other reports in which early mortality rates were 5%-10% (9, 10). The much lower mortality rates we observed may be related to improvements in donor management, the preoperative status of the recipient, and postoperative management in the intensive care unit.
During the study period, there were two major changes in the perioperative management of heart transplant recipients, the use of the bicaval technique, beginning in 1999, and the introduction during 1999 of an immunosuppressive regimen consisting of anti-IL2R mAb and mycophenolate mofetil. Preoperative evaluation and postoperative management in all patients were directed by a single cardiologist.
Compared with the standard technique, the bicaval technique results in improved atrial function (11, 12), a lower rate of post-operative arrhythmias (8), a reduced need for permanent pacing (13), and decreased tricuspid regurgitation (14). In one series, use of the bicaval technique improved survival (15). In contrast, a comparison of outcomes using the bicaval and standard techniques in heart transplantation showed that neither was associated with a survival advantages (16). Although the bicaval technique seemed to be superior during the early postoperative period, we observed no differences in the long-term survival between the two groups (Fig. 2B). Because our immunosuppressive protocol also changed during the study period, we could not determine whether surgical technique affected on survival.
Traditionally, the most common causes of death during the first 30 days after transplantation are graft failure, multi-organ failure, and infection. An updated report from the registry of the International Society of Heart and Lung Transplantation showed that graft failure and infection were the most important causes of 30-day mortality (10). Because only 1 of our patients died, prior to postoperative 30 days, of infection, direct comparison was difficult. Our low mortality rates showed the effectiveness of recent advancements in myocardial protection and donor management.
Infection, graft failure, and acute rejection have been regarded as the most common causes of death within 1 yr after transplantation. We found that infection remained an important cause of death during this period, whereas graft failure was more common during this period than other post-transplant periods. Four patients died due to graft failure, at onset times of about 6 months postoperatively. Endomyocardial biopsy and echocardiography were performed within 1 month in two patients with normal contractility and no evidence of significant rejection. Another patient had experienced postoperative constrictive pericarditis.
Infection was the predominant cause of death between 5 and 10 yr. During this period, the incidences of graft failure and rejection were relatively low. Sites of infection varied and included the lungs (pneumonia), brain (meningitis), and peritoneal catheters, with pneumonia being the most common cause of death. Four patients had malignancies, including three with lymphoma and one with lung cancer.
This study had several limitations, most of them being inherent to the retrospective analysis of patients in a single center. However, the regimen of postoperative management was controlled by a single cardiologist, allowing consistent patient management during the follow-up period. The causes of death after heart transplantation were complex, so the assignment of a single cause was difficult. In most cases underlying disease was considered to be the cause of death.
In conclusion, the present study shows that the surgical mortality rates of adults who underwent heart transplantation are excellent and that long-term survival is acceptable. The most common cause of death within 1 yr is graft failure, followed by infection. Notably, none of our patients died due to cardiac allograft vasculopathy. Additional studies are necessary to assess the impact of cardiac allograft vasculopathy on survival.
Figures and Tables
Fig. 1
Annual trends of heart transplantation numbers in Asan Medical Center. Korea Organization of National Organ Service (KONOS).

Fig. 2
Overall survival rate using the Kaplan-Meier method (A) and comparison between the standard and bicaval techniques (B). YSR, year survival rate.

AUTHOR SUMMARY
Long-term Mortality in Adult Orthotopic Heart Transplant Recipients
Sung-Ho Jung, Jae Joong Kim, Suk Jung Choo, Tae-Jin Yun, Cheol Hyun Chung, and Jae Won Lee
Heart transplantation is the treatment of choice in patients wiht end-stage heart failure. To improve the long-term results of heart transplantation, we should know the causes of death after the surgery. We investigated the cases of post-operative death according to the time after transplantation in Korea. In-hospital mortality was 1% (2/201) and a 10-yr survival rate was 74%. The late mortality was primarily due to infection, malignancy, and immune rejection. The Death related with cardiac allograft vasculopathy was very rare. Further study would be necessary to analyze the differences of causes of death in Korea compared with western countries.
References
1. Fonarow GC, Abraham WT, Albert NM, Stough WG, Gheorghiade M, Greenberg BH, O'Connor CM, Sun JL, Yancy C, Young JB. OPTIMIZE-HF Investigators and Hospitals. Age- and gender-related differences in quality of care and outcomes of patients hospitalized with heart failure (from OPTIMIZE-HF). Am J Cardiol. 2009. 104:107–115.
2. Kalogeropoulos A, Georgiopoulou V, Kritchevsky SB, Psaty BM, Smith NL, Newman AB, Rodondi N, Satterfield S, Bauer DC, Bibbins-Domingo K, Smith AL, Wilson PW, Vasan RS, Harris TB, Butler J. Epidemiology of incident heart failure in a contemporary elderly cohort: the health, aging, and body composition study. Arch Intern Med. 2009. 169:708–715.
3. Hunt SA, Haddad F. The changing face of heart transplantation. J Am Coll Cardiol. 2008. 52:587–598.
4. Taylor DO, Edwards LB, Aurora P, Christie JD, Dobbels F, Kirk R, Rahmel AO, Kucheryavaya AY, Hertz MI. Registry of the International Society for Heart and Lung Transplantation: twenty-fifth official adult heart transplant report--2008. J Heart Lung Transplant. 2008. 27:943–956.
5. Lower RR, Stofer RC, Shumway NE. Homovital transplantation of the heart. J Thorac Cardiovasc Surg. 1961. 41:196–204.
6. Choo SJ, Kim JJ, Kim SP, Lee JW, Wan RS, Park NH, Lee SK, Yoo DG, Song H, Chung CH, Kim KS, Song MG. Heart transplantation. A retrospective analysis of the long-term results. Yonsei Med J. 2004. 45:1173–1180.
7. Sarsam MA, Campbell CS, Yonan NA, Deiraniya AK, Rahman AN. An alternative surgical technique in orthotopic cardiac transplantation. J Card Surg. 1993. 8:344–349.
8. el Gamel A, Yonan NA, Grant S, Deiraniya AK, Rahman AN, Sarsam MA, Campbell CS. Orthotopic cardiac transplantation: a comparison of standard and bicaval Wythenshawe techniques. J Thorac Cardiovasc Surg. 1995. 109:721–729.
9. Luckraz H, Goddard M, Charman SC, Wallwork J, Parameshwar J, Large SR. Early mortality after cardiac transplantation: should we do better? J Heart Lung Transplant. 2005. 24:401–405.
10. Taylor DO, Stehlik J, Edwards LB, Aurora P, Christie JD, Dobbels F, Kirk R, Kucheryavaya AY, Rahmel AO, Hertz MI. Registry of the International Society for Heart and Lung Transplantation: Twenty-sixth Official Adult Heart Transplant Report-2009. J Heart Lung Transplant. 2009. 28:1007–1022.
11. Leyh RG, Jahnke AW, Kraatz EG, Sievers HH. Cardiovascular dynamics and dimensions after bicaval and standard cardiac transplantation. Ann Thorac Surg. 1995. 59:1495–1500.
12. Traversi E, Pozzoli M, Grande A, Forni G, Assandri J, Viganò M, Tavazzi L. The bicaval anastomosis technique for orthotopic heart transplantation yields better atrial function than the standard technique: an echocardiographic automatic boundary detection study. J Heart Lung Transplant. 1998. 17:1065–1074.
13. Meyer SR, Modry DL, Bainey K, Koshal A, Mullen JC, Rebeyka IM, Ross DB, Bowker S, Wang S. Declining need for permanent pacemaker insertion with the bicaval technique of orthotopic heart transplantation. Can J Cardiol. 2005. 21:159–163.
14. Park KY, Park CH, Chun YB, Shin MS, Lee KC. Bicaval anastomosis reduces tricuspid regurgitation after heart transplantation. Asian Cardiovasc Thorac Ann. 2005. 13:251–254.
15. Aziz T, Burgess M, Khafagy R, Wynn Hann A, Campbell C, Rahman A, Deiraniya A, Yonan N. Bicaval and standard techniques in orthotopic heart transplantation: medium-term experience in cardiac performance and survival. J Thorac Cardiovasc Surg. 1999. 118:115–122.
16. Weiss ES, Nwakanma LU, Russell SB, Conte JV, Shah AS. Outcomes in bicaval versus biatrial techniques in heart transplantation: an analysis of the UNOS database. J Heart Lung Transplant. 2008. 27:178–183.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download