Abstract
The factors related to death and functional recovery after primary pontine hemorrhage (PPH) in Koreans has not been well defined. The authors sought to identify independent predictors of death and functional recovery after PPH using data obtained at a single institute. Data were collected retrospectively on 281 patients with PPH admitted to the Stroke Unit at our hospital between January 1, 2000 and December 31, 2009. Multivariate logistic regression analysis was used to evaluate the associations between selected variables and 30-day mortality and 90-day functional recovery after PPH. One-hundred and ten patients (39.1%) died within 30 days of PPH and 27 patients (9.6%) achieved functional recovery within 90 days. By multivariate analysis, unconsciousness, dilated pupils, abnormal respiration, systolic blood pressure < 100 mmHg, hydrocephalus, and conservative treatment were found to be predictors of 30-day mortality, whereas consciousness, intact motor function, no history of hypertension or diabetes mellitus, intact eye movement, a hematoma volume of < 5 mL, no ventricular hemorrhage, and normally sized ventricle were found to be predictors of 90-day functional recovery. The present findings suggest that systolic hypotension of less than 100 mmHg may predict 30-day mortality and a history of underlying hypertension and diabetes mellitus may predict 90-day functional recovery.
Primary pontine hemorrhage (PPH) is extremely rare in patients with hemorrhagic stroke, and accounts for only about 5%-10% of intracranial hemorrhages. PPH has an incidence of 2-4 per 100,000 of the population per annum (1-3), and reported mortality rates vary widely from 30% to 90% (4-6). The classical clinical features of PPH at presentation are; coma, quadriplegia, ophthalmoparesis, and pinpoint pupils (4, 7). In the past, PPH were accepted as fatal, but computed tomography (CT) allows now small PPH to be defined, and thus, mortality rates have decreased (8). Continuous and numerous efforts have been made to improve the outcome of patients with PPH, and developments in the stereotactic surgery and microsurgery field have undoubtedly improved outcomes (9, 10). However, PPH does not have a uniform prognosis, and varies from early death to long-term survival without neurological deficits (7). Accordingly, studies on decisive factors that lead to early death or a better outcome are useful in clinical practice. In recent studies, a fatal outcome was reported in patients with coma on admission, pupillary abnormalities, intraventricular extension, hydrocephalus, or a large hematoma (4, 8). Furthermore, Murata et al. (4) and Wessels et al. (2) reported a significant correlation between death and age. However, the numbers of PPH patients enrolled in previous reports were relatively small, and precise statistical analyses were lacking. In Korea, although several reports have been published on the clinical outcomes and prognostic factors of PPH, only one study on 41 patients utilized multivariate analysis to identify prognostic factors (11). Despite the increasing prevalence of ischemic stroke attributed to a rapid westernization of lifestyle, PPH is being increasingly diagnosed in Korea (12, 13). Furthermore, studies undertaken to identify predictors of outcome have largely been performed in the Western countries or in Japan (1-5, 8). Accordingly, the factors related to death and functional recovery after PPH in the Korean population has not been well defined.
To evaluate the effectivenesses of treatment strategies, and to optimize the managements of individuals in accord with established prognostic factors, reliable predictors of death and functional outcome should be identified. Using previously established putative prognostic variables obtained from the literature and the results of our single institute-based multivariate analysis, we sought to identify independent predictors of death and functional recovery after PPH in the Korean population based on experiences at a single institute.
Between January 1, 2000 and December 31, 2009, 322 patients with a diagnosis of PPH were admitted to the Stroke Unit at our hospital (a university hospital, serving a population of about 1,500,000 people). Of these 322 patients, 281 had available medical and radiological records which met the inclusion criteria, and these patients constituted our study cohort. We extracted all patient-related data from a computerized database (PACS; m-view™, Marosis Corporation). Three clinical research coordinators independently extracted and recorded patient information using a structured form. To preserve patient confidentiality, patient identifiers were omitted from the collated data set. The inclusion criteria applied were; a diagnosis of PPH verified by CT or magnetic resonance imaging (MRI) and admission to the stroke unit within 24 hr of symptom onset. As recommended by the Stroke Council of the American Heart Association (SCAHA) (14), selected patients underwent conventional angiography to identify secondary causes of intracerebral hemorrhage. Patients with hemorrhage secondary to head trauma, a ruptured cerebral aneurysm, an arteriovenous malformation, a tumor, bleeding diathesis, or a hemorrhagic infarction were excluded.
Of the baseline variables recorded, we selected age, sex, cigarette smoking and alcohol intake histories, body mass index (BMI), diabetes mellitus, hypertension, hyperlipidemia, hepatopathy, and a family history of stroke because according to the literature they are the most epidemiologically relevant prognostic indicators (1-5, 8, 11). Historical features were dichotomized as present or absent; these included current smoking or a history of smoking (≥ 10 cigarettes/day, ≥ 6 months), and alcohol intake (≥ 46 g/day, 3 days/week) (15). BMI was defined as weight in kilograms divided by height in meters squared.
Prodromal symptoms reported by patients or their relatives were noted. In addition, we selected the following potential clinically prognostic indicators based on literature accounts (1-5, 8, 11); consciousness at admission, pupillary reflex, motor weakness, ophthalmoparesis, violent shivering, abnormal posture to noxious stimulation, hyperthermia, abnormal respiration, seizure, and systolic blood pressure. For statistical analysis, patients were classified as conscious, stuporous, or in coma on admission.
Cranial CTs were performed on admission. All radiologic features were available for analysis, that is, volume of hemorrhage (< 5 mL vs ≥ 5 mL), location of hemorrhage, ventricular extension, and hydrocephalus. Hemorrhagic volumes were measured using the ellipsoid formula (4/3π × A × B × C) where A, B and C represent the respective radii in three dimensional images (16). Hemorrhages where divided into three types (dorsal, ventral, and massive), according to the CT classification of Chung and Park (6). Hematomas were classified as dorsal when the location of the PPH was uni- or bilateral tegmental, sparing the base pontis, as ventral when the hematoma occupied the ventral base pontis and the junction between the bilateral tegmentum, and as massive when hematoma occupied the base pontis and the bilateral tegmentum with extension to the midbrain. Two neuroradiologists individually conducted the radiologic review to diagnose PPH and determine their types.
Patients were treated in accord with a treatment algorithm used at our institution. Surgical approaches were individualized based on site, PPH size, and associated intraventricular hemorrhage or hydrocephalus. The techniques utilized included; suboccipital craniotomy (CO), suboccipital craniectomy (CE), CT-guided stereotactic hematoma evacuation, and/or extraventricular drainage (EVD). The attending neurosurgeon decided whether to implant a bone flap (CO or CE) depending on the intra-operative presence of cerebellar swelling after PPH removal. EVD was performed alone or combined with open surgery or stereotactic evacuation for intracranial pressure (ICP) control, particularly in the setting of hydrocephalus or intraventricular hemorrhage. When an intraventricular catheter was used to monitor ICP, cerebrospinal fluid (CSF) drainage was accomplished by intermittent drainage for short periods in response to ICP elevation. All patients (medical and surgical) were cared for in a neurosurgical intensive care unit until they were considered stable enough to move to a general unit. Hypertension was regulated early during the course of therapy, by setting a target maximal systolic blood pressure (SBP). During the first 24 hr, labetalol was initial administered to maintain an SBP of < 160 mmHg, despite the risk of bradycardia posed by labetalol. We also used continuous intravenous nicardipine or nitroprusside anti-hypertensive therapy when blood pressure was not controlled by labetalol or hydralazine. During the next 48 to 72 hr, the target SBP was usually set at 140 mmHg, and enteral anti-hypertensives were started when SBP was maintained below this level. We also used a hypertonic agent (mannitol) when CT indicated a mass effect or when clinical symptoms showed increased ICP signs, such as severe headache with vomiting and decreased mentation. Mannitol was initially administered at 0.6 to 1.0 g/kg intravenously, followed by 0.25-0.5 g/kg every 4 hr for 4 days, and then tapered over 2 days. Treatment included invasive monitoring of ICP when indicated. Using an ICP monitor (infrared parenchymal catheter, Camino, Integra Life Science Corporation, Plainsboro, NJ, USA), an ICP elevation was defined as > 20 mmHg and cerebral perfusion pressure was maintained at 70 to 100 mmHg.
Patients were followed for at least 90 days after PPH. Outcomes were assessed as mortality within 30 days of symptom onset (post-PPH), and as functional statuses in patients that survived for more than 90 days post-PPH (17), which were assessed using the Modified Rankin's Scale (MRS) as follows; no symptom (MRS 0), symptomatic but no disability (MRS 1), mild disability (MRS 2), moderate disability with independent walking (MRS 3), severe disability (MRS 4), bedridden state (MRS 5), and death (MRS 6). For statistical purposes, patients were assigned to two outcome category groups, namely, the "functional recovery" group (MRS 0, 1, 2, 3), members of which were functionally independent, and the "non-functional recovery" group (MRS 4, 5, 6). Information on mortality and functional outcome was categorized using medical records, information obtained from family members by telephone interviews, or by direct patient examinations conducted at our outpatient department after discharge.
Our primary aim was to identify associations between the selected variables and 30-day mortality and 90-day functional recovery. Univariate analysis was used initially to identify possible relations between outcome and each of the potential prognostic factors using the chi-squared test. Subsequently, multivariate logistic regression analysis was used to identify those variables independently associated with functional recovery and mortality. Kaplan-Meier survival curve analysis was used to depict cumulative mortalities. The analysis was performed using SPSS Ver. 12.0 for Windows (SPSS Institute, Inc., Chicago, IL, USA), and statistical significance was accepted for P values of < 0.05.
This retrospective and a single institute-based study protocol was approved by the Institutional Review Board (MSH 2008-010) at our hospital and informed consent was obtained from all the subjects if survived or one of family members if died or unconscious for collection of clinical data. The data presented in this report has never been published or submitted for publication wholly or in part.
Two-hundred and eighty-one eligible records were identified and analyzed during the course of this study. Of the 281 study subjects, 202 (71.9%) were male and 79 (28.1%) were female. Mean patient age was 56.4 ± 16.3 yr (range 27-85 yr). The mortality rate at 30 days after PPH was 39.1% (n = 110), and 140 deaths (49.8%) occurred within 3 months, 162 (57.7%) within 6 months, and 182 (64.8%) within 12 months. Fig. 1 shows cumulative mortalities during the at least 6 month follow-up period. For all study subjects, the rate of a good functional recovery at 90 days was 9.6% (n = 27), and at 90 days post-PPH, the rate of a good functional recovery was 19.1% among the 141 that survived at 90 days post-PPH. Eighty-six (30.6%) of the study subjects underwent surgical intervention and 195 (69.4%) received initial conservative treatment. The most frequently used surgical technique was CT-guided stereotactic PPH evacuation, which was used in 114 patients (40.7%).
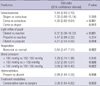
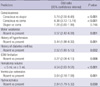
Univariate analysis showed that the following variables were significantly associated with death during the first 30 days post-PPH (Tables 1, 2, 3, 4); a previous history of diabetes mellitus, hypertension, unconsciousness at admission, dilated pupils, limb weakness, ophthalmoplegia, an abnormal posture to noxious stimulation, abnormal respiration, systemic hypotension at admission, a hemorrhage volume ≥ 5 mL, a massive hemorrhage, ventricular extension of hemorrhage, presence of hydrocephalus, and conservative treatment. For surgically treated patients, surgical technique and time to surgery were not found to be associated with 30-day mortality.
Multivariate logistic regression analysis was performed on the variables identified by univariate analysis results and on those mentioned in the literature. Results are presented in Table 5. Multivariate analysis showed that a comatose mentality, dilated pupils, abnormal respiration, a SBP < 100 mmHg at admission, hydrocephalus, and conservative treatment were independently associated with 30-day mortality. Other variables found to be associated with 30-day mortality by univariate analysis were not found to be associated by multivariate analysis.
At 90 days after diagnosis of PPH, there were 141 survivors (50.2%), and of these survivors, 27 (9.6% of all patients) achieved functional recovery (MRS 0, 1, 2, 3), and 254 (90.4% of all patients) achieved a non-functional recovery (MRS 4, 5). Of the selected variables, the following were found to be significantly associated with functional recovery by univariate analysis (Tables 1-4); BMI < 25, absence of history of underlying diabetes, hypertension, consciousness, normal reactive pupils, normal respiration, a hematoma volume of < 5 mL, basal and dorsal type of hemorrhage, and the absence of limb weakness, ophthalmoplegia, an abnormal postural response to pain, and hydrocephalus. Surgical treatment which was associated with 30-day mortality was not associated with functional recovery. Additionally, it was observed that in the surgically treated patients, surgical technique and time to surgery were not associated with good functional recovery by univariate analysis.
Multivariate logistic regression analysis showed that the following eight admission variables were independently associated with a good functional recovery at 90 days post-PPH (Table 6); conscious mentality, a hematoma volume of < 5 mL, and the absence of ventricular extension of blood, hydrocephalus, limb weakness, a history of underlying diabetes, hypertension, and ophthalmoplegia. Other variables found to be associated with good functional recovery at 90 days post-PPH by univariate analysis were not found to be associated by multivariate analysis.
This is the largest multivariate analysis performed to date at a single institute in Korea on the predictors of outcome after PPH. Only one multivariate logistic analysis has been previously conducted to determine the predictors of survival and functional outcome after PPH by Jung et al. in 2007 (11). The previous study was performed on 41 PPH patients, and it was found that transverse hematoma diameter and initial consciousness were independently associated with survival rate. In addition, it was suggested that long-term outcome is influenced by initial consciousness, transverse diameter, antero-posterior diameter, and hematoma volume. However, surgical treatment was not included among the treatment modalities-all patients were treated conservatively. We believe this is why hematoma volume was found to be associated with survival by Jung et al. (11). On the other hand, we found no association between hematoma volume and survival. We treated PPH patients with a volume exceeding 5 mL by surgical intervention, and we believe that these surgical interventions are responsible for the discrepancy between our result and that of Jung et al. (11).
The efficacy of surgery in PPH patients remains debatable. Fewel et al. (18) and Manno et al. (19) suggested that surgical management offers no benefit to patients with a brainstem hemorrhage, whereas Han et al. (20) and Hara et al. (9) advocated the efficacy of the surgical treatment of PPH. In the present study, surgical treatment is associated with a low 30-day mortality by univariate and multivariate analysis, but not with better functional recovery at 90-day post-PPH. Although a controlled comparative clinical trial is needed to determine the efficacy of the surgical treatment for PPH, such a trial is likely to pose ethical problems regarding which can be originated from weak evidence. In fact, our results and those of Hara et al. (9) are somewhat limited because randomization was not performed and because of selection bias. Furthermore, surgical therapy is not standard therapy for PPH and is probably limited to selected indications at specialized centers. For example, at our institute, large or dorsally exophytic hematomas tend to be treated by surgery, such as, by suboccipital craniotomy or craniectomy and CT-guided stereotactic aspiration. And, it was thought to be same reason that intraventricular extension of hemorrhage was not correlated with outcome.
Some reports have suggested that intraventricular PPH extension is associated with a fatal outcome (4, 8). However, the present study shows that intraventricular PPH extension is not associated with high 30-day mortality, but associated with poorer 90-day functional recovery. This result is believed to be due to the frequent extraventricular drainage conducted in cases with intraventricular hemorrhage. In terms of acute hydrocephalus, Murata et al. (4) found no improvement in outcome when acute hydrocephalus in PPH was treated by extraventricular drainage. Similarly, we found that acute hydrocephalus was associated with a high 30-day mortality rate despite frequent extraventricular drainage.
Although many studies have reported that hypertension is the most common cause of PPH (1-3, 7, 8), its effect on clinical outcome remains debatable. In the present study, it is interesting to find that a systolic hypotension of < 100 mmHg at admission was associated with a high risk of mortality within 30 days. On the other hand, Dziewas et al. (1) found that an extremely high systolic pressure (> 180 mmHg) at admission was strongly associated with death in PPH patients. However, in the present study, 51 patients (18.1%) had a systolic blood pressure of > 180 mmHg at admission, and 18 (35.3%) of these patients died within 30 days, which is similar to the 30-day mortality rate of patients with as systolic blood pressure of ≤ 180 mmHg. We believe that this discrepancy might have been due to the different treatments administered for hypertension and different PPH severities. In addition, we consider that systolic hypotension at admission could be explained by rapid brain stem destruction due to the effects of hemorrhage in the pons and those of acute hydrocephalus, both of which could lead to brainstem herniation.
Regarding a history of underlying hypertension, our results and those of Balci et al. (3) suggest that it has no effect on survival in PPH, but Dziewas et al. (1) suggested that underlying hypertension has an effect on survival in PPH. In terms of functional recovery, Wessels et al. (2) and Rabinstein et al. (7) suggested that a history of hypertension has no effect. However, our results and those of Wijdicks et al. (8) suggested that a history of hypertension affected functional recovery.
Considering functional recovery, Dziewas et al. (1) reported a good recovery rate of 25% among 12 survivors, Rabinstein et al. (7) reported a rate of 77% among 36, Wijdicks et al. (8) a rate of 47% among 17, Jung et al. (11) a rate of 54.5% among 22, and Masiyama et al. (21) a rate of 78% among 14 survivors. Our study showed a good recovery rate at 12-month post-PPH of 15.3% among all study subjects and 43.4% among 99 survivors, and this good functional recovery rate concurs with those of other studies. Furthermore, in the present study, we estimated functional recovery using the MRS, but other studies have used the Glasgow Outcome Scale (GOS), which could have caused some functional outcome differences. Rabinstein et al. (7) suggested that cause was a main predictor of outcome in patients with pontine hemorrhage. According to their data, previous histories of hypertension, diabetes mellitus, or stroke, and smoking were not correlated with a poor outcome at 3 months post-PPH. However, their study was performed in patients with PPH or secondary pontine hemorrhage, such as, that caused by a cavernous malformation. In the present study, histories of hypertension and diabetes mellitus were found to be associated with poor functional recovery. Furthermore, the different objectives of studies might be responsible for result differences.
Other variables at admission, such as, a comatose mentality, dilated pupils, abnormal respiration, and systemic hypotension, which are considered to indicate life-threatening conditions, were found to be associated with 30-day mortality. These conditions could be explained by rapid brain stem destruction due to the effects of hemorrhage on the reticular activating system in the upper third of the pontine tegmentum and the effects of acute hydrocephalus. According to the literature, 'a coma on admission' most reliably predicts a poor outcome. In Kushner and Bressman's series (22), all 6 comatose PPH patients at presentation died and the 4 non-comatose patients survived. Masiyama et al. (21) reported 3 survivors among 14 comatose patients, but 11 survivors among 12 non-comatose patients. In a study conducted by Wijdicks et al. (8), 21 patients died, which all patients were comatose at presentation, and among 17 patients who survived, only 4 were comatose at admission; Murata et al. (4) reported 8 survivors among 40 comatose patients at admission, but 34 survivors among 40 non-comatose patients. These numbers are in a line with our own results. Of 182 patients who died during the first year post-PPH, 117 patients were comatose patients, and of the 99 survivors at 1-yr follow-up visits, no patient was comatose on admission.
Although this study was largest of its type conducted to date, its findings are limited by several shortcomings. First, this retrospective study was performed using data obtained at a single institute and was not conducted on a multi-institutional or a national basis, and thus, our results may not accurately represent the national situation. Second, patients with an extremely severe hemorrhage were less likely to have undergone complete evaluation, which would have introduced study bias. Third, it is difficult to conclude that surgical treatment is the more effective treatment modality in PPH patients due to the lack of non-randomization and the selection bias introduce by choosing treatment modalities. Fourth, the means of determining results differed from those used in similar studies, for example, the use of GOS or MRS.
To overcome these limitations, a more comprehensive and comparative study, free of ethical problems is required. Nevertheless, it is hoped that knowledge of the predictors of mortality and functional recovery identified in the present study will improve patient outcomes and individual patient management.
In conclusion, this retrospective single institute-based multivariate analysis of Korean PPH patients suggests that poor initial consciousness, dilated pupils, abnormal respiration, systemic hypotension at admission, hydrocephalus, and conservative treatment independently predict early mortality, and that better consciousness, no limb weakness, no history of previous diabetes or hypertension, no ophthalmoplegia, a small hematoma volume, no intraventricular extension of hemorrhage, and no hydrocephalus more powerfully predict functional recovery than the other variables examined. In particular, it is interesting to find that a systolic blood pressure < 100 mmHg at admission can predict 30-day mortality, and that a history of underlying hypertension or diabetes mellitus can predict 90-day functional recovery by multivariate logistic analysis.
Figures and Tables
Fig. 1
Cumulative mortality curve. The one-year mortality rate was 64.8% and 2-yr mortality rate 72.3%.
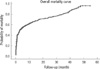
Table 1
Epidemiologic characteristics of patients and univariate analysis of predictors of 30-day mortality and 90-day functional recovery after primary pontine hemorrhage (N = 281)
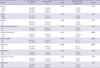
Table 2
Clinical manifestations of patients and univariate analysis of predictors of 30-day mortality and 90-day functional recovery after primary pontine hemorrhage (N = 281)

Table 3
Characteristics of pontine hemorrhage and univariate analysis of predictors of 30-day mortality and 90-day functional recovery after primary pontine hemorrhage (N = 281)

AUTHOR SUMMARY
Predictors of 30-day Mortality and 90-day Functional Recovery after Primary Pontine Hemorrhage
Ji Hwan Jang, Yun Gyu Song, and Young Zoon Kim
The factors related to death and functional recovery after primary pontine hemorrhage (PPH) in Koreans has not been well defined. The authors sought to identify independent predictors of death and functional recovery after PPH using data obtained at a single institute. Data were collected retrospectively on 281 patients with PPH admitted to the Stroke Unit at our hospital between January 1, 2000 and December 31, 2009. One-hundred and ten patients (39.1%) died within 30 days of PPH and 27 patients (9.6%) achieved functional recovery within 90 days. By multivariate analysis, unconsciousness, dilated pupils, abnormal respiration, systolic blood pressure < 100 mmHg, hydrocephalus, and conservative treatment were found to be predictors of 30-day mortality, whereas consciousness, intact motor function, no history of hypertension or diabetes mellitus, intact eye movement, a hematoma volume of < 5 mL, no ventricular hemorrhage, and normally sized ventricle were found to be predictors of 90-day functional recovery. The present findings suggest that systolic hypotension of less than 100 mmHg predicts 30-day mortality, and a history of underlying hypertension and diabetes mellitus predict 90-day functional recovery.
References
1. Dziewas R, Kremer M, Lüdemann P, Nabavi DG, Dräger B, Ringelstein B. The prognostic impact of clinical and CT parameters in patients with pontine hemorrhage. Cerebrovasc Dis. 2003. 16:224–229.
2. Wessels T, Möller-Hartmann W, Noth J, Klötzsch C. CT findings and clinical features as markers for patient outcome in primary pontine hemorrhage. Am J Neuroradiol. 2004. 25:257–260.
3. Balci K, Asil T, Kerimoglu M, Celik Y, Utku U. Clinical and neuroradiological predictors of mortality in patients with primary pontine hemorrhage. Clin Neurol Neurosurg. 2005. 108:36–39.
4. Murata Y, Yamaguchi S, Kajikawa H, Yamamura K, Sumioka S, Nakamura S. Relationship between the clinical manifestations, computed tomographic findings and the outcome in 80 patients with primary pontine hemorrhage. J Neurol Sci. 1999. 167:107–111.
5. Jeong JH, Yoon SJ, Kang SJ, Choi KG, Na DL. Hypertensive pontine microhemorrhage. Stroke. 2002. 33:925–929.
6. Chung CS, Park CH. Primary pontine hemorrhage: a new CT classification. Neurology. 1992. 42:830–834.
7. Rabinstein AA, Tisch SH, McClelland RL, Wijdicks EF. Cause is the main predictor of outcome in patients with pontine hemorrhage. Cerebrovasc Dis. 2004. 17:66–71.
8. Wijdicks EF, St Louis E. Clinical profiles predictive of outcome in pontine hemorrhage. Neurology. 1997. 49:1342–1346.
9. Hara T, Nagata K, Kawamoto S, Sashida J, Abe T, Wada A, Sakamoto T. Functional outcome of primary pontine hemorrhage: conservative treatment or stereotaxic surgery. No Shinkei Geka. 2001. 29:823–829.
10. Hong JT, Choi SJ, Kye DK, Park CK, Lee SW, Kang JK. Surgical outcome of hypertensive pontine hemorrhages: experience of 13 cases. J Korean Neurosurg Soc. 1998. 27:59–65.
11. Jung DS, Jeon BC, Park YS, Oh HS, Chun TS, Kim NK. The predictors of survival and functional outcome in patients with pontine hemorrhage. J Korean Neurosurg Soc. 2007. 41:82–87.
12. Korean Neurological Association. Korean Neurological Association Epidemiology of cerebrovascular disease in Korea: a collaborative study, 1989-1990. J Korean Med Sci. 1993. 8:281–289.
13. Park HS, Kang MJ, Huh JT. Recent epidemiological trends of stroke. J Korean Neurosurg Soc. 2008. 43:16–20.
14. Broderick JP, Adams HP Jr, Barsan W, Feinberg W, Feldmann E, Grotta J, Kase C, Krieger D, Mayberg M, Tilley B, Zabramski JM, Zuccarello M. Guidelines for the management of spontaneous intracerebral hemorrhage: a statement for healthcare professionals from a special writing group of the Stroke Council, American Heart Association. Stroke. 1999. 30:905–915.
15. Ikehara S, Iso H, Toyoshima H, Date C, Yamamoto A, Kikuchi S, Kondo T, Watanabe Y, Koizumi A, Wada Y, Inaba Y, Tamakoshi A. Japan Collaborative Cohort Study Group. Alcohol consumption and mortality from stroke and coronary heart disease among Japanese men and women: the Japan collaborative cohort study. Stroke. 2008. 39:2936–2942.
16. Broderick JP, Brott TG, Duldner JE, Tomsick T, Huster G. Volume of intracerebral hemorrhage. A powerful and easy to use predictor of 30 day mortality. Stroke. 1993. 24:987–993.
17. van Swieten JC, Koudstaal PJ, Visser MC, Schouten HJ, van Gijn J. Interobserver agreement for the assessment of handicap in stroke patients. Stroke. 1988. 19:604–607.
18. Fewel ME, Thompson BG Jr, Hoff JT. Spontaneous intracerebral hemorrhage: a review. Neurosurg Focus. 2003. 15:E1.
19. Manno EM, Atkinson JL, Fulgham JR, Wijdicks EF. Emerging medical and surgical management strategies in the evaluation and treatment of intracerebral hemorrhage. Mayo Clin Proc. 2005. 80:420–433.
20. Han YP, Yoon BS, Hong SK, Hu C, Lee BW, Chang JH, Kim HJ. Treatment of pontine hemorrhage. J Korean Neurosurg Soc. 1985. 14:695–704.
21. Masiyama S, Niizuma H, Suzuki J. Pontine haemorrhage: a clinical analysis of 26 cases. J Neurol Neurosurg Psychiatry. 1985. 48:658–662.
22. Kushner MJ, Bressman SB. The clinical manifestations of pontine hemorrhage. Neurology. 1985. 35:637–643.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download