Abstract
The objective of the study was to document practice pattern of gastroenterologists for the management of gastroesophageal reflux disease (GERD) under the minimal influence of the insurance reimbursement guideline. Data on management for 1,197 consecutive patients with typical GERD symptoms were prospectively collected during 16 weeks. In order to minimize the influence of reimbursement guideline on the use of proton pump inhibitors (PPIs), rabeprazole was used for the PPI treatment. A total of 861 patients (72%) underwent endoscopy before the start of treatment. PPIs were most commonly prescribed (87%). At the start of treatment, rabeprazole 20 mg daily was prescribed to 94% of the patients who received PPI treatment and 10 mg daily to the remaining 6%. At the third visits, rabeprazole 20 mg daily was prescribed to 70% of those who were followed and 10 mg daily for the remaining 30%. Continuous PPI treatment during the 16-week period was performed in 63% of the study patients. In conclusion, a full-dose PPI is preferred for the initial and maintenance treatment of GERD under the minimal influence of the insurance reimbursement guideline, which may reflect a high proportion of GERD patients requiring a long-term treatment of a full-dose PPI.
Gastroesophageal reflux disease (GERD) is a common gastrointestinal disease in Asia as well as in the West (1, 2). Studies have reported that 10%-20% of the adult Western population experience typical GERD symptoms (heartburn and/or regurgitation) at least once per week (1). The prevalence of GERD in adult Koreans is reported to be 3.5%-8.5% (3-5). The prevalence of GERD appears to be increasing in Korea. This increase has been possibly attributed to changes in diet, an increasing aged population, the increasing frequency of endoscopic examinations, and the widely spreading knowledge on GERD.
The Montreal definition describes GERD as a condition that develops when the reflux of gastric contents causes troublesome symptoms and/or complications (6). A number of regional and international guidelines and recommendations for the management of GERD have been published. The Genval workshop report on reflux disease management, published in 1999 (7), and the Asia-Pacific consensus on the management of GERD, published in 2008 (8), are considered to be useful references for the management of GERD. Previous studies show that proton pump inhibitors (PPIs) are the most effective drug for patients with GERD (7, 8). Actually, PPIs are known to be most commonly prescribed for the treatment of GERD. However, the prescription pattern of PPIs in patients with GERD may be different between countries, which is partly attributed to the economic situation or the health insurance system. In Korea, national health insurance covers the cost for the medication prescribed in hospitals and clinics according to the insurance reimbursement guideline. Accordingly, the prescription pattern of PPIs used for the treatment of GERD is substantially influenced by the insurance reimbursement guideline.
Thus, the aim of this study was to document practice pattern of gastroenterologists for the management of GERD patients under the minimal influence of the insurance reimbursement guideline.
This study was a multicenter prospective observational study conducted in Korea. Fifty-six gastroenterologists at 51 secondary and tertiary care hospitals representing most regions of Korea participated in the study. We chose the hospitals in the consideration of the population living in that region. Fig. 1 shows the distribution of those hospitals. All participating gastroenterologists were required to recruit about 20 consecutive eligible patients who complained of typical GERD symptoms (heartburn and/or regurgitation). Patients were eligible for inclusion in this study if they were aged ≥ 18 yr and had typical GERD symptoms (heartburn and/or regurgitation) at least once per week over the previous 7 days with or without esophagitis. Endoscopy and 24-hr esophageal pH monitoring were not essential for inclusion. Patients were excluded from participation if they had taking PPIs or histamine 2 receptor blocking agents within the previous 4 weeks. The other exclusions were hypersensitivity to the active ingredient of PPIs and the presence of organic diseases such as gastrointestinal cancer, severe liver disease, pancreatic disease, peptic ulcer, inflammatory bowel disease, severe renal impairment, or severe respiratory disease.
This study was observational and descriptive in nature. Thus, we tried to reduce the influence of the study on the routine clinical practice for enrolled patients. The only thing that was affected by the study protocol was to choose a PPI. In order to minimize the influence of the insurance reimbursement guideline on the use of PPIs, we recommended the use of rabeprazole (Pariet, Janssen Korea Ltd., Seoul, Korea) for patients in whom PPI treatment should be considered for the management of GERD symptoms, because rabeprazole is the only PPI of which both full-dose and half-dose are permitted for the initial and maintenance treatment of GERD, irrespective of the presence of erosive esophagitis, in the national insurance reimbursement guideline. The others associated with the treatment for patients enrolled in the study had not been set by the study protocol. Participating gastroenterologists were asked to carry out their routine practice at their own decision. The maximum observation period for the study was 16 weeks. During the study period, gastroenterologists followed their usual practice of patient care; the severity of symptoms and medications prescribed were recorded at each visit, using a web-based electronic data capture system. At the visit for inclusion, demographic data and information on the patient's symptoms, previous investigations for GERD, and treatment received were documented. In addition, the frequency (days/week) and severity (0, none; 1, mild; 2, moderate; 3, severe) of symptoms over the previous 7 days were assessed. When esophagogastroduodenoscopy (EGD) or 24-hr esophageal pH monitoring had been performed for the evaluation of GERD symptoms, its results were reviewed.
Since this study was not a clinical trial, there was no hypothesis for the determination of the adequate sample size. Nonetheless, a sample size of 1,120 patients (20 patients per a gastroenterologist) was planned. A subgroup analysis was carried out using the chi-squared test and Student's t-test. The statistical analysis was performed using SPSS for Windows version 11 (SPSS Inc., Chicago, IL, USA).
The study was approved by each of the institutional review boards of the hospitals where the principal investigator (approval number: 4-2008-0201) and other investigators belonged. Each patient received information on the study design such as data handling and aims of the study. Informed consent was obtained. This study was an observational study and designed to have as little impact as possible on the management of patients.
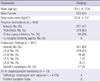
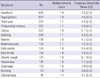
Fifty-six gastroenterologists at 32 secondary and 19 tertiary care hospitals participated in the study. A total of 1,197 patients (523 males, 44%) of mean age 53.1 ( ± 13.6) yr were recruited. Fifty-seven percent of them were enrolled at secondary care hospitals and the others (43%) at tertiary care hospitals. At the time of enrollment, 479 patients (40%) had previous EGD results and 382 patients (32%) underwent EGD before the start of medications. Thirty-six percent of those who had EGD results showed erosive esophagitis, and 3% had Barrett's esophagus. At the time of enrollment, 6 patients had previous results of 24-hr esophageal pH monitoring. Seven patients underwent 24-hr esophageal pH monitoring during the evaluation period before the start of medications, all of whom had atypical GERD symptoms and history of previous treatment for GERD symptoms. Baseline data and symptoms on patients enrolled in the study are shown in Table 1 and 2, respectively. The most common accompanying symptom was chest pain, followed by postprandial fullness, globus, belching, nausea, abdominal pain, early satiety, sore throat, chronic cough, hoarseness, dysphagia, vomiting, and odynophagia in the order of prevalence.
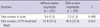
During the 16-week study period, the mean total number of visits per patient was 3.4 ( ± 1.4, ranged 1-6). PPIs were prescribed in 1,037 patients (87% of the study patients). Fig. 2 shows the total duration of PPI treatment in study subjects. The total duration of PPI treatment during the study period was ≤ 2 weeks in 2%, > 2 weeks and ≤ 4 weeks in 9%, > 4 weeks and ≤ 8 weeks in 10%, > 8 weeks and ≤ 12 weeks in 5%, and > 12 weeks and ≤ 16 weeks in 74%. A total of 748 patients were followed at week 16. The total number of visits and the total duration of PPI treatment did not significantly differ between patients with and without erosive esophagitis (Table 3). At the start of treatment, gastroenterologists prescribed rabeprazole 20 mg (full-dose) daily to 94% of the patients who received PPI treatment and rabeprazole 10 mg (half-dose) daily to the remaining 6%. At the second visits, rabeprazole 20 mg daily was prescribed to 89% of those who were followed, and 10 mg daily to the remainder. At the third visit, the participating gastroenterologists prescribed rabeprazole 20 mg daily to 70% of those who were followed and 10 mg daily for the remaining 30%. During PPI treatment, prokinetics, mucosal protectives, antacids and histamine 2 receptor blocking agents were concomitantly used in 31%, 5%, 4%, and 1% of the patients, respectively.
Several international guidelines for the management of GERD are reported (6-8), but no domestic guidelines on clinical practice for patients with GERD have been issued yet in Korea. In the present study, we followed patients with typical GERD symptoms for 16 weeks, and observed gastroenterologists' treatment patterns. The current study showed that PPIs are prescribed for the majority of patients with typical GERD symptoms and that Korean gastroenterologists preferred a full-dose PPI for both initial and maintenance treatment of GERD, irrespective of the presence of erosive esophagitis, rather than a half-dose PPI. This prospective observational study was conducted at secondary or tertiary care hospitals. Primary care clinics were excluded, because the aim of the study was to document gastroenterologists' treatment patterns. Patients with typical GERD symptoms who visit secondary and tertiary care hospitals participating in the study are treated by gastroenterologists. The institutions involved were selected on a nationwide scale in consideration of the number of regional population. Patients with typical GERD symptoms were recruited consecutively to reduce bias. EGD is relatively cheap in Korea because its cost is covered by national medical insurance. EGD was available in all institutions participating in the present study. Seventy-two percent of patients enrolled in the study had the results of EGD. Erosive esophagitis was observed in 36% of them, the majority of which was of grade LA-A or LA-B. Longitudinal studies conducted in Asia show an increase in the prevalence of GERD symptoms and reflux esophagitis (9-11). The ratio of erosive reflux disease (ERD) to nonerosive reflux disease (NERD) in Asia is believed to be lower than in the West (12). The ratio of ERD found in the present study was 36%, which seems to be getting comparable to that reported in the West. This may be partly attributed to the fact that the participating institutions were secondary and tertiary care hospitals.
Since studies on the sensitivity and specificity of heartburn for predicting the presence of GERD are lacking in Korea, it is uncertain whether heartburn is a definite marker of GERD in the Korean population. Erosive esophagitis found in patients with heartburn suggests that heartburn results from gastroesophageal reflux. Heartburn in patients without erosive esophagitis is considered to be NERD or functional heartburn. Functional heartburn is believed to be a different entity from NERD, particularly in terms of acid reflux patterns and the responsiveness to PPIs (13). Functional heartburn can be diagnosed when there are no abnormal acid or nonacid esophageal reflux, no symptom correlation with reflux, and no response to PPIs (14). Abnormal acid or nonacid reflux can be determined using a 24-hr esophageal pH/impedance monitoring. Esophageal pH monitoring was available in 28 institutions (55% of the participating institutions). However, only 1% of the study patients underwent 24-hr ambulatory esophageal pH monitoring, which suggests that this test is not commonly performed even at secondary and tertiary care hospitals. In general, PPI trial is recommended to be preceding esophageal pH monitoring, particularly in patients with typical GERD symptoms. In the present study, ambulatory esophageal pH monitoring was performed mainly in patients with atypical GERD symptoms and history of previous PPI treatment for GERD symptoms, which is in keeping with the current guidelines.
The Asian-Pacific experts for GERD reported a general consensus that PPIs provide the most effective treatment for ERD and NERD (8). The consensus is based on previous studies showing that PPIs are superior to histamine 2 receptor blocking agents in terms of healing esophageal mucosa and relieving heartburn symptoms in patients with GERD (15-17). In the present study, most of patients enrolled in the study received PPI treatment (87% of the study patients). Prokinetics were the most commonly used concomitant medications, which can be possibly supported by the positive value of prokinetics in the treatment of GERD (18, 19) and substantial overlap between GERD symptoms and dyspepsia (5, 20). Our findings of the present study that 27% and 15% of the patients with typical GERD symptoms had postprandial fullness and early satiety, respectively, demonstrate overlap between GERD symptoms and dyspepsia.
The Asian-Pacific consensus includes statements on the duration of PPI treatment for ERD and NERD as follows; "NERD patients require more than 4 weeks of initial continuous PPI therapy and ERD patients need a minimum of 4-8 weeks of initial continuous PPI therapy" (8). It is difficult to determine timing to change initial treatment to maintenance treatment. According to the guidelines, maintenance treatment usually begins after 4 weeks of initial treatment in NERD patients and after 8 weeks of initial treatment in patients with ERD. The influence of national health insurance system on the use of drugs is too big in Korea, because it covers all patients visiting hospitals due to GERD symptoms. Based on the national health insurance reimbursement guideline, full-dose of most PPIs, except rabeprazole, is permitted only for the initial treatment of ERD, but not for the initial treatment of NERD and the maintenance treatment of ERD and NERD. According to that guideline, only half-dose PPI can be used for the initial treatment in patients with GERD symptoms who have no endoscopic findings and in NERD patients, and for the maintenance treatment of GERD. Thus, practice pattern is prone to be distorted by the reimbursement guideline. Rabeprazole is the only PPI of which both full-dose and half-dose are permitted for the initial and maintenance treatment of ERD and NERD under the Korean health insurance system. So, in order to reduce distortion or variability in the clinical practice for GERD patients due to the national health insurance reimbursement guideline, we made a decision to recommend rabeprazole when PPI treatment is required for the enrolled patients. Since our main aims were to investigate the prescription pattern on the dosage of PPIs used for the treatment of GERD and to know whether Korean gastroenterologists keep the international guideline for the treatment of GERD, we tried to reduce the influence of the national health insurance reimbursement guideline and the study protocol. Thus, treatment for patients enrolled in the study had not been set by the study protocol, and participating gastroenterologists carried out their practice at their own decision.
Given that rabeprazole 20 mg daily was used as initial treatment in 94% of the patients who received PPI treatment, the majority of Korean gastroenterologists appear to prefer a full-dose PPI for the initial treatment of GERD, irrespective of the presence of erosive esophagitis. Gastroenterologists participating in this study tended to use a full-dose PPI without step-down of the dose. These points are not in keeping with the insurance reimbursement criteria, which might be attributed to a high proportion of GERD patients requiring a long-term treatment of a fulldose PPI. In the present study, the mean duration of continuous PPI therapy during the 16-week observational period was 96 and 95 days in patients with and without erosive esophagitis, respectively. In the present study, 62% of the study patients were continuously treated with PPIs until the end of the study period. Participating gastroenterologists were allowed to prescribe only rabeprazole, either 10 mg or 20 mg, if they want to use PPI. Rabeprazole is the only PPI that both dosages are permitted to be used in the maintenance therapy according to the reimbursement guideline. Accordingly, they appear to choose the PPI dosage mainly based on the treatment efficacy. If other PPIs would have selected for this study, they might have prescribed according to the reimbursement guideline, irrespective of the treatment efficacy. One of our aims was to investigate drug compliance, but we found that drug compliance was impossible to investigate, because many patients were not followed during the study period. Since this was an observational study, follow-up was not controlled by the study protocol. So, follow-up loss was not prevented, and drug compliance could not be investigated. According to the study design, participating gastroenterologists were able to make a decision for tests and treatment for the enrolled patients at their discretion. Thus, our findings suggest that many Korean patients with typical GERD symptoms need a long-term treatment of a full-dose PPI.
In conclusion, endoscopy is commonly performed for the evaluation of GERD symptoms, but 24-hr esophageal pH monitoring is not. A full-dose PPI is preferred for the initial and maintenance treatment of GERD under the minimal influence of the insurance reimbursement guideline, which may reflect a high proportion of GERD patients requiring a long-term treatment of a full-dose PPI. The management guideline appropriate for Korean patients with GERD is required.
Figures and Tables
ACKNOWLEDGMENTS
We thank the following investigators who participated in the study: Dr. Kang MK (Andong Seongso Hospital); Kang SB (Daejeon Seongmo Hospital); Ko KH (Bundang Cha Hospital); Kwon JH (Masan Medical Center); Kim NH (Ilsan Paik Hospital); Kim DY (Bumin Hospital); Kim SS (Uijeongbu St. Mary's Hospital); Kim SH (Chonbuk National University Hospital); Kim YH (Yeongkwang Hospital); Kim YK (Gachon University Gil Hospital); Kim JW (Wonju Christian Hospital); Kim JH (Hallym University Medical Center); Kim CH (Busan Paik Hospital); Kim TN (Yeungnam Medical Center); Kim TO (Pusan National University Hospital); Min HJ (Gyeongsang National University Hospital); Park KH (Mizmedi Hospital); Park SG (Maryknoll hospital); Park JH (Kangbuk Samsung Hospital); Baik CR (St. Vincent's Hospital); Sung JK (Chungnam National University Hospital); Song KA (Pusan National University Hospital); Song HJ (Asan Medical Center); Oh JC (Cheondan Hospital); Oh HJ (Daerim St. Mary's Hospital); Yoon BK (Hanmaeum Hospital); Yoon YH (Gangnam Severance Hospital); Yoon HS (Mizmedi Hospital); Lee KS (Sun Hospital); Lee SM (Pusan National University Hospital); Lee SK (Myongj St. Mary's Hospital); Lee CK (Soonchunhyang University Hospital); Lee HR (Hanyang University Hospital); Jang BI (Yeungnam Medical Center); Cheon YC (Hanyang Kuri University Hospital); Cho YC (Tongyeong Red Cross Hospital); Cho YS (Ilsan Hospital); Ji JS (Incheon St. Mary's Hospital); Choi KD (Asan Medical Center); Choi ST (Pohang St. Mary's Hospital); Choi SH (Busan St. Mary's Hospital); Ha CY (Gyeongsang National University Hospital); Hong KY (Kwangju Christian Hospital).
AUTHOR SUMMARY
Practice Pattern of Gastroenterologists for the Management of GERD Under the Minimal Influence of the Insurance Reimbursement Guideline: A Multicenter Prospective Observational Study
Kwang Jae Lee, Jin Il Kim, Ju Sang Park, Byung Sik Moon, Sang-Gyun Kim, Jae Hee Chun, Hoon-Yong Jung, Chang Hwan Choi, Seong Woo Chun, Geun Am Song, Myung Gyu Choi and Hoon Jai Chun
We studied practice pattern of gastroenterologists for the management of GERD under the minimal influence of the insurance reimbursement guideline in Korea. A full-dose proton pump inhibitor (PPI) is preferred for the initial and maintenance treatment of GERD, which may reflect a high proportion of GERD patients requiring a long-term treatment of a full-dose PPI.
References
1. Dent J, El-Serag HB, Wallander MA, Johansson S. Epidemiology of gastro-esophageal reflux disease: a systematic review. Gut. 2005. 54:710–717.
2. Wong BC, Kinoshita Y. Systematic review on epidemiology of gastroesophageal reflux disease in Asia. Clin Gastroenterol Hepatol. 2006. 4:398–407.
3. Yang SY, Lee OY, Bak YT, Jun DW, Lee SP, Lee SH, Park GT, Yoon BC, Choi HS, Hahm JS, Lee MH, Lee DH. Prevalence of gastroesophageal reflux disease symptoms and uninvestigated dyspepsia in Korea: a population-based study. Dig Dis Sci. 2008. 53:188–193.
4. Cho YS, Choi MG, Jeong JJ, Chung WC, Lee IS, Kim SW, Han SW, Choi KY, Chung IS. Prevalence and clinical spectrum of gastroesophageal reflux: a population-based study in Asan-si, Korea. Am J Gastroenterol. 2005. 100:747–753.
5. Lee SY, Lee KJ, Kim SJ, Cho SW. Prevalence and risk factors for overlaps between gastroesophageal reflux disease, dyspepsia, and irritable bowel syndrome: a population-based study. Digestion. 2009. 79:196–201.
6. Vakil N, van Zanten SV, Kahrilas P, Dent J, Jones R. Global Consensus Group. The Montreal definition and classification of gastroesophageal reflux disease: a global evidence-based consensus. Am J Gastroenterol. 2006. 101:1900–1920.
7. Dent J, Brun J, Fendrick AM, Fennerty MB, Janssens J, Kahrilas P, Lauritsen K, Reynolds JC, Shaw M, Talley N. An evidence-based appraisal of reflux disease management: the Genval Workshop Report. Gut. 1998. 44:S1–S16.
8. Fock KM, Talley NJ, Fass R, Goh KL, Katelaris P, Hunt R, Hongo M, Ang TL, Holtmann G, Nandurkar S, Lin SR, Wong BC, Chan FK, Rani AA, Bak YT, Sollano J, Ho KY, Manatsathit S. Asia-Pacific consensus on the management of gastroesophageal reflux disease: update. J Gastroenterol Hepatol. 2008. 23:8–22.
9. Lim SL, Goh WT, Lee JM, Ng TP, Ho KY. Community Medicine GI Study Group. Changing prevalence of gastroesophageal reflux with changing time: longitudinal study in an Asian population. J Gastroenterol Hepatol. 2005. 20:995–1001.
10. Ho KY, Chan YH, Kang JY. Increasing trend of reflux esophagitis and decreasing trend of Helicobacter pylori infection in patients from a multiethnic Asian country. Am J Gastroenterol. 2005. 100:1923–1928.
11. Sollano JD, Wong SN, Andal-Gamutan T, Chan MM, Carpio RE, Tady CS, Ismael AE, Judan-Ruiz EA, Ang VN, Go JT, Lim VY, Perez JY, Alvarez SZ. Erosive esophagitis in the Philippines: a comparison between two time periods. J Gastroenterol Hepatol. 2007. 22:1650–1655.
12. Ha NR, Lee HL, Lee OY, Yoon BC, Choi HS, Hahm JS, Ahn YH, Koh DH. Differences in clinical characteristics between patients with non-erosive reflux disease and erosive esophagitis in Korea. J Korean Med Sci. 2010. 25:1318–1322.
13. Lee KJ, Kwon HC, Cheong JY, Cho SW. Demographic, clinical, and psychological characteristics of the heartburn groups classified using the Rome III criteria and factors associated with the responsiveness to proton pump inhibitors in the gastroesophageal reflux disease group. Digestion. 2009. 79:131–136.
14. Galmiche JP, Clouse RE, Bálint A, Cook IJ, Kahrilas PJ, Paterson WG, Smout AJ. Functional esophageal disorders. Gastroenterology. 2006. 130:1459–1465.
15. Caro JJ, Salas M, Ward A. Healing and relapse rates in gastroesophageal reflux disease treated with the newer proton-pump inhibitors lansoprazole, rabeprazole, and pantoprazole compared with omeprazole, ranitidine, and placebo: evidence from randomized clinical trials. Clin Ther. 2001. 23:998–1017.
16. Richter JE, Campbell DR, Kahrilas PJ, Huang B, Fludas C. Lansoprazole compared with ranitidine for the treatment of nonerosive gastroesophageal reflux disease. Arch Intern Med. 2000. 160:1803–1809.
17. Fujiwara Y, Higuchi K, Nebiki H, Chono S, Uno H, Kitada K, Satoh H, Nakagawa K, Kobayashi K, Tominaga K, Watanabe T, Oshitani N, Arakawa T. Famotidine vs. omeprazole: a prospective randomized multicentre trial to determine efficacy in non-erosive gastro-oesophageal reflux disease. Aliment Pharmacol Ther. 2005. 21:10–18.
18. Kim YS, Kim TH, Choi CS, Shon YW, Kim SW, Seo GS, Nah YH, Choi MG, Choi SC. Effect of itopride, a new prokinetic, in patients with mild GERD: a pilot study. World J Gastroenterol. 2005. 11:4210–4214.
19. Madan K, Ahuja V, Kashyap PC, Sharma MP. Comparison of efficacy of pantoprazole alone versus pantoprazole plus mosapride in therapy of gastroesophageal reflux disease: a randomized trial. Dis Esophagus. 2004. 17:274–278.
20. Kaji M, Fujiwara Y, Shiba M, Kohata Y, Yamagami H, Tanigawa T, Watanabe K, Watanabe T, Tominaga K, Arakawa T. Prevalence of overlaps between GERD, FD and IBS and impact on health-related quality of life. J Gastroenterol Hepatol. 2010. 25:1151–1156.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download