Abstract
The coexistence of cerebral infarcts and Alzheimer's disease (AD) is common, but the influence of symptomatic cerebral infarcts on cognition is uncertain in AD. We hypothesize that symptomatic cerebral infarcts may provide an additive cognitive factor contributing to dementia in the AD population. We studied 1,001 clinically probable or possible AD patients in the Alzheimer Disease Research Center (ADRC) database. Linear regression was used to evaluate for an association between symptomatic cerebral infarcts and memory, language, executive function, abstract reasoning, and visuospatial performance, separately. Models were adjusted for covariates including age, gender, education, ethnicity, hypertension, diabetes mellitus, heart disease, clinical dementia rating, the presence of silent cerebral infarcts, and multiplicity or location of infarcts. Clinical history of stroke was present in 107 patients, radiological infarcts in 308 patients, and 68 patients with both were considered to have symptomatic infarcts. Adjusting for all covariates, AD patients with symptomatic infarcts had more impairment of executive function (P < 0.05). The influence of cerebral infarcts is neither general nor diffuse, and the presence of clinical history may have a more important influence on executive performance in AD.
Both Alzheimer pathology and cerebral infarcts are common in older people, making the influence of cerebral infarcts on cognition a matter of interest (1-3). Several magnetic resonance imaging (MRI)-based studies have documented that silent or symptomatic infarcts are associated with poorer cognitive performance, cognitive decline, or increased likelihood of dementia in the community (4-6). Pure vascular dementia, although uncommon, may result from cerebral infarcts (7).
However, in Alzheimer's disease (AD) patients, the contribution of vascular lesions to cognitive impairment is uncertain. Detection of vascular cognitive burden in AD may be helpful in differentiating between mixed dementia (AD with infarcts) and pure AD, and to allow strategies to prevent recurrent vascular injury.
The results from previous studies are inconsistent. Some studies have suggested that patients with AD and concomitant cerebrovascular lesions had poorer cognitive performance than those without (8-10), whereas other studies have suggested that vascular lesions did not have an important effect on the clinical features including cognitive performance (11-13). These differing findings may be the result of different examined stages of AD (10), relative small numbers (< 30) of AD patients with cerebral infarcts (8, 10-13), and exclusion of large infarcts (8, 12, 13).
Patients with cerebral infarcts are a heterogeneous group with respect to clinical evidence (symptomatic or silent), location, volume, and multiplicity. Therefore, a larger sample may be needed to study the influence on cognition (14). Additionally, the importance of clinical history of stroke, which is often neglected in autopsy-based AD studies, might be studied together with other radiological features of cerebral infarcts and other covariates of AD to elucidate the influence of cerebral infarct in AD (11-13). Separation of symptomatic infarcts from silent infarcts is important because they have a different clinical significance in daily practice. Here we have examined the relationship of symptomatic cerebral infarcts to cognition in AD using a large database including 16 yr of data from an Alzheimer's Disease Research Center (ADRC).
The study population consisted of subjects enrolled in the ADRC at Columbia University Subjects underwent standardized clinical evaluation, which included a structured neurological and psychiatric examination, neuropsychological testing, laboratory tests, and neuroimaging. Diagnoses are determined at a weekly consensus conference. Diagnosis of AD is based on National Institute of Neurological Communicative Disorders and Stroke-Alzheimer's Disease and Related Disorders Association (NINCDS-ADRDA) criteria (15). Details about the process have been published elsewhere (16, 17).
Information on stroke history was obtained from the patient and/or caregiver through structured questions. Neurological findings supporting a history of a stroke were documented after examination. Clinical stroke was defined by either symptoms (history) or signs (examination) that were indicative of stroke. In recent years, nearly all subjects have undergone computed tomography (CT) or MRI as part of their clinical evaluation. The interpretation of the neuroimaging data by the neuroradiologist was blinded to patient information other than "dementia" and was encoded in a database. A radiological infarct was defined as an area of hypodensity on brain CT scan or hyperintensity on T2-weighted brain MRI scan accompanied by hypointensity on T1-weighted images (4). White matter T2 hyperintensities without T1 changes, or dilated perivascular spaces, were not considered to be cerebral infarcts. Symptomatic infarcts were defined as having both radiological infarcts and clinical history of stroke. Silent infarcts were diagnosed in those patients showing radiological infarct without clinical history of stroke.
Between July 1991 and November 2005, 1,781 patients were diagnosed with AD, and of these, 780 patients were excluded due to absence of information about stroke history (n = 86) and/or absence of information about brain imaging (n = 728). Among the remaining 1,001 AD patients, a clinical history of stroke was present in 107 patients, and radiological infarcts in 308 patients. Sixty-eight patients with both were considered as having symptomatic infarcts.
AD patients that were included in this study were less educated (11.1 vs 11.6 yr, P = 0.02), more likely to be Hispanic (27% vs 17%, P < 0.001), more likely to have hypertension (49% vs 41%, P = 0.003), and less likely to have heart disease (11% vs 14%, P = 0.02) than the 780 excluded AD patients. There were no significant differences between the included and excluded AD patients regarding age, gender, and the proportion with diabetes mellitus.
In order to evaluate the influence of symptomatic cerebral infarcts on the cognitive performance of AD patients, selected neuropsychological tests were grouped into the following cognitive domains and converted into domain measures (16, 17). The memory domain included the total recall and delayed recall of the Selective Reminding Test and the recognition components of a multiple-choice version of the Benton Visual Retention Test. The executive function domain included phonemic fluency (a controlled oral word association test) and categorical fluency (animals and vegetables). The language domain included the total naming score for 15 selected items from the Boston Naming Test and the first 6 items from the repetition and comprehension subsets of the Boston Diagnostic Aphasia Examination. The visuospatial domain included the 5-item Rosen Drawing Test and the matching component of the multiple choice version of the Benton Visual Retention Test. The abstract reasoning domain included the age-scaled score of the revised Wechsler Adult Intelligence Scale (WAIS-R) similarities subtest and the identities and oddities subtest of the Dementia Rating Scale.
In order to define the cognitive domains, the results of each of the 12 baseline individual tests were first transformed into z-scores. Mean and standard deviations (SDs) for each test were calculated from the scores of 500 age-gender-matched subjects from the same ADRC data set who had neither dementia nor amnestic mild cognitive impairment nor non-amnestic mild cognitive impairment according to consensus at the consensus conference. There were no significant differences between AD patients and controls regarding age, gender, duration of education, ethnicity, and frequency of silent or symptomatic infarcts. Mean z-scores for each cognitive domain were calculated. Some individual test scores were missing; however, the domain measure was calculated when at least half of the individual scores were available.
We compared the demographic features of AD patients according to the presence of symptomatic cerebral infarcts using a non-parametric test for continuous variables and chi-square test for categorical variables. We evaluated the influence of symptomatic infarcts on the scores of the each cognitive domain measures using linear regression. The first linear regression analyses included symptomatic infarcts as an independent variable and cognitive domain measures as dependent variables. These were adjusted for age, sex, education, and ethnicity. After initial analysis, additional covariates were added to the model. We adjusted for diabetes mellitus, hypertension, heart disease, and the clinical dementia rating. In further regression analyses, we additionally adjusted for silent infarct, multiplicity of radiological infarcts, and location of radiological infarcts.
This study was approved by the institutional review board of the New York State Psychiatric Institute (Protocol #5467R). All subjects gave informed consent for participation in this study. This study followed Good Clinical Practice, consistent with the International Conference on Harmonization (ICH) ethical principles for medical research involving human subjects, and with full compliance with privacy principles.
By NINCDS-ADRDA criteria, there were 522 probable AD patients and 479 possible AD patients. Most of the latter were designated as possible due to the presence of concomitant vascular or psychiatric dysfunction. Severity of dementia, classified by Clinical Dementia Rating (CDR) scale, was CDR 1 in 726 patients (72.5%), CDR 2 in 206 patients (20.6%), and CDR 3 in 69 patients (6.9%). A total of 503 infarcts were detected in the following locations: frontal 34; temporal 14; parietal 28; occipital 17; thalamus 51; basal ganglia 106; white matter 161; brainstem 27; cerebellum 32, and unclassified 33. Among 308 patients with radiological infarcts, 188 patients had a single lesion and the remaining 120 patients had multiple lesions. Neuroimaging, included MRI was performed in 59.9% of patients and CT alone in 40.1% of patients. The time between brain imaging and neuropsychological evaluation was somewhat greater for CT (9.9 ± 18.9 months) compared to MRI (7.2 ± 13.7 months, P = 0.01).
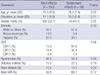
AD patients with symptomatic infarcts were older than those without (P = 0.03). Comparisons of other characteristics were not different between groups including imaging modality usage and duration between neuropsychological evaluation and neuroimaging (Table 1).
AD patients with a symptomatic infarct had poorer scores for executive function, irrespective of adjustment for age, gender, education, and ethnicity. This significance was persistent after four additional adjustments with vascular risk factors (hypertension, diabetes, and heart diseases) and CDR, silent infarct, multiple infarct, and frontal infarcts (Table 2). AD patients with a symptomatic infarct also had poorer scores in language and visuospatial performance after adjustment for age, gender, education, ethnicity, and multiple infarcts, but not in the other analyses.
Silent infarcts, multiple infarcts, and frontal infarcts had no discernible influence on any cognitive performance. Other locations of infarcts could not be added to the model due to inadequate of model fitness (variance inflation > 10).
When the analysis was limited to 962 patients by excluding those who had history of stroke without radiological infarcts, AD patients with a symptomatic infarct still had poorer scores for executive function in all models. When the analysis included only the 553 patients who had undergone MRI within one year of testing, AD patients with symptomatic infarcts still had poorer scores for executive function (β, -0.15; 95% CI: -0.60 to -0.09; P = 0.01). Only 4 patients had symptomatic infarcts among the 522 patents with probable AD and the influence of symptomatic infarcts disappeared in the separated analysis in probable AD patients.
Consistent with results from other studies of non-demented elderly (4-6, 18), symptomatic infarcts in patients with AD likewise had an additional unfavorable influence on cognition, even after considering the severity of AD. This result is consistent with described cognitive changes after symptomatic stroke in AD (19, 20). A decline in executive performance was noted regardless of the multiplicity or location of infarcts, within the limits of this study. Executive dysfunction may be related to injury to the frontal-subcortical network, or possibly related to other infarct locations (21).
We did not find a detrimental effect of silent radiological infarcts in AD patients, unlike some studies of non-demented elderly or patients with mild AD (4, 10). Usually, silent infarcts have a smaller volume and are located in non-eloquent areas compared to symptomatic infarcts; therefore, it is difficult to detect minimal changes resulting from minor infarcts, especially in severe or neocortical stage AD.
The strengths of our study included a large multiethnic referral population, separate consideration of symptomatic infarcts and silent infarcts, examination of several cognitive domains, and adjustment for multiple covariates. There are also a number of limitations to this study. First, we were unable to examine the various factors that may have influenced the associations identified, such as the timing of symptomatic infarcts, subtypes of stroke, the presence of white matter hyperintensities (22). Second, numbers of patients with severe dementia are small compared to those with mild to moderate dementia. Also, there are many fewer patients with symptomatic cerebral infarcts, than with silent infarcts, althouth this reflects actual prevalences (11). Third, we do not have validation of diagnosis of AD with autopsy findings, so there is a possibility of misdiagnosis of vascular dementia as AD. However, AD patients with symptomatic infarcts apt to be classified into possible AD regardless of burden of AD pathology. Therefore, it might be impossible to study the influence of symptomatic infarct after excluding possible AD patients. Finally, the analysis here involves data accumulated over a 16 yr (1991-2005), with accompanying difference in imaging modalities and varying time intervals between neuroimaging study and the neuropsychological evaluation. Additionally, executive function was not evaluated by the other tests for frontal-executive function (23).
Despite these potential limitations, our results support the hypothesis that symptomatic cerebral infarcts in the AD population may provide an additive "non-memory" factor contributing to dementia and the influence of cerebral infarcts is neither general nor diffuse, and the presence of clinical history may have a more important influence on executive performance in AD.
AUTHOR SUMMARY
Importance of Symptomatic Cerebral Infarcts on Cognitive Performance in Patients with Alzheimer's Disease
Soo-Jin Cho, Nikolaos Scarmeas, Tae-Won Jang, Karen Marder, Ming-Xin Tang, and Lawrence S. Honig
Both Alzheimer pathology and cerebral infarcts are common in older people. The contribution of symptomatic cerebral infarcts to cognitive impairment is uncertain in AD. We studied 1,001 clinically probable or possible AD patients. Linear regression was used to evaluate for an association between symptomatic cerebral infarcts and memory, language, executive function, abstract reasoning, and visuospatial performance, separately. Models were adjusted for covariates including age, gender, education, ethnicity, vascular risk factors, clinical dementia rating, the presence of silent cerebral infarcts, and multiplicity or location of infarcts. Adjusting for all covariates, AD patients with symptomatic infarcts (n = 68) had more impairment of executive function (P < 0.05). Silent infarcts (n = 240) had no influence on any cognitive performance. The presence of clinical history of cerebral infarct may have a more important influence on executive performance in AD.
References
1. Korczyn AD. Alzheimer's disease and vascular brain lesions. J Neurol Sci. 2005. 231:1–2.
2. Schneider JA, Arvanitakis Z, Leurgans SE, Bennett DA. The neuropathology of probable Alzheimer disease and mild cognitive impairment. Ann Neurol. 2009. 66:200–208.
3. Honig LS, Tang MX, Albert S, Costa R, Luchsinger J, Manly J, Stern Y, Mayeux R. Stroke and the risk of Alzheimer disease. Arch Neurol. 2003. 60:1707–1712.
4. Longstreth WT Jr, Bernick C, Manolio TA, Bryan N, Jungreis CA, Price TR. Cardiovascular Health Study Collaborative Research Group. Lacunar infarcts defined by magnetic resonance imaging of 3660 elderly people: the Cardiovascular Health Study. Arch Neurol. 1998. 55:1217–1225.
5. Prins ND, van Dijk EJ, den Heijer T, Vermeer SE, Jolles J, Koudstaal PJ, Hofman A, Breteler MM. Cerebral small-vessel disease and decline in information processing speed, executive function and memory. Brain. 2005. 128:2034–2041.
6. Luchsinger JA, Brickman AM, Reitz C, Cho SJ, Schupf N, Manly JJ, Tang MX, Small SA, Mayeux R, DeCarli C, Brown TR. Subclinical cerebrovascular disease in mild cognitive impairment. Neurology. 2009. 73:450–456.
7. Kalaria RN, Erkinjuntti T. Small vessel disease and subcortical vascular dementia. J Clin Neurol. 2006. 2:1–11.
8. Schmidtke K, Hüll M. Neuropsychological differentiation of small vessel disease, Alzheimer's disease and mixed dementia. J Neurol Sci. 2002. 203-204:17–22.
9. Esiri MM, Nagy Z, Smith MZ, Barnetson L, Smith AD. Cerebrovascular disease and threshold for dementia in the early stages of Alzheimer's disease. Lancet. 1999. 354:919–920.
10. Song IU, Kim JS, Kim YI, Eah KY, Lee KS. Clinical significance of silent cerebral infarctions in patients with Alzheimer disease. Cogn Behav Neurol. 2007. 20:93–98.
11. Del Ser T, Hachinski V, Merskey H, Munoz DG. Alzheimer's disease with and without cerebral infarcts. J Neurol Sci. 2005. 231:3–11.
12. Lee JH, Olichney JM, Hansen LA, Hofstetter CR, Thal LJ. Small concomitant vascular lesions do not influence rates of cognitive decline in patients with Alzheimer disease. Arch Neurol. 2000. 57:1474–1479.
13. Reed BR, Mungas DM, Kramer JH, Ellis W, Vinters HV, Zarow C, Jagust WJ, Chui HC. Profiles of neuropsychological impairment in autopsy-defined Alzheimer's disease and cerebrovascular disease. Brain. 2007. 130:731–739.
14. Jellinger KA, Attems J. Neuropathological evaluation of mixed dementia. J Neurol Sci. 2007. 257:80–87.
15. McKhann G, Drachman D, Folstein M, Katzman R, Price D, Stadlan EM. Clinical diagnosis of Alzheimer's disease: report of the NINCDS-ADRDA Work Group under the auspices of Department of Health and Human Services Task Force on Alzheimer's Disease. Neurology. 1984. 34:939–944.
16. Scarmeas N, Albert SM, Manly JJ, Stern Y. Education and rates of cognitive decline in incident Alzheimer's disease. J Neurol Neurosurg Psychiatry. 2006. 77:308–316.
17. Vliet EC, Manly J, Tang MX, Marder K, Bell K, Stern Y. The neuropsychological profiles of mild Alzheimer's disease and questionable dementia as compared to age-related cognitive decline. J Int Neuropsychol Soc. 2003. 9:720–732.
18. Schneider JA, Wilson RS, Cochran EJ, Bienias JL, Arnold SE, Evans DA, Bennett DA. Relation of cerebral infarctions to dementia and cognitive function in older persons. Neurology. 2003. 60:1082–1088.
19. Regan C, Katona C, Walker Z, Hooper J, Donovan J, Livingston G. Relationship of vascular risk to the progression of Alzheimer disease. Neurology. 2006. 67:1357–1362.
20. Kalaria RN. The role of cerebral ischemia in Alzheimer's disease. Neurobiol Aging. 2000. 21:321–330.
21. Vataja R, Pohjasvaara T, Mäntylä R, Ylikoski R, Leppävuori A, Leskelä M, Kalska H, Hietanen M, Aronen HJ, Salonen O, Kaste M, Erkinjuntti T. MRI correlates of executive dysfunction in patients with ischaemic stroke. Eur J Neurol. 2003. 10:625–631.
22. Wright CB, Festa JR, Paik MC, Schmiedigen A, Brown TR, Yoshita M, DeCarli C, Sacco R, Stern Y. White matter hyperintensities and subclinical infarction: associations with psychomotor speed and cognitive flexibility. Stroke. 2008. 39:800–805.
23. Ahn HJ, Chin J, Park A, Lee BH, Suh MK, Seo SW, Na DL. Seoul Neuropsychological Screening Battery-dementia version (SNSB-D): a useful tool for assessing and monitoring cognitive impairment in dementia patients. J Korean Med Sci. 2010. 25:1071–1076.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download