Abstract
Many predictive models have been proposed for better stratification of diffuse large B-cell lymphoma (DLBCL). Hans' algorithm has been widely used as standard to sub-classify DLBCL into germinal center B-cell (GCB) and non-GCB origins. However, there have been disagreements in the literature regarding its prognostic significance. Here, we retrospectively analyzed Hans' algorithm and the individual immunohistochemical biomarkers at different cut-off values (5%, 30%, 50% or 75%) in 94 Korean patients with DLBCL treated with combination chemotherapy with cyclophosphamide, daunorubicin, vincristine, and prednisone. No significant differences were observed between the GCB (18 patients, 19.1%) and non-GCB (76, 80.9%) groups. Among individual biomarkers, CD10 negativity (cut point: 30%) and bcl-6 positivity (cut point: 5%) were independent good prognostic markers in progression-free survival (PFS), whereas bcl-6 (cut point: 5%) positivity was an independent good prognostic marker in overall survival irrelevant of international prognostic index. The present study showed the lack of predictability of Hans' algorithm in DLBCL patients, and that CD10, Bcl-6 may have diverse prognostic significance at different cut-off values. Our results suggest that the proposed cut-off value may not be applied universally, and that the optimal cut-off value may need to be optimized for individual laboratory.
Diffuse large B cell lymphoma (DLBCL) is the most common type of non-Hodgkin's lymphoma (1, 2). Although DLBCL is considered as a specific category, the variable clinical outcomes, morphologic and genetic alterations reflect that these lymphomas are heterogeneous groups of tumor rather than single clinicopathologic entity (3). For prediction of the response of chemotherapy and patient's survival, international prognostic index (IPI) is widely used. The IPI includes 5 clinical parameters and its efficacy is relatively excellent (4). But it does not represent the biologic or genetic feature of the tumor.
Recent subjects dealing with DLBCL heterogeneity have studied with genetic diversity and molecular alteration of this tumor. Particular attention has been focused on the relationship between B cell differentiation stage and the prognosis of DLBCL (3, 5). Gene expression profiling using cDNA microarray identified two distinct molecular subgroups with germinal center Bcell-like (GCB) and non-germinal center B-cell-like (non-GCB). The GCB group has more favorable outcome than non-GCB group (6, 7). Although this analysis provided critical information about the molecular heterogeneity of DLBCL, it is not routinely used in clinical practice because of high cost and the necessity of fresh frozen samples for analysis. For that reason, the identification methods using immunohistochemistry of paraffin-embedded tissue were developed by several groups (3, 5, 8). Most of these methods use CD 10 or bcl-6 as GCB markers and MUM1 or CD138 as non-GCB markers. Among these studies, Hans' method has been widely accepted as the standard in discriminating GCB group and non-GCB group of DLBCL patients (8). Because Hans' algorithm is relatively simple and feasible, many laboratories adopted it as a standard method. However, few studies have demonstrated the validity of Hans' discrimination method in predicting the prognosis of Asian DLBCL patients (9).
It was known that single protein expression of each marker such as CD10, bcl-6, MUM-1, bcl-2 and CD5, also might provide clinical information in DLBCL (8, 10-13). However, studies of the protein expression have reported conflicting results. These results predominantly are due to the differences of the cut-off values and the lack of standardized approach for each marker. Here we performed an analysis addressing the prognostic significance of Hans' method in Korean DLBCL patients who treated with combination chemotherapy with cyclophosphamide, daunorubicin, vincristine, and prednisone (CHOP). We also investigate the clinical significance of individual biomarkers and compared the results with different cut-off values.
All patients who were consecutively diagnosed in Asan Medical Center between September 1999 and September 2004 were retrieved from the database of department of oncology. All of the patients received CHOP chemotherapy without rituximab. Inclusion criteria for the study were a reference diagnosis of DLBCL (134 patients), and the availability of formalin-fixed and paraffin-embedded material for tissue microarray construction (94 patients). All cases were reviewed and were confirmed as DLBCL by two pathologists according to the WHO classification (2008). Patients with transformed lymphoma, AIDS associated tumor, primary mediastinal lymphoma, primary CNS lymphoma, stage I DLBCL, or received rituximab therapy were excluded.
For the tissue microarray (TMA), hematoxylin and eosin-stained sections from each paraffin-embedded, formalin-fixed block were used to define diagnostic areas. Two random, representative 0.6 mm cores were obtained from each case and inserted in a grid pattern into a recipient paraffin block using a tissue arrayer. Sections (5 µm) were cut from each TMA and stained with antibodies to CD20, CD10, bcl-6, MUM1, CD5, CD138, and bcl-2 using the avidin-biotin method. The level of each immunochemical marker was assessed by a modification of the method by Hans et al. (8) in which, a case was considered positive, when 30% or more of the tumor cells were stained with the antibody. A 4-point system was devised based on the proportion of positive cell: 5%, 30%, 50%, and 75%. Each core was evaluated independently by two pathologists, and in case of disagreement, third measurement by the joint review was adopted. The cases were sub-classified into GCB-derived DLBCL and non-GCB derived DLBCL according to the algorithm proposed by Hans et al. (8).
The survival analysis was performed according to the method of Kaplan and Meier. Overall survival (OS) was defined as the time from diagnosis to the date of death or last contact. Progression-free survival (PFS) was defined as the time from diagnosis to the date of progression, death or last contact. Patients were censored for OS at the time of the last contact if currently alive and for PFS if no progression or death had occurred at the time of their last visit. Survival data between defined subgroups were compared with the log-rank test. Multivariate analyses were carried out by a Cox regression model and were used to select variables with independent predictive significance. Statistical data processing was carried out with SPSS software. Probability values less than 0.05 were considered statistically significant.
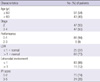
Clinical data were available for all 94 patients included in the study. The patients' median age was 59 yr (range, 18-82) at diagnosis. The median follow up period was 60 months. Five-year progression free survival rate of the whole cases was 59% (95% CI, 54%-64%) and 5 yr overall survival rate was 64% (95% CI, 59%-69%). The characteristics of these patients are listed in Table 1.
Of the 94 cases of DLBCL, expression of CD10 was seen in 9 cases (9.5%), bcl-6 in 27 cases (28.7%), MUM1 in 70 cases (74.4%) at the 30% positivity of cut-off point. Using the algorithm of Hans et al., 18 cases (19.1%) were classified as GCB group and 76 cases (80.9%) were classified as non-GCB group. With a median follow up of 5 yr, there was no significant survival difference between patients with GCB group and those with non-GCB group. The 5-yr PFS estimates ( ± SE) were 61% ± 11% for GCB group vs 58% ± 6% for non-GCB group (P = 0.79, Fig. 1A). For 5-yr OS, the estimates were 72% ± 11% for GCB group vs 62% ± 6% for non-GCB group (P = 0.40, Fig. 1B).
The percentage of positively-stained tumor cells and survival analysis of each biomarker at the different cut off value point are recorded in Table 2. There was no statistical difference of IPI scores (0-2 vs 3-5) between positive and negative group of all biomarkers except bcl-2 by the cut-off point of 75% (P = 0.043). The survival analysis of each biomarker showed variable results with different cut-off point for each marker. Although bcl-6 positive group had longer PFS than negative group, PFS difference was narrowed down from the cut-off point of 5% (P = 0.004) to the cut-off point of 75% (P = 0.116).
In univariate analysis, CD10 negative DLBCL had longer PFS than CD10-positive group at the cut-off point of 30% (P = 0.013; Fig. 2A). CD 10 positivity did not have clinical meaning at any of the other cut-off points. As we mentioned earlier, bcl-6 positive group had significant longer PFS. The bcl-6 positivity had a clinical value at both cut off point of 5% (P = 0.004; Fig. 2B) and 30% (P = 0.018) in PFS analysis. CD5 negative group had longer PFS than CD5 positive group at the cut-off point of 5% (P = 0.009). The IPI had a high value for predicting PFS (P < 0.001). The bcl-6 positive group had longer OS than negative group at the cut-off point of 5% (P = 0.001; Fig. 3). The IPI also had a high value for predicting OS (P < 0.001). The expression of MUM1 and bcl-2 did not correlate with the survival of DLBCL patients in our study.
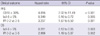
The results of Cox multivariate analyses showed that CD 10 expression at the cut-off point of 30%, bcl-6 expression at the cut-off point of 5% and IPI score were independent prognostic factors of PFS. For OS, bcl-6 expression at the cut-off point of 5% and IPI score were independent prognostic factors of OS in multivariate analysis (Table 3).
Many predictive models have been proposed for better stratification of DLBCL using immunohistochemical stains for germinal center B-cell marker or activated B-cell marker (3, 8, 10). The Nebraska Lymphoma Study Group proposed a classification algorithm (Hans' method) using immunohistochemical stain with CD10, bcl-6 and MUM-1 (8). It is generally accepted that classification of DLBCL by Hans' algorithm gives relevant prognostic information for DLBCL patients treated with CHOP chemotherapy, although it does not reliably predict the survival of DLBCL patients who relapsed or were refractory to initial chemotherapy (14, 15). Recent studies have reported the usefulness of Hans' algorithm even in the rituximab-based chemotherapy era (16, 17). However, there is a disagreement on the prognostic value of Han's classification method in DLBCL patients in the literature (18-20). No correlation was reported between Hans' classification and the survival in the DLBCL patients treated by CHOP or CHOP-like chemotherapy, or CHOP with rituximab in the previous retrospective or prospective studies (18-20). The lack of clinical usefulness of the Hans' classification method in predicting the survival of Korean patients with DLBCL treated with CHOP chemotherapy in the present study agrees with the previous reports, and illustrates the limitation of the currently available immunohistochemical discrimination of the GCB versus non-GCB groups (18-20). The Hans' method has 70%-80% concordance with the gene expression profiling (GEP) classification, while, the remaining 20%-30% is discrepant (8, 18). A new immunostain algorithm recently proposed by Nebraska group uses GCET1, CD10, bcl-6, MUM-1 and FOXP1 (21). Although its reported concordance rate with GEP classification is 93%, its clinical usefulness should be tested in large scale studies in different populations.
Whereas each biomarker had prognostic significance at the uniform cut off value of 30% in the Hans' reports and other studies, each biomarker showed variable results at the cut off value of 30% in the present study (8). As a marker of germinal center, CD10 is generally associated with better prognosis. Interestingly, CD 10 expression was an independent negative prognostic factor of PFS in the present study. Although the small sample size warrants caution in the interpretation, the findings calls for further study in the Korean population on a larger scale to rule out ethnic or regional differences. The low positivity of CD10 stain and high positivity of MUM-1, and the lower proportion of GCB group compared to Western population in our study are in agreement with the previous reports from Japan and China (22, 23).
The BCL6 proto-oncogene, a gene essential for the germinal center formation, is the most commonly translocated gene in DLBCL (24, 25). The expression of bcl-6 protein had a predictive power in both PFS and OS irrelevant of IPI, in agreement with the previous reports (8, 26). Expression of MUM-1 signifies the step of B-cell maturation toward plasma cell, and serves as a marker of activated B-cell (10, 27). It was reported that MUM1 expression was related with worse survival of DLBCL patients (8, 10). Unlike the previous reports of the deleterious effect of MUM1 expression on survival, MUM1 expression had little impact on survival of DLBCL patients in this study. CD5 is an antigen expressed by most T cells and a subset of B cells, and can be infrequently expressed by DLBLCL (28). It is known that CD5 positive DLBLC tumors are observed in elderly women with high IPI score and poor survival (13). In the univariate survival analysis of our study, CD5 expression had a prognostic significance for both PFS and OS. But this prognostic significance became negligible in multivariate analysis.
We showed that prognostic significance of each biomarker varied with different cut-off value. Inter-laboratory technical variations (such as different primary antibodies, different fixation method, various antigen retrieval and signal amplification technique) and inter-observer variations exist (29). In a typical referral center where consultation cases make the significant portion of the cases, the laboratory or the pathologist have no control over many pre-analytic variables including fixation method or the duration of fixation. To overcome these technical variations, Lunenburg lymphoma biomarker consortium recommended the centralized consensus review and validated assessment of biomarkers in each laboratory (30). On the other hand, there may be variations in the significance of these markers among different populations, as seen in this study. We propose that setting up of an optimal cut-off value of each biomarker in the individual laboratory is a viable option.
In conclusion, Hans' classification method subdividing DLBCL to GCB group and non-GCB group had no clinical significance in our study. CD10 negative expression and bcl-6 positive expression group had favorable outcomes in DLBCL patients who treated with CHOP chemotherapy. Because prognostic significance of each biomarker is varied with different cut-off value, the cut-off level of biomarker is needed to be determined with individual institutions' clinical results.
Figures and Tables
Fig. 1
Kaplan-Meier curves of progression-free survival (PFS) (A) and overall survival (OS) (B) based on stratifying diffuse large B cell lymphomas (DLBCL) into germinal center B-cell (GCB) and non-germinal center B-cell (non-GCB) groups.

Fig. 2
Kaplan-Meier curves of progression free survival (PFS) according to CD10 (cut-off 30%) (A) and bcl-6 (cut-off 5%) (B).

AUTHOR SUMMARY
Prognostic Value of Immunohistochemical Biomarkers at Different Cut-off Values in Patients with Diffuse Large B-cell Lymphoma Treated with CHOP Chemotherapy
Sukjoong Oh, Dong Hoe Koo, Cheolwon Suh, Shin Kim, Bong Hee Park, Joon Kang and Jooryung Huh
Hans' algorithm has been widely used to sub-classify diffuse large B-cell lymphoma (DLBCL). However, there is a disagreement in the literature regarding its prognostic significance. Here, we retrospectively analyzed Hans' algorithm and the individual immunohistochemical biomarkers at different cut-off values in 94 DLBCL patients. Although no significant differences were observed between the subgroups, CD10 negativity (cut point: 30%) and bcl-6 positivity (cut point: 5%) were independent good prognostic markers. It is requested to obtain the optimized cut-off values of Han's algorithm for individual laboratory.
References
1. The Non-Hodgkin's Lymphoma Classification Project. A clinical evaluation of the International Lymphoma Study Group classification of non-Hodgkin's lymphoma. Blood. 1997. 89:3909–3918.
2. Anderson JR, Armitage JO, Weisenburger DD. Epidemiology of the non-Hodgkin's lymphomas: distributions of the major subtypes differ by geographic locations. The Non-Hodgkin's Lymphoma Classification Project. Ann Oncol. 1998. 9:717–720.
3. Colomo L, López-Guillermo A, Perales M, Rives S, Martinez A, Bosch F, Colomer D, Falini B, Montserrat E, Campo E. Clinical impact of the differentiation profile assessed by immunophenotyping in patients with diffuse large B-cell lymphoma. Blood. 2003. 101:78–84.
4. The International Non-Hodgkin's Lymphoma Prognostic Factors Poject. A predictive model for aggressive non-Hodgkin's lymphoma. N Engl J Med. 1993. 329:987–994.
5. Barrans SL, Carter I, Owen RG, Davies FE, Patmore RD, Haynes AP, Morgan GJ, Jack AS. Germinal center phenotype and bcl-2 expression combined with the International Prognostic Index improves patient risk stratification in diffuse large B-cell lymphoma. Blood. 2002. 99:1136–1143.
6. Alizadeh AA, Eisen MB, Davis RE, Ma C, Lossos IS, Rosenwald A, Boldrick JC, Sabet H, Tran T, Yu X, Powell JI, Yang L, Marti GE, Moore T, Hudson J Jr, Lu L, Lewis DB, Tibshirani R, Sherlock G, Chan WC, Greiner TC, Weisenburger DD, Armitage JO, Warnke R, Levy R, Wilson W, Grever MR, Byrd JC, Botstein D, Brown PO, Staudt LM. Distinct types of diffuse large B-cell lymphoma identified by gene expression profiling. Nature. 2000. 403:503–511.
7. Rosenwald A, Wright G, Chan WC, Connors JM, Campo E, Fisher RI, Gascoyne RD, Muller-Hermelink HK, Smeland EB, Giltnane JM, Hurt EM, Zhao H, Averett L, Yang L, Wilson WH, Jaffe ES, Simon R, Klausner RD, Powell J, Duffey PL, Longo DL, Greiner TC, Weisenburger DD, Sanger WG, Dave BJ, Lynch JC, Vose J, Armitage JO, Montserrat E, Lopez-Guillermo A, Grogan TM, Miller TP, LeBlanc M, Ott G, Kvaloy S, Delabie J, Holte H, Krajci P, Stokke T, Staudt LM. Lymphoma/Leukemia Molecular Profiling Project. The use of molecular profiling to predict survival after chemotherapy for diffuse large-B cell lymphoma. N Engl J Med. 2002. 346:1937–1947.
8. Hans CP, Weisenburger DD, Greiner TC, Gascoyne RD, Delabie J, Ott G, Müller-Hermelink HK, Campo E, Braziel RM, Jaffe ES, Pan Z, Farinha P, Smith LM, Falini B, Banham AH, Rosenwald A, Staudt LM, Connors JM, Armitage JO, Chan WC. Confirmation of the molecular classification of diffuse large B-cell lymphoma by immunohistochemistry using a tissue microarray. Blood. 2004. 103:275–282.
9. Oh YH, Park CK. Prognostic evaluation of nodal diffuse large B cell lymphoma by immunohistochemical profiles with emphasis on CD138 expression as a poor prognostic factor. J Korean Med Sci. 2006. 21:397–405.
10. Chang CC, McClintock S, Cleveland RP, Trzpuc T, Vesole DH, Logan B, Kajdacsy-Balla A, Perkins SL. Immunohistochemical expression patterns of germinal center and activation B-cell markers correlate with prognosis in diffuse large B-cell lymphoma. Am J Surg Pathol. 2004. 28:464–470.
11. Hill ME, MacLennan KA, Cunningham DC, Vaughan Hudson B, Burke M, Clarke P, Di Stefano F, Anderson L, Vaughan Hudson G, Mason D, Selby P, Linch DC. Prognostic significance of BCL-2 expression and bcl-2 major breakpoint region rearrangement in diffuse large cell non-Hodgkin's lymphoma: a British National Lymphoma Investigation Study. Blood. 1996. 88:1046–1051.
12. Gascoyne RD, Adomat SA, Krajewski S, Krajewska M, Horsman DE, Tolcher AW, O'Reilly SE, Hoskins P, Coldman AJ, Reed JC, Connors JM. Prognostic significance of Bcl-2 protein expression and Bcl-2 gene rearrangement in diffuse aggressive non-Hodgkin's lymphoma. Blood. 1997. 90:244–251.
13. Yamaguchi M, Seto M, Okamoto M, Ichinohasama R, Nakamura N, Yoshino T, Suzumiya J, Murase T, Miura I, Akasaka T, Tamaru J, Suzuki R, Kagami Y, Hirano M, Morishima Y, Ueda R, Shiku H, Nakamura S. De novo CD5+ diffuse large B-cell lymphoma: a clinicopathologic study of 109 patients. Blood. 2002. 99:815–821.
14. van Imhoff GW, Boerma EJ, van der Holt B, Schuuring E, Verdonck LF, Kluin-Nelemans HC, Kluin PM. Prognostic impact of germinal center-associated proteins and chromosomal breakpoints in poor-risk diffuse large B-cell lymphoma. J Clin Oncol. 2006. 24:4135–4142.
15. Nyman H, Adde M, Karjalainen-Lindsberg ML, Taskinen M, Berglund M, Amini RM, Blomqvist C, Enblad G, Leppä S. Prognostic impact of immunohistochemically defined germinal center phenotype in diffuse large B-cell lymphoma patients treated with immunochemotherapy. Blood. 2007. 109:4930–4935.
16. Wilson WH, Dunleavy K, Pittaluga S, Hegde U, Grant N, Steinberg SM, Raffeld M, Gutierrez M, Chabner BA, Staudt L, Jaffe ES, Janik JE. Phase II study of dose-adjusted EPOCH and rituximab in untreated diffuse large B-cell lymphoma with analysis of germinal center and post-germinal center biomarkers. J Clin Oncol. 2008. 26:2717–2724.
17. Fu K, Weisenburger DD, Choi WW, Perry KD, Smith LM, Shi X, Hans CP, Greiner TC, Bierman PJ, Bociek RG, Armitage JO, Chan WC, Vose JM. Addition of rituximab to standard chemotherapy improves the survival of both the germinal center B-cell-like and non-germinal center B-cell-like subtypes of diffuse large B-cell lymphoma. J Clin Oncol. 2008. 26:4587–4594.
18. Veelken H, Vik Dannheim S, Schulte Moenting J, Martens UM, Finke J, Schmitt-Graeff A. Immunophenotype as prognostic factor for diffuse large B-cell lymphoma in patients undergoing clinical risk-adapted therapy. Ann Oncol. 2007. 18:931–939.
19. Dupuis J, Gaulard P, Hemery F, Itti E, Gisselbrecht C, Rahmouni A, Copie-Bergman C, Brière J, El Gnaoui T, Gaillard I, Meignan M, Haioun C. Respective prognostic values of germinal center phenotype and early (18) fluorodeoxyglucose-positron emission tomography scanning in previously untreated patients with diffuse large B-cell lymphoma. Haematologica. 2007. 92:778–783.
20. Ott G, Ziepert M, Klapper W, Horn H, Szczepanowski M, Bernd HW, Thorns C, Feller AC, Lenze D, Hummel M, Stein H, Müller-Hermelink HK, Frank M, Hansmann ML, Barth TF, Moller P, Cogliatti S, Pfreundschuh M, Schmitz N, Trümper L, Loeffler M, Rosenwald A. Immunoblastic morphology but not the immunohistochemical GCB/nonGCB classifier predicts outcome in diffuse large B-cell lymphoma in the RICOVER-60 trial of the DSHNHL. Blood. 2010. 116:4916–4925.
21. Choi WW, Weisenburger DD, Greiner TC, Piris MA, Banham AH, Delabie J, Braziel RM, Geng H, Iqbal J, Lenz G, Vose JM, Hans CP, Fu K, Smith LM, Li M, Liu Z, Gascoyne RD, Rosenwald A, Ott G, Rimsza LM, Campo E, Jaffe ES, Jaye DL, Staudt LM, Chan WC. A new immunostain algorithm classifies diffuse large B-cell lymphoma into molecular subtypes with high accuracy. Clin Cancer Res. 2009. 15:5494–5502.
22. Shiozawa E, Yamochi-Onizuka T, Takimoto M, Ota H. The GCB subtype of diffuse large B-cell lymphoma is less frequent in Asian countries. Leuk Res. 2007. 31:1579–1583.
23. Chen Y, Han T, Iqbal J, Irons R, Chan WC, Zhu X, Fu K. Diffuse large B-cell lymphoma in Chinese patients: immunophenotypic and cytogenetic analyses of 124 cases. Am J Clin Pathol. 2010. 133:305–313.
24. Kerckaert JP, Deweindt C, Tilly H, Quief S, Lecocq G, Bastard C. LAZ3, a novel zinc-finger encoding gene, is disrupted by recurring chromosome 3q27 translocations in human lymphomas. Nat Genet. 1993. 5:66–70.
25. Ye BH, Cattoretti G, Shen Q, Zhang J, Hawe N, de Waard R, Leung C, Nouri-Shirazi M, Orazi A, Chaganti RS, Rothman P, Stall AM, Pandolfi PP, Dalla-Favera R. The BCL-6 proto-oncogene controls germinal-centre formation and Th2-type inflammation. Nat Genet. 1997. 16:161–170.
26. Winter JN, Weller EA, Horning SJ, Krajewska M, Variakojis D, Habermann TM, Fisher RI, Kurtin PJ, Macon WR, Chhanabhai M, Felgar RE, Hsi ED, Medeiros LJ, Weick JK, Reed JC, Gascoyne RD. Prognostic significance of Bcl-6 protein expression in DLBCL treated with CHOP or RCHOP: a prospective correlative study. Blood. 2006. 107:4207–4213.
27. Gaidano G, Carbone A. MUM1: a step ahead toward the understanding of lymphoma histogenesis. Leukemia. 2000. 14:563–566.
28. Burns BF, Warnke RA, Doggett RS, Rouse RV. Expression of a T-cell antigen (Leu-1) by B-cell lymphomas. Am J Pathol. 1983. 113:165–171.
29. Lossos IS, Morgensztern D. Prognostic biomarkers in diffuse large B-cell lymphoma. J Clin Oncol. 2006. 24:995–1007.
30. de Jong D, Rosenwald A, Chhanabhai M, Gaulard P, Klapper W, Lee A, Sander B, Thorns C, Campo E, Molina T, Norton A, Hagenbeek A, Horning S, Lister A, Raemaekers J, Gascoyne RD, Salles G, Weller E. Lunenburg Lymphoma Biomarker Consortium. Immunohistochemical prognostic markers in diffuse large B-cell lymphoma: validation of tissue microarray as a prerequisite for broad clinical applications--a study from the Lunenburg Lymphoma Biomarker Consortium. J Clin Oncol. 2007. 25:805–812.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download