Abstract
Resection of retroperitoneal tumors is usually perfomed using the anterior retroperitoneal approach. Our report presents an innovative method utilizing a robotic surgical system. A 50-yr-old male patient visited our hospital due to a known paravertebral mass. Magnetic resonance imaging showed a well-encapsulated mass slightly abutting the abdominal aorta and left psoas muscle at the L4-L5 level. The tumor seemed to be originated from the prevertebral sympathetic plexus or lumbosacral trunk and contained traversing vessels around the tumor capsule. A full-time robotic transperitoneal tumor resection was performed. Three trocars were used for the robotic camera and working arms. The da Vinci Surgical System® provided delicate dissection in the small space and the tumor was completely removed without damage to the surrounding organs and great vessels. This case demonstrates the feasibility of robotic resection in retroperitoneal space. Robotic surgery offered less invasiveness in contrast to conventional open surgery.
Despite the breakthrough of the endoscope, the development of minimally invasive approaches in spinal surgery using this technology has proved challenging. The laparoscopic anterior approach was highlighted after its first publication in 1995 (1), but surgical results related to the superiority of the new method compared to the conventional open and mini-open anterior approaches were unconvincing (2-5).
During the past decade, robotic surgical systems have been developed continuously, and these advances have allowed for the substitution of laparoscopic procedures in many surgical fields due to the realization of 3D vision and enhanced ergonomics (6-8). A paravertebral tumor in the retroperitoneal space usually requires wide exposure and retraction of the peritoneal organs or great vessels for its removal. The laparoscopic approach is an endeavoring method, but it satisfactorily cannot offer visual cues and instrumental motion. In response, robotic surgical systems are expected to be a solution for these problems. The objective of our report is to present advantages of robotic surgery in deep-seated retroperitoneal neurogenic tumors requiring gentle dissection and minimal retraction.
A 50-yr-old male patient who had a known paravertebral mass visited our clinic on August 11, 2009. He underwent discectomy on the right side at the L4-5 level due to 6-month long radiculopathy. At that time, magnetic resonance imaging (MRI) scans revealed a round, encapsulated left paravertebral mass at the same level. However, since the patient had not complained of any symptoms caused by the mass, and a posterior approach was not feasible, it was decided that the mass would be observed for six months. During follow-up, MRI scan showed the mass had double in size and was located on the left side of the L4 vertebral body, close to the aortic bifurcation; the patient additionally complained of numbness on his left posterior thigh (Fig. 1). As a result, several options such as observation, tissue biopsy or surgery were proposed, and the patient chose surgery. The patient underwent surgery on August 12, 2009.
The patient was placed in a right semilateral position. A 12-mm trocar for the camera was made just above the umbilicus. Two 8-mm trocars were introduced 8-10 cm away from the camera port. A trocar for right side robotic arm was introduced directed to the symphysis pubis and left side trocar was made at an intersecting point between the left mid-clavicular line and the imaginary line from umbilicus to left anterior superior iliac spine. Another 12-mm trocar was made for suction and assistance between the camera port and 8-mm trocar. The distances between the trocars were decided enough for avoiding collisions of instruments (Fig. 2). After trocar insertion, the da Vinci Surgical System® was introduced from the backside of the patient cart. Maryland bipolar forceps and monopolar curved scissors were employed as the left and right instruments, respectively (Fig. 3A). Detachment of the large bowel from the posterior peritoneal wall was performed after CO2 inflation. The left psoas muscle and ureter were noted beneath the transparent posterior peritoneum (Fig. 3A). Incision of the posterior peritoneum was made at the left renal artery level, then the left kidney and psoas muscle was definitively identified. By tracing the left psoas muscle, the oval shape mass was noticed. The mass was slightly abutting the aorta but it did not adhere to the vessel. The tumor was dissected and small vessels traversing the tumor capsule were coagulated with bipolar forceps. After circumferential dissection, the tumor was excised with minimal traction of the originating nerve (Fig. 3B). The specimen was placed in the EndoCatch retrieval bag (Autosuture, Norwalk, CT, USA) and removed through the assistant port. During the pocedure, the amount of bleeding was less than 100 cc. Setup time for the da Vinci Surgical System® was 30 min, and the total time of anesthesia was 160 min. The sum of all incisions was 6 cm. Although the bleeding was minimal, we left an indwelling catheter for delayed bleeding. The catheter was withdrawn the day after the surgery. The patient started a diet 6 hr after the surgery and was discharged 48 hr after the surgery. The pathological diagnosis of the tumor was schwannoma.
Anterior retroperitoneal approach is the most employed method for paravertebral neurogenic tumor resection. However, the retroperitoneal approach requires a relatively large incision, and the risk of great vessel and peritoneal organ damage or nerve injury is substantial. Moreover, if the tumor is located deep in the pelvic floor, the surgical field may be limited to a narrow space.
The laparoscopic approach has been applied to many types of abdominal procedures. Laparoscopic surgery can offer shorter hospital stays, cosmetic advantages, and early recovery. It has substituted various conventional surgeries as a minimally invasive surgical tool. In the spinal surgical field, spinal anterior fusion using the laparoscope was also spotlighted in the 1990s, but the merits of the laparoscope have not been established yet because of its steep learning curve coupled with the surgeon's unfamiliarity with intra-abdominal anatomy. In addition, a higher probability of complication, such as retrograde ejaculation, compared with the conventional approach also has prevented its spread (1, 2, 4). The da vinci Surgical System® remarkably improved laparoscopic procedures with enhanced visual information and improved dexterity. Therefore, it was not difficult to learn and practice this robotic system even though we had no prior experience in laparoscopic surgery.
A few reports about the robotic surgery in the removal of paravertebral tumors have been reported by cardio-thoracic surgeons and urologists. They have reported the advantages of utilizing robotic technology in laparoscopic procedures, highlighting the minimal morbidity, reduced hospital stay, and rapid recovery normally associated with robot-assisted procedure (9-11). Moskowitz RM et al. (9) reported a successful resection of a thoracolumbar neurofibroma using the da Vinci surgical system®. Although laparoscopic removal of a neurofibroma had already been reported, that report was notable because a purely laproscopic approach without hand assistance was rare. We have previously tested the feasibility of employing robotic technology to approach the vertebral column in a swine model (12).
Currently, it seems to us that the most appropriate use of robotic surgery in spinal neurosurgery is when resecting a paraspinal tumor because the minmal invasiveness and increased laparoscopic dexterity help make the robotic-assisted procedure excellent. The lack of EndoWrist® equipments for work on spinal column and for spinal instrumentation notwithstanding, application of robotic surgical system in the different areas of spinal surgery is indeed promising.
In our case, the tumor was located in the deep retroperitoneal paravertebral space and quite close to the aortic bifurcation. We decided to perform tranasperitoneal tumor excision with the da Vinci Surgical System® in light of these facts. Robotic paravertebral tumor removal offered clear, three-dimensional images of the operating field and enabled delicate dissection from the aorta and originating nerve (6, 13, 14). It also offered a similar freedom of motion comparable to human hands.
In contrast to the conventional retroperitoneal approach, this procedure required minimal retraction, and limited damage to the psoas muscle and internal organs along with meticulous bleeding control was facilitated with this magnified view. The operation time was 160 min, but with repeated training and clinical experience, the time necessary to set up the system and perform the surgery itself is certainly able to decrease. Although it took longer setup time, whole opeartion time was not increased in contrast to our conventional retroperitoneal approach. The patient was content with the minimal incision, and a quick diet after the surgery, he was discharged 2 days after surgery. Histopathological examination revealed a benign schwannoma with focal hemorrhage. Although there are a few case reports about rapidly growing vestibular schwannoma (15-18), most benign paraspinal neurogenic tumor have a slow growth rate. In the present case, tumor diameter was increased but, the focal hemorrhagic component and case of tumor size is not understood. Further immunochemical study is required for determining identifying the charachteristic.
Robot-assisted removal of paravertebral tumors in the lumbosacral area appears to be very useful, especially if the tumors are deeply seated and surrounded with vital organs. Moreover, application to another type of spinal surgery, such as anterior interbody fusion, also seems feasible with this robotic system. Although the da Vinci Surgical System® still depends on a visual cue without tactile communication, it certainly can promote the surgeon's dexterity with a gentle learning curve (19).
This illustrative case demonstrates the utility of robotic surgery in the removal of a paravertebral tumor. Robotic removal of the paravertebral tumor proved superior to the conventional retroperitoneal approach with respect to its minimal invasiveness and increased safety. There is no doubt that its use will become yet another breakthrough in minimally-invasive spinal surgery.
Figures and Tables
Fig. 1
Enlarged mass 6 month after the initial MRI scan. Preoperative sagittal (A) and axial (B) T1 enhanced Magnetic Resonance Imaging sans showing a round encapsulated left paravertebral mass at the L4-5 level and CT angiography (C) demonstrating the location close to the aortic bifurcation (Arrow indicates tumor mass).

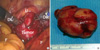
Fig. 3
Operative findings of robot-assisted paraspinal tumor resection. (A) Dissection of tumor through robotic bipolar forceps and monopolar scissors (U, ureter; DL, left arm of da Vinci; DR, right arm of da Vinci; F, paracolic fat). (B) Tumor specimen (4 × 3 × 4 cm) was removed successfully with robot assisted resection.
References
1. Mathews HH, Evans MT, Molligan HJ, Long BH. Laparoscopic discectomy with anterior lumbar interbody fusion: a preliminary review. Spine (Phila Pa 1976). 1995. 20:1797–1802.
2. Inamasu J, Guiot BH. Laparoscopic anterior lumbar interbody fusion: a review of outcome studies. Minim Invasive Neurosurg. 2005. 48:340–347.
3. Kaiser MG, Haid RW Jr, Subach BR, Miller JS, Smith CD, Rodts GE Jr. Comparison of the mini-open versus laparoscopic approach for anterior lumbar interbody fusion: a retrospective review. Neurosurgery. 2002. 51:97–103.
4. Zdeblick TA, David SM. A prospective comparison of surgical approach for anterior L4-L5 fusion: laparoscopic versus mini anterior lumbar interbody fusion. Spine (Phila Pa 1976). 2000. 25:2682–2687.
5. Chung SK, Lee SH, Lim SR. Comparative study of laparascopic L5-S1 fusion versus open mini-anterior lumbar interbody fusion. J Korean Neurosurg Soc. 2003. 33:154–159.
6. Ballantyne GH. Robotic surgery, telerobotic surgery, telepresence, and telementoring. Surg Endosc. 2002. 16:1389–1402.
7. Moorthy K, Munz Y, Dosis A, Hernandez J, Martin S, Bello F, Rockall T, Darzi A. Dexterity enhancement with robotic surgery. Surg Endosc. 2004. 18:790–795.
8. Rha KH. The present and future of robotic surgery. J Korean Med Assoc. 2008. 51:67–73.
9. Moskowitz RM, Young JL, Box GN, Paré LS, Clayman RV. Retroperitoneal transdiaphragmatic robotic-assisted laparoscopic resection of a left thoracolumbar neurofibroma. JSLS. 2009. 13:64–68.
10. Morgan JA, Kohmoto T, Smith CR, Oz MC, Argenziano M. Endoscopic computer-enhanced mediastinal mass resection using robotic technology. Heart Surg Forum. 2003. 6:E164–E166.
11. Ruurda JP, Hanlo PW, Hennipman A, Broeders IA. Robot-assisted thoracoscopic resection of a benign mediastinal neurogenic tumor: technical note. Neurosurgery. 2003. 52:462–464.
12. Kim MJ, Ha Y, Yang MS, Yoon DH, Kim KN, Kim H, Yang JW, Lee JY, Yi S, Jung WJ, Rha KH. Robot-assisted anterior lumbar interbody fusion (ALIF) using retroperitoneal approach. Acta Neurochir (Wien). 2010. 152:675–679.
13. Lanfranco AR, Castellanos AE, Desai JP, Meyers WC. Robotic surgery: a current perspective. Ann Surg. 2004. 239:14–21.
14. Mack MJ. Minimally invasive and robotic surgery. JAMA. 2001. 285:568–572.
15. Harada K, Nishizaki T, Adachi N, Suzuki M, Ito H. Pediatric acoustic schwannoma showing rapid regrowth with high proliferative activity. Childs Nerv Syst. 2000. 16:134–137.
16. Hwang SK, Kim DG, Paek SH, Kim CY, Kim MK, Chi JG, Jung HW. Aggressive vestibular schwannomas with postoperative rapid growth: clinicopathological analysis of 15 cases. Neurosurgery. 2002. 51:1381–1390.
17. Seol HJ, Jung HW, Park SH, Hwang SK, Kim DG, Paek SH, Chung YS, Lee CS. Aggressive vestibular schwannomas showing postoperative rapid growth-their association with decreased p27 expression. J Neurooncol. 2005. 75:203–207.
18. Ohta S, Yokoyama T, Nishizawa S. Massive haemorrhage into acoustic neurinoma related to rapid growth of the tumour. Br J Neurosurg. 1998. 12:455–457.
19. Maniar HS, Council ML, Prasad SM, Prasad SM, Chu C, Damiano RJ Jr. Comparison of skill training with robotic systems and traditional endoscopy: implications on training and adoption. J Surg Res. 2005. 125:23–29.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download