Abstract
The present study was performed to determine the incidence and predictive factors of benign renal lesions in Korean patients undergoing nephrectomy for presumed renal cell carcinoma on preoperative imaging. We analyzed the pathologic reports and medical records of 1,598 eligible patients with unilateral, nonmetastatic, and nonfamilial renal masses. Of the 1,598 renal masses, 114 (7.1%) were benign lesions, including angiomyolipoma in 47 (2.9%), oncocytoma in 23 (1.4%), and complicated cysts in 18 (1.1%) patients. On univariate analysis, the proportion of benign lesions was significantly higher in female patients, and in patients with smaller tumors, cystic renal masses, and without gross hematuria as a presenting symptom. When renal lesions were stratified by tumor size, the proportion of benign as opposed to malignant lesions decreased significantly as tumor size increased. On multivariate analysis, female gender, smaller tumor size, and cystic lesions were significantly associated with benign histological features. The findings in this large cohort of Korean patients show a lower incidence (7.1%) of benign renal lesions than those of previous Western reports. Female gender, cystic renal lesions, and smaller tumor size are independent predictors of benign histological features.
Advances in modern imaging technology and the widespread implementation of conventional imaging modalities, such as ultrasonography (USG), computed tomography (CT), and magnetic resonance imaging (MRI), have led to an increase in the detection of incidental renal neoplasms (1, 2). Consequently, the incidence of benign renal masses has increased along with the increasing incidence of renal cell carcinoma (RCC) because current imaging and biopsy techniques cannot predict the histological features of renal tumors with complete accuracy (1, 3, 4). In contemporary practice, a number of Western studies have reported a 13%-25% incidence of benign renal lesions at nephrectomy (3, 5-11), although data on Asian patients are scarce. The few studies conducted with patients in Asian countries have reported a lower incidence, 10%-11%, than that reported by Western studies (12, 13). However, these studies were limited in that the data were based on relatively small study cohorts, and most studies excluded large masses.
The objectives of this study were to determine the incidence of benign renal lesions in a large cohort of Korean patients undergoing nephrectomies for image diagnosis of RCC and to investigate the clinical predictors of benign renal tumors.
The institutional review board at our institution approved this study. A total of 2,269 patients underwent nephrectomies between January 2000 and May 2010. We excluded 451 patients whose operations were recorded as simple nephrectomy, and 220 patients with recurred renal cancer, bilateral disease, metastatic disease, or familial disease. Hence, the medical records of 1,598 eligible patients who underwent consecutive radical or partial nephrectomies for presumed RCC were retrospectively reviewed and analyzed. In the 23 patients with multiple tumors in the same kidney, the largest tumor was included in the analysis. All patients underwent preoperative contrast-enhanced CT scans, MR imaging, or both for clinical diagnosis and staging, and all lesions included in this analysis were deemed sufficiently suspicious for RCC on preoperative imaging. Since data were collected at a single tertiary referral center, many patients were transferred from primary or secondary care centers after initial CT imaging was conducted. Experienced genitourinary radiologists at our institution reviewed all imaging studies that were performed at outside hospitals. If an image was obscure or of poor quality, we performed an additional imaging study, such as CT, MRI, or contrast-enhanced renal USG. When the results of additional imaging revealed a greater chance of a benign lesion, the lesions were closely monitored in most cases. If we performed nephrectomies for such lesions, the operations were recorded as simple nephrectomies and the patients were excluded. Renal lesions were classified into the following three categories on the basis of the pathologic reports: benign lesion, RCC, or other malignancy. Cystic renal masses were classified using the Bosniak classification (14). Bosniak category III lesions were defined as indeterminate cystic masses with thickened irregular walls or septa in which enhancement could be seen, and Bosniak category IV lesions were defined as clearly malignant cystic lesions that contained enhancing soft-tissue components. Renal carcinomas were classified according to the recommendations of the 1997 American Joint Committee on Cancer report of RCC classification and the Heidelberg classification scheme (15, 16). Tumor size was determined using pathological measurements. The data were analyzed as continuous variables and as categorical variables, stratifying tumors 2 cm or smaller, 2-4 cm, 4-7 cm, or larger than 7 cm.
Statistical analyses were performed with SPSS 17.0 software (SPSS, Chicago, IL, USA). Categorical variables were compared using the chi-square or Fisher's exact test, and continuous variables were compared using the Mann-Whitney test with or without Bonferroni's correction. Logistic regression analysis was performed to identify the variables predictive of benign lesions. All P values were two-sided, and differences were considered statistically significant at P < 0.05.
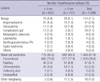
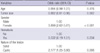
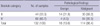
Table 1 summarizes the clinicopathological parameters that were assessed in this study. Among the 1,598 patients, 1,081 patients (67.6%) were male and 517 patients (32.4%) were female. The mean age was 54.3 yr (range, 10 to 86), and the mean tumor size was 4.8 cm (range, 0.6 to 24 cm). Of the 1,598 renal masses, 1,468 (91.9%) were RCC and 16 (1.0%) were other malignancies. Benign renal lesions were found in 114 (7.1%) patients, including angiomyolipoma (AML) in 47 (2.9%), oncocytoma in 23 (1.4%), complicated cyst in 18 (1.1%), and metanephric adenoma in 6 (0.4%) patients (Table 2). AML constituted 41.2% of all benign lesions; when a tumor was 4 cm or smaller, AML was the most common benign renal tumor, whereas oncocytoma was most prevalent if the tumor was larger than 4 cm (Table 2). The proportion of benign lesions was significantly higher in females than in males (13.5% vs 4.1%, P < 0.001). The most common presenting symptom was gross hematuria (9.4%), followed by ipsilateral flank pain (8.0%), systemic symptoms including weight loss or severe fatigue (3.4%), and palpable abdominal masses (1.3%). Gross hematuria was significantly more common in patients with malignant lesions (P = 0.026). When renal lesions were stratified according to tumor size, the incidence of benign as opposed to malignant lesions decreased significantly as tumor size increased (P = 0.004) (Table 1). In patients with renal masses 2 cm or smaller, 2-4 cm, 4-7 cm, and larger than 7.0 cm, the incidences of benign lesions were 11.7%, 7.5%, 6.1%, and 3.7%, respectively, showing a significant linear-by-linear association on Cochran-Armitage trend test (P < 0.001). Benign lesions were more common in cystic lesions than in solid lesions (13.6% vs 6.5%, P = 0.002). On multiple logistic regression analysis, female gender, smaller tumor size, and cystic renal lesions were independent predictors of benign histological features (Table 3). When 132 cystic renal lesions were classified according to their pathologic results, Bosniak category III lesions had a 31.8% chance of being benign, while Bosniak category IV lesions had only a 4.5% chance of being benign (Table 4).
To our knowledge, this study is the largest contemporary series to evaluate the incidence of benign renal lesions in Asian patients. The overall incidence of benign pathological findings in Korean patients at surgery was 7.1%, which is lower than the incidences reported in recent studies from Western countries (3, 6-11). In this respect, it has already been suggested that the low incidence of oncocytomas in Asian patients is one reason why Asian patients have a lower incidence of benign renal lesions compared to Western patients (12). In the present study, AML (2.9%) was the most common benign finding, followed by oncocytoma (1.4%), which was approximately half as common as AML. These results were consistent with the findings of two previous studies showing that oncocytoma was less frequent in Asian countries in comparison with a 6%-13% incidence in Western countries (12, 13). Notably, the overall incidence of benign lesions in our data was slightly lower than the incidence of benign lesions reported in studies from Japan and China (12, 13). These differences might be due to different inclusion criteria and additional imaging studies. We included renal masses larger than 7 cm and excluded a large number of benign cases through multimodal preoperative imaging studies. Studies have shown that patients with larger tumors have a lower incidence of benign lesions (17). In addition, when there was an obscure lesion on a CT image, we did not hesitate to perform additional imaging studies, including another round of CT, MRI, or additional contrast-enhanced renal USG, which could improve the characterization of renal tumors (18-21). Therefore, a number of benign lesions, such as AMLs or benign cystic lesions, were excluded. This may explain why we observed a lower incidence of benign lesions compared with those in other East Asian series. Many studies have demonstrated that the incidence of benign renal lesions at surgery is higher in female patients (11-13). In this respect, our data were consistent. The incidence of benign lesions in women was about four times higher than that in men (odds ratio [OR] 3.899, 95% confidence interval [CI] 2.62-5.81, P < 0.001), which could be attributed to the higher incidence of AML in women than in men (6.2% vs 1.4%, P < 0.001). Unlike the clear association with sex, however, there is controversy about the relationship between tumor size and pathological results. Studies have tended to show an inverse relationship between tumor size and the incidence of benign lesions on univariate analysis (22), although studies that excluded larger renal lesions did not show a relationship in multivariate analysis (11, 12, 23). By limiting the inclusion criteria to small lesions, the significant relationship between tumor size and pathological outcome disappeared. In contrast, studies that included all renal masses without size limitations exhibited a significant relationship between tumor size and pathological outcome (10). In this study, the incidence of benign lesions was significantly related to tumor size, similar to results reported by Frank et al. (5), who analyzed a large cohort of 2,935 tumors. Cystic renal lesions were also independently associated with the incidence of benign histological features. The incidence of benign lesions was about two times higher in cystic lesions than in solid lesions (OR 2.177, 95% CI 1.25-3.80, P = 0.006). When cystic renal lesions were classified according to Bosniak classification, 31.8% of category III lesions and 4.5% of category IV lesions were benign. The incidences of benign lesions were slightly lower than those of previous studies (24, 25). In a comprehensive literature review, Warren et al. (26) reported incidences of benign lesions in category III and IV lesions of 67% and 7.5%, respectively. However, this might also be attributed to more active implementation of additional imaging studies, such as contrast-enhanced USG, at our institution (27). Quaia et al. (28) reported that contrast-enhanced USG was better than CT for the diagnosis of malignancy in complex cystic renal masses. In addition, the differences in the definitions of Bosniak classifications among centers might influence the results. To our knowledge, our study is the first to report the incidence of benign lesions for presumed RCC in light of specific presenting symptoms. Interestingly, we found no difference between benign and malignant lesions with respect to the following presenting symptoms: ipsilateral flank pain, mass palpability, or systemic symptoms such as weight loss or severe fatigue. Although gross hematuria was more common in malignancy, the significance of this difference disappeared on multivariate analysis.
Our study had some limitations. First, its retrospective nature might have skewed our data, although we included a large cohort of patients. Second, as a single-center study, there may be undetected regional and demographic trends that might have influenced the types of patients who came to our institution. Third, we used the final pathological tumor diameter instead of the radiological tumor diameter. A study conducted by Schlomer et al. (29) reported that preoperative CT imaging may slightly overestimate the pathological sizes of renal tumors with diameters of 1-5 cm. Therefore, to determine the clinical predictors of benign lesions, tumor sizes measured through imaging studies would be more reasonable. However, it is also well known that, for renal tumors, clinical size and pathological size are highly correlated with each other (30). In addition, more than one half of all of the study patients were transferred to our institution after CT or MR imaging was performed at a previous institution. Consequently, there were differences in imaging protocols that might have caused differences in measurements. Furthermore, a considerable time gap intervened between CT scanning and nephrectomy, during which time tumor growth might have occurred. For this reason, it was difficult to use radiological tumor sizes in this study. Finally, the number of partial nephrectomies was significantly higher for benign lesions. However, the reason seems to be that benign lesions were smaller. Despite these limitations, the results of this study may provide valuable information for clinicians counseling patients with renal lesions and may help clinicians decide the most appropriate therapeutic modality, including renal biopsies and close monitoring.
In conclusion, a large cohort from a single institution in Korea showed a lower incidence (7.1%) of benign renal lesions than those found in Western studies. The most common benign lesion was AML, which accounted for 41.2% of all benign lesions. When a tumor was 4 cm or smaller, AML was the most common benign renal tumor, while oncocytoma was the most prevalent when the tumor was larger than 4 cm. Female gender, cystic renal lesions, and smaller tumor size were independently associated with the incidence of benign histological features.
Figures and Tables
AUTHOR SUMMARY
Incidence and Predictive Factors of Benign Renal Lesions in Korean Patients with Preoperative Imaging Diagnoses of Renal Cell Carcinoma
Seo Yong Park, Seong Soo Jeon, Seo Yeon Lee, Byong Chang Jeong, Seong Il Seo, Hyun Moo Lee, and Han Yong Choi
The incidence of benign renal masses has increased along with the increasing incidence of renal cell carcinoma because current imaging and biopsy techniques cannot predict the histological features of renal tumors with complete accuracy. In contemporary practice, a number of Western studies have reported a 13%-25% incidence of benign renal lesions at nephrectomy, although data on Asian patients are scarce. Hence, the present study was performed to determine the incidence and predictive factors of benign renal lesions in Korean patients undergoing nephrectomy for presumed renal cell carcinoma on preoperative imaging. The overall incidence of benign pathological findings in Korean patients at surgery was 7.1%, which is lower than the incidences reported in recent studies from Western countries. Female gender, smaller tumor size, and cystic lesions were significantly associated with benign histological features.
References
1. Hollingsworth JM, Miller DC, Daignault S, Hollenbeck BK. Rising incidence of small renal masses: a need to reassess treatment effect. J Natl Cancer Inst. 2006. 98:1331–1334.
2. Volpe A, Panzarella T, Rendon RA, Haider MA, Kondylis FI, Jewett MA. The natural history of incidentally detected small renal masses. Cancer. 2004. 100:738–745.
3. Murphy AM, Buck AM, Benson MC, McKiernan JM. Increasing detection rate of benign renal tumors: evaluation of factors predicting for benign tumor histologic features during past two decades. Urology. 2009. 73:1293–1297.
4. Silverman SG, Gan YU, Mortele KJ, Tuncali K, Cibas ES. Renal masses in the adult patient: the role of percutaneous biopsy. Radiology. 2006. 240:6–22.
5. Frank I, Blute ML, Cheville JC, Lohse CM, Weaver AL, Zincke H. Solid renal tumors: an analysis of pathological features related to tumor size. J Urol. 2003. 170:2217–2220.
6. Kutikov A, Fossett LK, Ramchandani P, Tomaszewski JE, Siegelman ES, Banner MP, Van Arsdalen KN, Wein AJ, Malkowicz SB. Incidence of benign pathologic findings at partial nephrectomy for solitary renal mass presumed to be renal cell carcinoma on preoperative imaging. Urology. 2006. 68:737–740.
7. Lane BR, Babineau D, Kattan MW, Novick AC, Gill IS, Zhou M, Weight CJ, Campbell SC. A preoperative prognostic nomogram for solid enhancing renal tumors 7 cm or less amenable to partial nephrectomy. J Urol. 2007. 178:429–434.
8. McKiernan J, Yossepowitch O, Kattan MW, Simmons R, Motzer RJ, Reuter VE, Russo P. Partial nephrectomy for renal cortical tumors: pathologic findings and impact on outcome. Urology. 2002. 60:1003–1009.
9. Pahernik S, Roos F, Hampel C, Gillitzer R, Melchior SW, Thüroff JW. Nephron sparing surgery for renal cell carcinoma with normal contralateral kidney: 25 years of experience. J Urol. 2006. 175:2027–2031.
10. Schlomer B, Figenshau RS, Yan Y, Venkatesh R, Bhayani SB. Pathological features of renal neoplasms classified by size and symptomatology. J Urol. 2006. 176:1317–1320.
11. Snyder ME, Bach A, Kattan MW, Raj GV, Reuter VE, Russo P. Incidence of benign lesions for clinically localized renal masses smaller than 7 cm in radiological diameter: influence of sex. J Urol. 2006. 176:2391–2395.
12. Fujii Y, Komai Y, Saito K, Iimura Y, Yonese J, Kawakami S, Ishikawa Y, Kumagai J, Kihara K, Fukui I. Incidence of benign pathologic lesions at partial nephrectomy for presumed RCC renal masses: Japanese dual-center experience with 176 consecutive patients. Urology. 2008. 72:598–602.
13. Xiong YH, Zhang ZL, Li YH, Liu ZW, Hou GL, Liu Q, Yun JP, Zhang XQ, Zhou FJ. Benign pathological findings in 303 Chinese patients undergoing surgery for presumed localized renal cell carcinoma. Int J Urol. 2010. 17:517–521.
14. Bosniak MA. Diagnosis and management of patients with complicated cystic lesions of the kidney. AJR Am J Roentgenol. 1997. 169:819–821.
15. Kovacs G, Akhtar M, Beckwith BJ, Bugert P, Cooper CS, Delahunt B, Eble JN, Fleming S, Ljungberg B, Medeiros LJ, Moch H, Reuter VE, Ritz E, Roos G, Schmidt D, Srigley JR, Storkel S, van den Berg E, Zbar B. The Heidelberg classification of renal cell tumours. J Pathol. 1997. 183:131–133.
16. Störkel S, Eble JN, Adlakha K, Amin M, Blute ML, Bostwick DG, Darson M, Delahunt B, Iczkowski K. Classification of renal cell carcinoma: Workgroup No 1 Union Internationale Contre le Cancer (UICC) and the American Joint Committee on Cancer (AJCC). Cancer. 1997. 80:987–989.
17. Schachter LR, Cookson MS, Chang SS, Smith JA Jr, Dietrich MS, Jayaram G, Herrell SD. Second prize: frequency of benign renal cortical tumors and histologic subtypes based on size in a contemporary series: what to tell our patients. J Endourol. 2007. 21:819–823.
18. Hélénon O, André M, Correas JM, Khairoune A, Merran S, Balleyguier C. Characterization of renal masses. J Radiol. 2002. 83:787–804.
19. Pallwein L, Mitterberger M, Aigner F, Pinggera GM, Gradl J, Klauser A, Halpern EJ, Strasser H, Bartsch G, Frauscher F. Small renal masses: the value of contrast-enhanced colour Doppler imaging. BJU Int. 2007. 99:579–585.
20. Roy C, Gengler L, Sauer B, Lang H. Role of contrast enhanced US in the evaluation of renal tumors. J Radiol. 2008. 89:1735–1744.
21. Tello R, Davison BD, O'Malley M, Fenlon H, Thomson KR, Witte DJ, Harewood L. MR imaging of renal masses interpreted on CT to be suspicious. AJR Am J Roentgenol. 2000. 174:1017–1022.
22. Kim SI, Choi YD, Kim SJ, Chung BH, Seong do H, Kim CI, Cheon SH, Cho JS, Song YS, Kim YS, Cho IR, Lee DH, Song KH, Kim HS, Lee JS, Yang WJ, Hong SJ. A multi-institutional study on histopathological characteristics of surgically treated renal tumors: the importance of tumor size. Yonsei Med J. 2008. 49:639–646.
23. Jeon HG, Lee SR, Kim KH, Oh YT, Cho NH, Rha KH, Yang SC, Han WK. Benign lesions after partial nephrectomy for presumed renal cell carcinoma in masses 4 cm or less: prevalence and predictors in Korean patients. Urology. 2010. 76:574–579.
24. Lang EK, Macchia RJ, Gayle B, Richter F, Watson RA, Thomas R, Myers L. CT-guided biopsy of indeterminate renal cystic masses (Bosniak 3 and 2F): accuracy and impact on clinical management. Eur Radiol. 2002. 12:2518–2524.
25. Marszalek M, Ponholzer A, Brössner C, Wachter J, Maier U, Madersbacher S. Elective open nephron-sparing surgery for renal masses: single-center experience with 129 consecutive patients. Urology. 2004. 64:38–42.
26. Warren KS, McFarlane J. The Bosniak classification of renal cystic masses. BJU Int. 2005. 95:939–942.
27. Ascenti G, Mazziotti S, Zimbaro G, Settineri N, Magno C, Melloni D, Caruso R, Scribano E. Complex cystic renal masses: characterization with contrast-enhanced US. Radiology. 2007. 243:158–165.
28. Quaia E, Bertolotto M, Cioffi V, Rossi A, Baratella E, Pizzolato R, Cov MA. Comparison of contrast-enhanced sonography with unenhanced sonography and contrast-enhanced CT in the diagnosis of malignancy in complex cystic renal masses. AJR Am J Roentgenol. 2008. 191:1239–1249.
29. Schlomer B, Figenshau RS, Yan Y, Bhayani SB. How does the radiographic size of a renal mass compare with the pathologic size? Urology. 2006. 68:292–295.
30. Yaycioglu O, Rutman MP, Balasubramaniam M, Peters KM, Gonzalez JA. Clinical and pathologic tumor size in renal cell carcinoma; difference, correlation, and analysis of the influencing factors. Urology. 2002. 60:33–38.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download