Abstract
The aim of this study is to describe the clinical characteristics of prepubertal- and adolescent-onset bipolar disorder (BD) and to identify any clinical differences between patients with prepubertal- and adolescent-onset BD. We analyzed the clinical records of 53 inpatients with BD. These patients were divided into prepubertal-onset and adolescent-onset groups. We also divided the subjects into narrow, intermediate, and broad phenotypes according to the definitions proposed by Leibenluft and colleagues. Of the total sample, 16 patients (30.2%) were in the prepubertal-onset group and 37 (69.8%) were in the adolescent-onset group. Patients with prepubertal-onset BD were more likely to display an insidious clinical presentation, atypical features, and comorbid psychopathology. And the majority of the subjects, especially in the prepubertal-onset group, were classified under the intermediate and broad phenotypes. These results suggest that the clinical presentation of BD with prepubertal-onset is different from that of adolescent-onset BD. It is inferred that a significant number of patients with prepubertal- and adolescent-onset BD do not meet DSM-IV criteria for mania or hypomania from the results of this study.
In recent decades, there has been a dramatic increase in recognition of prepubertal- and adolescent-onset bipolar disorder (BD). As there is no clear consensus among experts regarding the clinical presentation of BD, diagnostic symptom criteria, or clinical course in adolescents and children, the diagnosis and treatment of BD in prepubertal and adolescent youth remains a controversial issue. Some investigators have reported that the phenomenology of adolescent mania is similar to that of adult mania (1, 2), while other researchers have reported that adolescent patients display a significantly higher rate of mixed episodes and a significantly lower rate of psychotic features than adult patients (3). The clinical presentation of BD in prepubertal groups has been debated, as well. Previous studies suggest that the presentation of prepubertal BD is atypical when judged by adult standards and that prepubertal BD is different from that of adolescent BD. The atypical features of prepubertal BD, which have been proposed by researchers, are a mixed presentation rather than the classic euphoric, grandiose presentation with an insidious onset and a chronic course (4-7). A research roundtable meeting was convened to discuss the controversial areas in the diagnosis of prepubertal BD at the National Institute of Mental Health (NIMH), Bethesda, MD, USA on April 27, 2000. Experienced clinicians and researchers with expertise on prepubertal BD agreed that the diagnosis of BD in prepubertal populations is possible with currently available psychiatric assessment instruments. Further, in addition to the phenotypes that fit the Diagnostic Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV) (8) criteria for bipolar I disorder, there exists other phenotypes that do not meet the DSM-IV criteria (9). Leibenluft et al. (10) introduced a framework for the classification of juvenile bipolar spectrum disorders into narrow, intermediate, and broad phenotypes. The phenotypic system is based on the DSM-IV episode and duration criteria, as well as the presence or absence of the classic manic symptoms of elevated mood and grandiosity.
Although BD is more common in children than has been acknowledged previously, prepubertal BD remains difficult to diagnose (11-13). Previous studies about the clinical course of early onset BD have reported that children with BD tend to show a chronic course, severe functional impairment, and other psychiatric complications (14-17). Therefore, it is important to identify the age-specific manifestations of BD and to define the diagnostic possibilities for prepubertal and adolescent groups with BD. Early detection and intervention could improve treatments and clinical outcomes during these important life stages.
The aim of our study is to describe the clinical characteristics of prepubertal- and adolescent-onset BD, and to identify any clinical differences between prepubertal- and adolescent-onset groups.
We implemented a retrospective study design. Specifically, all of the patients who had been hospitalized and diagnosed with BD between January 2004 and January 2009 at the Child and Adolescent Psychiatry Service Unit at Samsung Medical Center, Seoul, Republic of Korea were included in the analysis. A total of 53 subjects were identified and diagnosed with bipolar I disorder, bipolar II disorder, or BD NOS based on the DMS-IV diagnostic criteria by experienced child and adolescent psychiatrists. The subjects were divided into two age groups on the basis of recommendations published by a number of authors (7, 18, 19): the prepubertal-onset group (who displayed mood episodes beginning before age 13) and the adolescent-onset group (who displayed mood episodes beginning at or above age 13). We analyzed a range of clinical variables drawn from the medical records of the psychiatrists in charge of the patients. These variables included the age at onset of symptoms of BD, the age at diagnosis, the symptoms in the clinical course, family history, and psychiatric comorbidities. The symptoms at onset, which the subjects had shown dominantly in the initial phase, fell into four categories: irritability and aggressive behavior, depressive symptoms, manic symptoms, and mood swings and fluctuations. The symptoms at the time of hospitalization were divided into four categories based on the DSM-IV episode criteria: mania, hypomania, mixed symptoms, and depression. The treatment before and after the diagnosis of BD were also examined. We reviewed psychological evaluations, including the Korean Educational Development Institute-Wechsler Intelligence Scale for children-III (KEDI-WISC-III) and the Korean Child Behavior Checklist (K-CBCL) (20).
This study was conducted with the approval of the Institutional Review Board at the Samsung Medical Center (IRB file NO 2008.09.068). Informed consent was exempted.
All subjects were classified into narrow, intermediate, and broad phenotypes according to the definitions proposed by Leibenluft et al. The narrow phenotype was assigned to those who met the full DSM-IV diagnostic criteria for mania or hypomania and who also had the hallmark symptoms of elevated mood or grandiosity. The intermediate phenotypes included two subcategories: those individuals with hallmark symptoms of a short duration and those with episodic irritable mania or hypomania that meets the duration criteria, but without elation. The broad phenotype consisted of non-episodic symptoms of severe irritability and hyperarousal, however, this phenotype does not include the hallmark symptoms of elated mood or grandiosity (10).
We assigned 16 patients (30.2%) to the prepubertal-onset group and 37 (69.8%) to the adolescent-onset group. Table 1 shows the mean age at the onset of symptoms of BD, the mean age at initial diagnosis, and the mean age at hospitalization of our sample. The duration between the onset of symptoms and the diagnosis of BD in the prepubertal-onset group was significantly longer than that in the adolescent-onset group (Table 1). There were significant gender differences between the groups, and the majority of the prepubertal-onset group was male. Specifically, 13 (81.2%) of the prepubertal group were male and 18 (48.6%) of the adolescent group were male (P=0.03).
In the prepubertal group, the initial phase of BD was a categorized as a tendency to exhibit irritability and aggressive behavior, while the adolescent group tended to express depressive symptoms. Many of the subjects in the prepubertal and adolescent groups had presented with a mixed episode at the time of admission. There were no differences between the groups with respect to family history of BD or major depressive disorder. In the prepubertal-onset group, the rate of comorbidity was higher than that of the adolescent-onset group and attention-deficit/hyperactivity disorder was the most prevalent comorbid disorder (Table 2).
There were no differences between groups in intelligence scores as assessed by the KEDI-WISC-III. The mean full scale IQ scores for the prepubertal and adolescent groups were 99.36 (SD=25.46) and 90.30 (SD=18.33), respectively. No meaningful differences were detected between the groups in K-CBCL scores. In both groups, all of the K-CBCL clinical subscales other than the somatization subscale were greater than 60, which tends to be predictive of clinically significant psychopathology (Table 3) (21).
In the prepubertal-onset group, only three (18.8%) met the DSM-IV criteria for mania or hypomania, and these three were classified into the narrow phenotype. In the adolescent-onset group, 12 (32.4%) met the DSM-IV criteria for mania or hypomania, and they were classified into the narrow phenotype (Table 4).
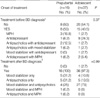
Four subjects (25.0%) from the prepubertal-onset group had been taking methylphenidate and 13 (35.1%) from the adolescent-onset group had been taking antidepressants prior to the diagnosis of BD. After the diagnosis of BD, the most prevalent prescription in the adolescent-onset group was a mood stabilizer with antipsychotics. There was tendency toward monotherapy with either mood stabilizers or antipsychotics in the prepubertal-onset group (Table 5).
These results suggest that prepubertal-onset BD patients tend to show an insidious clinical presentation, atypical features, and more comorbid psychopathology than BD patients with adolescent-onset. We infer that a significant number of patients with prepubertal- and adolescent-onset BD do not meet DSM-IV criteria for mania or hypomania from the results of this study.
Many seriously disturbed children with affective dysregulation and high levels of agitation and aggression present diagnostic and therapeutic challenges to clinicians. Recent research suggests that children with chronic, continuous, severe irritability or prolonged anger outbursts are often diagnosed with BD (22). In our study, the prepubertal sample displayed symptoms, such as marked irritability and aggressive behavior in the year or years prior to receiving a diagnosis of BD. Additionally, the duration between the onset and diagnosis of BD in the prepubertal-onset group was longer than that of the adolescent-onset group. This delay in diagnosis at early ages may be due to the fact that the initial presentation of the prepubertal BD is often not mood symptoms, but rather behavioral problems. Another possible reason for the delayed diagnosis of BD at early ages may be a high frequency of comorbidity. In this study, we found that many patients with prepubertal-onset BD had comorbid externalizing disorders, such as attention-deficit hyperactivity disorder (ADHD) (43.8%), as well as oppositional defiant disorder and conduct disorder (30.8%). Systemic studies show that rates of ADHD range from 60% to 90% in pediatric patients with BD (7, 18). Clinical reports have estimated the rates of conduct disorder in manic children and adolescents with BD to range from 17% to 69% (17, 23). Thus, it may be that the combination of mood changes and disruptive behavior are a specific marker of BD syndrome in young patients (24).
Until now, there have been few studies that have applied the proposed phenotypes of juvenile BD (10) to clinical subjects. When we applied this criteria to the patients examined in this study, the majority of the subjects, especially in the prepubertal-onset group, were classified under the intermediate and broad phenotypes, which did not meet the DSM-IV criteria for either mania or hypomania. The results of the present study correspond with a previous study that reported only approximately 50% of child and adolescent bipolar patients met DSM-IV criteria (4). In this study, 37% of the prepubertal group and 32% of the adolescent group was classified as the broad phenotype. Since the broad phenotype consists of non-episodic symptoms of severe irritability without elated mood or grandiosity, it is easy to confuse the broad phenotype with childhood externalizing disorders. This phenotypic system can help clinicians develop a more clear phenotypic description of prepubertal and adolescent BD and to re-evaluate young patients who do not meet the DSM-IV criteria for mania, but who do have mood symptoms, behavioral changes, and functional impairment. Longitudinal studies that examine the clinical course of the broad phenotype are warranted in order to find out whether this categorization represents a homogenous subgroup of bipolar spectrum disorder.
Early detection of BD and recognition of comorbid disorders is very important for determining the appropriate types and sequences of treatments. In our study, four (25.0%) of the prepubertal-onset group had been taking methylphenidate, and 13 (35.1%) of the adolescent-onset group had been taking antidepressants prior to the diagnosis of BD. Stimulant use to target ADHD symptoms in bipolar patients can be problematic because of its potential to precipitate or exacerbate mood-related symptoms (25). Additionally, previous work has suggested that there is concern that antidepressants can worsen the clinical course of bipolar illness (26).
The CBCL is one of the best-studied, empirically derived, checklists available to examine childhood psychopathology (27). Recently it has been shown that the CBCL is useful in distinguishing BD from ADHD. Additionally, children with BD typically have high scaled scores in the Aggression, Attention Problems, Delinquency, Thought Problems, and Anxious/Depressed subscales of the CBCL (28, 29). Although we failed to find any differences in K-CBCL subscales between groups, the results of this study support the previous studies. It is important to consider a diagnosis of BD when assessing children with high scores on these CBCL subscales even when they do not fit any of DSM-IV diagnostic criteria.
This retrospective study has some limitations, such as the lack of structured or semi-structured interviews for diagnosis. In this study, however, we evaluated the clinical features of the subjects intensively in the inpatient clinic for a month or months. A minimum of two psychiatrists and a psychologist participated in the diagnosis of the subjects. Additionally, it is known that clinical assessment and structured interview are highly consistent with each other (30). We divided the subjects into prepubertal- and adolescent onset BD according to the age. In order to define the prepubertal phase, it is required to examine the secondary sex characteristics of the subjects. The biological marker, such as Tanner stage could be used in the following study. In the results of research examining the clinical presentation of BD, it has been demonstrated that it is ideal to evaluate patients with BD who do not have any other psychiatric disorders. Nonetheless, the examination of pure bipolar patients in prepubertal and adolescent populations is complicated due to the high rates of comorbidity common among individuals with BD. Further research must be conducted to separate the effects of comorbid psychiatric disorders on the clinical course of BD in young patients.
BD in prepubertal and adolescent populations is a serious, recurrent, and debilitating psychiatric concern. Too often BD is not considered as a possible diagnosis in children, and delayed diagnosis may have negative effects on the clinical course and prognosis for children. Alternative diagnostic criteria and assessment instruments for prepubertal and adolescent BD need to be developed.
Figures and Tables
Table 2
Clinical characteristics in prepubertal and adolescent-onset bipolar disorder

*by chi-square test.
BD, Bipolar affective disorder; MD, Major depression; ADHD, Attention-deficit/hyperactivity disorder; ODD, Oppositional defiant disorder; CD, Conduct disorder; PDD, Pervasive developmental disorder; PDDNOS, Pervasive developmental disorder, not otherwise specified; MR, Mental retardation; BIF, Borderline interllectual functioning.
Table 3
Comparison of T Scores for CBCL Subscales in prepubertal and adolescent-onset bipolar disorder

References
1. Coryell W, Norten SG. Mania during adolescence. The pathoplastic significance of age. J Nerv Ment Dis. 1980. 168:611–613.
2. Hsu LK, Starzynski JM. Mania in adolescence. J Clin Psychiatry. 1986. 47:596–599.
3. McElroy SL, Strakowski SM, West SA, Keck PE Jr, McConville BJ. Phenomenology of adolescent and adult mania in hospitalized patients with bipolar disorder. Am J Psychiatry. 1997. 154:44–49.
4. Faedda GL, Baldessarini RJ, Glovinsky IP, Austin NB. Pediatric bipolar disorder: phenomenology and course of illness. Bipolar Disord. 2004. 6:305–313.
5. Findling RL, Gracious BL, McNamara NK, Youngstrom EA, Demeter CA, Branicky LA, Calabrese JR. Rapid, continuous cycling and psychiatric co-morbidity in pediatric bipolar I disorder. Bipolar Disord. 2001. 3:202–210.
6. Geller B, Tillman R. Prepubertal and early adolescent bipolar I disorder: review of diagnostic validation by Robins and Guze criteria. J Clin Psychiatry. 2005. 66:Suppl 7. 21–28.
7. Wozniak J, Biederman J, Kiely K, Ablon JS, Faraone SV, Mundy E, Mennin D. Mania-like symptoms suggestive of childhood-onset bipolar disorder in clinically referred children. J Am Acad Child Adolesc Psychiatry. 1995. 34:867–876.
8. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 1994. 4th ed. Washington DC: American Psychiatric Press.
9. NIMH. National Institute of Mental Health research roundtable on prepubertal bipolar disorder. J Am Acad Child Adolesc Psychiatry. 2001. 40:871–878.
10. Leibenluft E, Charney DS, Towbin KE, Bhangoo RK, Pine DS. Defining clinical phenotypes of juvenile mania. Am J Psychiatry. 2003. 160:430–437.
11. Warneke L. A case of manic-depressive illness in childhood. Can Psychiatr Assoc J. 1975. 20:195–200.
12. Weinberg WA, Brumback RA. Mania in childhood: case studies and literature review. Am J Dis Child. 1976. 130:380–385.
13. Weller RA, Weller EB, Tucker SG, Fristad MA. Mania in prepubertal children: has it been underdiagnosed? J Affect Disord. 1986. 11:151–154.
14. Biederman J, Mick E, Faraone SV, Van Patten S, Burback M, Wozniak J. A prospective follow-up study of pediatric bipolar disorder in boys with attention-deficit/hyperactivity disorder. J Affect Disord. 2004. 82:Suppl 1. S17–S23.
15. Birmaher B, Axelson D, Strober M, Gill MK, Valeri S, Chiappetta L, Ryan N, Leonard H, Hunt J, Iyengar S, Keller M. Clinical course of children and adolescents with bipolar spectrum disorders. Arch Gen Psychiatry. 2006. 63:175–183.
16. Jairam R, Srinath S, Girimaji SC, Seshadri SP. A prospective 4-5 yr follow-up of juvenile onset bipolar disorder. Bipolar Disord. 2004. 6:386–394.
17. Jolin EM, Weller EB, Weller RA. Prepubertal bipolar disorder: proper diagnosis should lead to better treatment response. Curr Psychiatry Rep. 2005. 7:104–111.
18. Geller B, Sun K, Zimerman B, Luby J, Frazier J, Williams M. Complex and rapid-cycling in bipolar children and adolescents: a preliminary study. J Affect Disord. 1995. 34:259–268.
19. Lazaro L, Castro-Fornieles J, de la Fuente JE, Baeza I, Morer A, Pamias M. Differences between prepubertal-versus adolescent-onset bipolar disorder in a Spanish clinical sample. Eur Child Adolesc Psychiatry. 2007. 16:510–516.
20. Oh KJ, Lee HR. Development of Korean version of Child Behavior Checklist (K-CBCL). Korean Research Foundation Report. 1990. Seoul:
21. Chen WJ, Faraone SV, Biederman J, Tsuang MT. Diagnostic accuracy of the Child Behavior Checklist scales for attention-deficit hyperactivity disorder: a receiver-operating characteristic analysis. J Consult Clin Psychol. 1994. 62:1017–1025.
22. Carlson GA, Bromet EJ, Sievers S. Phenomenology and outcome of subjects with early- and adult-onset psychotic mania. Am J Psychiatry. 2000. 157:213–219.
23. Kovacs M, Pollock M. Bipolar disorder and comorbid conduct disorder in childhood and adolescence. J Am Acad Child Adolesc Psychiatry. 1995. 34:715–723.
24. Carlson GA. Identifying prepubertal mania. J Am Acad Child Adolesc Psychiatry. 1995. 34:750–753.
25. Koehler-Troy C, Strober M, Malenbaum R. Methylphenidate-induced mania in a prepubertal child. J Clin Psychiatry. 1986. 47:566–567.
26. Baumer FM, Howe M, Gallelli K, Simeonova DI, Hallmayer J, Chang KD. A pilot study of antidepressant-induced mania in pediatric bipolar disorder: characteristics, risk factors, and the serotonin transporter gene. Biol Psychiatry. 2006. 60:1005–1012.
27. Achenbach TM, Dumenci L. Advances in empirically based assessment: revised cross-informant syndromes and new DSM-oriented scales for the CBCL, YSR, and TRF: comment on Lengua, Sadowksi, Friedrich, and Fischer (2001). J Consult Clin Psychol. 2001. 69:699–702.
28. Biederman J, Wozniak J, Kiely K, Ablon S, Faraone S, Mick E, Mundy E, Kraus I. CBCL clinical scales discriminate prepubertal children with structured interview-derived diagnosis of mania from those with ADHD. J Am Acad Child Adolesc Psychiatry. 1995. 34:464–471.
29. Mick E, Biederman J, Pandina G, Faraone SV. A preliminary meta-analysis of the child behavior checklist in pediatric bipolar disorder. Biol Psychiatry. 2003. 53:1021–1027.
30. Wozniak J, Monuteaux M, Richards J, E Lail K, Faraone SV, Biederman J. Convergence between structured diagnostic interviews and clinical assessment on the diagnosis of pediatric-onset mania. Biol Psychiatry. 2003. 53:938–944.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download