Abstract
This study investigated the safety and effectiveness of each type of central venous catheters (CVC) in patients with cancer. We prospectively enrolled patients with cancer who underwent catherization involving a subclavian venous catheter (SVC), peripherally inserted central venous catheter (PICC), or chemo-port (CP) in our department. From March 2007 to March 2009, 116 patients underwent 179 episodes of catherization. A SVC was inserted most frequently (46.4%). Fifty-four complications occurred (30.1%): infection in 23 cases, malpositioning or migration of the tip in 18 cases, thrombosis in eight cases, and bleeding in five cases. Malpositioning or migration of the tip occurred more frequently with a PICC (P<0.001); infection occurred more often with a tunneled catheter (P=0.028) and was observed more often in young patients (P=0.023). The catheter life span was longer for patients with solid cancer (P=0.002) than for those with hematologic cancer, with a CP (P<0.001) than a PICC or SVC, and for an indwelling catheter with image guidance (P=0.014) than a blind procedure. In conclusion, CP is an effective tool for long term use and the fixation of tip is important for the management of PICC.
The development of increasingly complex treatment regimens for patients with advanced malignancies has led to a greater reliance on a variety of intravenous delivery systems. Patients who have cancer usually require repeated venous punctures for treatment monitoring, application of chemotherapy, or blood transfusions. Therefore, central venous catheters (CVCs) and implantable port systems have substantially facilitated the problem of vascular access. However, CVCs have inevitable problems such as insertion-related and long-term complications despite providing benefits to patients. The incidence of CVC-related complications is relatively high based on data from a study commissioned by the Food and Drug Administration in the 1990s, which showed a 10-25% complication rate and 10% morbidity (1). Insertion-related complications have dramatically decreased since the use of ultrasound guidance (USG), although one report described negative effects of USG (2). Major complications related to CVCs include infection and thrombosis (3, 4). Various management strategies have been recommended to prevent and treat infection and thrombosis (5), and CVC outcomes have improved considerably. Along with improvements in insertion technique and CVC management, improvements have been made in catheter design and materials, which have contributed to reducing CVC-related complications. To date, reports have dealt with the management guidelines for CVCs in patients with cancer (5-7), but institutional catheter implantation and maintenance guidelines tend to vary substantially. Furthermore, various kinds of catheters are available, each with its own strengths and weakness. Physicians must consider various factors such as catheter duration, technique, compliance, complications, cost, and efficacy to decide which catheter is best for optimal access to each patient. However, no evidence-based guide has been established to select the most appropriate vascular access device for each clinical situation, notwithstanding the broad range of vascular access devices available. In Korea, there were few studies for the subtype of CVCs (8, 9); however there was no report for the prospectively comprehensive study of CVCs in cancer patients. Therefore, we conducted this study prospectively to investigate the safety, efficacy, and complication rate of the various kinds of CVCs in patients with cancer, to provide the guidance for the central venous catheterization in cancer patients.
We prospectively enrolled cancer patients who were admitted to our department, and underwent catheterization for various purposes. The CVCs included a subclavian venous catheter (SVC), a peripherally inserted central venous catheter (PICC), or a chemoport (CP). The CVCs were categorized as tunneled catheters, CPs, and non-tunneled catheters, SVCs and PICCs, and the physician determined which CVC was appropriate. Indwelling of the catheter was performed by an expert interventional radiologist with radiological guidance, or it was performed at bedside with a blind approach. All operators wore aseptic gowns, masks, gloves, and all patients received a dressing with aseptic drapes. The SVCs had double or triple lumens and were permitted only for hospitalized patients. The PICC was inserted through the antecubital, basilic, brachial, or cephalic vein with USG and was used for both inpatients and outpatients. The PICC usually had a single lumen (5 Fr) and was made of silicone or second-/third-generation polyurethane. The CP was a totally implanted port, had Dacron anchoring cuffs with a reservoir and a single lumen, and was used for both inpatients and outpatients. CP insertion was performed by an expert interventional radiologist in the angiography room with fluoroscopic guidance.
No patient was given prophylactic antibiotics or anticoagulation drugs for infection or thrombosis. All patients received a closed dressing with Betadine on the catheter insertion site every 3 days. A saline flush (once daily) or heparin flush (once weekly, 10 mL) was performed for the hospitalized patients. Patients who had completed scheduled therapy with a CP received a heparin flush every 3 months.
We checked for any immediate- and late-onset complications. A catheter-related infection occurred when an infection was documented from a catheter tip culture or when a differential quantitative blood culture indicated the differential time to positivity (DTTP). We removed the central catheter when we detected a complicated catheter infection, such as a fungal or Gram-negative infection; however, we used salvage therapy, such as antibiotic locking therapy, for uncomplicated infections with tunneled catheters. All patients with catheter-related infections were administered systemic antibiotics for at least 2 weeks, either intravenously or orally. Catheter-related thrombosis was suspected when the flow rate slowed or it was impossible to backflush the catheter, and a confirmational study was conducted using Doppler USG or venography. However, all patients who had thrombosis symptoms, with or without a confirming test, were included as having thrombotic complications. When we suspected a catheter thrombus, we injected 5,000 IU of heparin or urokinase into the catheter. If this failed, we removed the catheter.
The primary endpoint was the complication rate. The secondary endpoints were catheter life span, catheter maintenance success rate, and factors affecting complications or the catheter life span. The catheter life span was calculated from the insertion date to the removal date and was assessed using the Kaplan-Meier method. The catheter maintenance success rate was defined by patients who maintained their catheters for the duration of the intended purpose such as the completion of therapy, discharge, or death. We used the chi-square test for categorical variables and the independent t-test for continuous variables to analyze the patient characteristics. To analyze the factors affecting the complication rate, we used the chi-square test or Fisher's exact test with a cross analysis. To analyze the factors affecting catheter life span, we used the Kaplan-Meier method and log-rank test for the univariate analysis and the Cox's proportional hazard regression model for the multivariate analysis. All tests were two-sided.
This study was approved by the Institutional Review Board of Soonchunhyang University Bucheon Hospital (Approval No. 07-42). After the protocol was approved, written informed consent was obtained from all patients before the entry of the study. All data collected from this study were kept confidential.
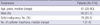
From March 2007 to March 2009, 116 patients underwent 179 catherization episodes. The median age was 61 yr (range, 20-80 yr). The median follow-up duration was 344 days (range, 64-767 days). The male to female ratio was 60:56, and 76 patients had solid malignancies, while 40 patients had hematologic malignancies. The median number of catheter insertions per patient was one (range, 1-4). A SVC was inserted most frequently (83 cases, 46.4%), followed by a CP (72 cases, 40.2%) and a PICC (24 cases, 13.4%). Most catheter insertions (170 cases, 95.0%) were performed in the angiography room with USG or fluoroscopic guidance. Blood product transfusion occurred in 136 cases (76.0%) and total parenteral nutrition (TPN) in 85 cases (47.5%) (Tables 1, 2).
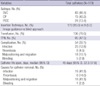
Fifty-four complications (30.1%) occurred in the 179 catheterization episodes. The most frequently documented complication was infection in 23 cases (12.8%), followed by malpositioning or migration of the tip in 18 cases (10.1%), thrombosis in eight cases (4.5%), and minor or major bleeding at the insertion site in five cases (2.8%). SVCs had significantly fewer complications than PICCs or CPs (18.1% vs 50% vs 34.7%). The incidence of infection was not different among disease type, gender, procedure technique (image guidance vs blind approach), transfusion, or TPN. However, infection occurred more in CPs than SVCs or PICCs (P=0.028). Additionally, an infection occurred more frequently in younger patients than older patients (P=0.023). Malpositioning or migration of the tip occurred more frequently with a PICC (P<0.001) than a SVC or a CP (33.3% vs 7.2% vs 5.6%). The incidence of thrombosis or bleeding was not different among gender, disease type, catheter type, procedural technique (image guidance vs blind approach), transfusion, or TPN (Table 3).
The catheter maintenance success rate was evaluable in 123 cases. The others were not due to a failure to complete therapy (38 cases), transfer to another hospital (15 cases), or not applicable (3 cases). Catheter maintenance was successful in 79 cases (64.2%) and removal of the catheter before the intended time (therapy completion, discharge, or death) occurred in 44 cases (35.8%). The catheter maintenance success rate was 72.7%. Infection (41.9%) or migration of the tip occurred in 41.9% of cases, followed by thrombosis in six cases and bleeding in one case.
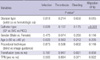
The median catheter life span was 45 days (95% confidence interval [CI], 32.3-57.6). The catheter life span was longer in patients with solid cancer (median days, 64 vs 32, P=0.002) than those with hematologic cancer. Furthermore, life span was longer for CPs (269 vs 37 vs 21 days, P<0.001) than PICCs or SVCs, and for indwelling catheters inserted with image guidance (45 vs 14 days, P=0.014) rather than a blind procedure. The multivariate analysis revealed that solid cancer and CP were significant factors for catheter life span compared to hematologic cancer or other catheter types. However, catheter life span was not different among gender, age (<60 vs ≥60 yr), or transfusion (Table 4, Fig. 1).
CVCs have a paramount role throughout the management of an oncology patient, as they are needed in the initial phases for surgery or chemotherapy, in the advanced stage for chronic treatment, and in the last stage for palliative measures. The insertion of a CVC may be the initial therapeutic step in some patients who have advanced cancer. Physicians must determine the individualized catheter type by considering various factors such as catheter duration, technique, compliance, complications, cost, and efficacy. CVCs are classified by tip position, technical features, or materials. They can be classified in terms of short-term, medium-term, or long-term access. Because SVCs are a non-tunneled catheter, the expected duration was generally short, and they have a known disadvantage of infection. The PICC is also a non-tunneled catheter and is useful for a relatively longer duration. The CP is a tunneled catheter and is useful for the long term. Tunneled catheters and PICCs (1, 10) are held to have lower infection rates, but no randomized controlled trials have demonstrated this contention to date (11). Additionally, thrombosis occurs more often with a PICC than other catheters due to the influence of multifactorial phenomena (12).
Based on these previous results and recommendations, we chose a particular type of catheter for each patient. However, some results differed from previous studies regarding the complication rate and catheter life span. Catheter-related infection occurred in 12.8%, was observed more in CPs than others, and was not significantly related with disease type, gender, procedural technique, transfusion, or TPN. The CP is a totally implanted tunnel catheter and requires needling through a subcutaneous tract, which presents the risk for a skin floral infection, especially in immunocompromised patients. CPs were used in patients with a solid malignancy, including those who experienced prolonged chemotherapy-related neutropenia and in patients with a hematologic malignancy. This trend may affect the CP-related high risk of infection due to the increased incidence of neutropenia in patients with a CP (13, 14). Furthermore, we found that a catheter-related infection was more frequent in young patients than in the elderly, which is consistent with the report of Samaras et al. (15). In the study, young patients had more hematologic cancer than solid cancer, and hematologic cancer was a risk factor for infection. However, the type of disease was not a significant factor for infection in our results, and no relationship was observed between age and disease type. Therefore, we cannot explain why age was a risk factor for infection, but we suggest that young patients may have received more intensive therapy than elders, and this factor may have contributed to the increased infection risk and increased incidence of neutropenia. In five cases, CVC-related infections were treatable with systemic antimicrobials and antibiotic locking therapy without removing the catheter; however, most (18 cases, 78%) resulted in catheter removal. Therefore, to maintain a long-duration CP, we should consider factors such as expected prolonged neutropenia or age and the need for more careful nursing, especially for needling. Further study is warranted for preventive strategies such as skin antisepsis, maximum sterile barriers, use of antimicrobial catheters, and antimicrobial catheter lock solutions (16, 17).
The incidence of thrombosis was 4.5% in our study, which was relatively low despite not using prophylactic anticoagulation. Of course, this may be an underestimate because asymptomatic patients were excluded. Debate about prophylactic anticoagulation has been ongoing. Prophylactic low-dose warfarin (1 mg/d) (18) and low-molecular-weight heparin (19) reduced the incidence of CVC-associated thrombosis in patients with cancer in randomized controlled trials. Since then, conflicting data have been reported for prophylactic anticoagulation from randomized controlled trials (20, 21). More recently, a negative report on warfarin thrombopropylaxis was published (22); therefore, a confirmative study for prophylaxis of thrombotic complications is required. When a thrombotic occlusion of a CVC occurs, anticoagulation therapy is occasionally available as a salvage therapy instead of catheter removal (23, 24). In our study, two cases with thrombotic occlusion were resolved through anticoagulation therapy (urokinase or heparin flushing) without removing the catheter. The thrombosis incidence rate tended to be more frequent (12.5%, 3 cases) in patients with PICCs than CPs or SVCs, but it was not a significant difference, which may have been due to the small number of patients enrolled. This trend may have resulted from the small lumen of the PICC (25); therefore, we should avoid the use of small lumen PICCs.
Unexpectedly, catheter tip migration was a more frequent complication in PICCs (8 cases, 33.3%) than in SVCs or CPs, which resulted in a decreased PICC life span (median life span, 37 days). The PICCs were inserted mid-arm with USG in both hospitalized patients and outpatients in our study. The mid-arm insertion site may have resulted in tip migration with arm motion; therefore, PICCs should be fixed well and patients, especially outpatients, need to be educated (26, 27).
We found no catheter-related immediate-onset complications, such as a hemothorax or pneumothorax, excluding bleeding. Most cases were performed by an expert interventional radiologist using USG or fluoroscopic guidance, which may have resulted in this finding. Although, a study has reported that USG is not beneficial for reducing catheter-related complication (2), the finding that we had no catheter-related immediate-onset complications, excluding minor bleeding, supports the use of an image-guided procedure. Therefore, it is optimal to insert catheters using USG or fluoroscopic guidance rather than a blind approach to reduce the immediate-onset complication rate. However, bleeding is possible in patients with coagulopathy, which needs to be prevented.
The median catheter life span was 46 days, and the CP was useful for the long term (median 269 days); however, the median life span of the PICC was 37 days, which was shorter than expected. A high complication rate, especially tip migration, may have contributed to this finding. Additionally, a longer-term use of catheters occurred in patients with a solid malignancy than hematologic malignancy. Patients with a solid malignancy underwent a CP rather than another catheter type due to scheduled, intermittent long-term chemotherapy. Therefore, the CP was considered an effective tool for long-term use in patients with cancer.
Some limitations were imposed, including the small number of patients; the study was non-randomized and observational, and permitted repeated indwelling in the same patient. However, the main findings were that the major catheter-related complication was infection, which occurred more frequently in young patients or those who received a CP; immediate CVC-related complications were very rare; and malpositioning or migration of the catheter tip was more frequent with a PICC than the others and this contributed to the finding that a PICC could not be maintained for a long duration.
In conclusion, the major problems related to CVCs were infection, thrombosis, and malpositioning or migration of the tip. Unexpectedly, a PICC could not be maintained for a long duration, due mainly to malpositioning or migration. Although the use of CPs resulted in a higher infection rate than the others, a CP was an effective tool for long-term use in patients with cancer. In addition, the insertion of CVCs with the image guidance is beneficial and the fixation of tip is important for the management of PICC. However the best choice of catheter type is essential for each patient. A further prospective randomized study with central catheters in patients with cancer to investigate the complication rate and safety of CVCs is warranted.
Figures and Tables
References
1. Scott WL. Central venous catheters. An overview of Food and Drug Administration activities. Surg Oncol Clin N Am. 1995. 4:377–393.
2. Mansfield PF, Hohn DC, Fornage BD, Gregurich MA, Ota DM. Complications and failures of subclavian-vein catheterization. N Engl J Med. 1994. 331:1735–1738.

3. Yildizeli B, Laçin T, Batirel HF, Yüksel M. Complications and management of long-term central venous access catheters and ports. J Vasc Access. 2004. 5:174–178.

4. Cortelezzia A, Fracchiolla NS, Maisonneuve P, Moia M, Luchesini C, Ranzi ML, Monni P, Pasquini MC, Lambertenghi-Deliliers G. Central venous catheter-related complications in patients with hematological malignancies: a retrospective analysis of risk factors and prophylactic measures. Leuk Lymphoma. 2003. 44:1495–1501.
5. McGee DC, Gould MK. Preventing complications of central venous catheterization. N Engl J Med. 2003. 348:1123–1133.

6. Vescia S, Baumgärtner AK, Jacobs VR, Kiechle-Bahat M, Rody A, Loibl S, Harbeck N. Management of venous port systems in oncology: a review of current evidence. Ann Oncol. 2008. 19:9–15.

7. Gallieni M, Pittiruti M, Biffi R. Vascular access in oncology patients. CA Cancer J Clin. 2008. 58:323–346.

8. Kim JT, Oh TY. Clinical review of totally implantable venous catheter. Korean J Thorac Cardiovasc Surg. 2007. 40:691–695.
9. Cho SG, Kim SH, Song HH, Song SH, Lee KH, Chung DY, Lee HJ, Kim SH, Kim KT, Kim CC. Radiologic placement of subcutaneous infusion ports in cancer patients: analysis of 45 cases. J Korean Cancer Assoc. 2000. 32:1115–1121.
11. Pratt RJ, Pellowe CM, Wilson JA, Loveday HP, Harper PJ, Jones SR, Mc-Dougall C, Wilcox MH. epic2: National evidence-based guidelines for preventing healthcare-associated infections in NHS hospitals in England. J Hosp Infect. 2007. 65:Suppl 1. S1–S64.

12. King MM, Rasnake MS, Rodriguez RG, Riley NJ, Stamm JA. Peripherally inserted central venous catheter-associated thrombosis: retrospective analysis of clinical risk factors in adult patients. South Med J. 2006. 99:1073–1077.

13. Howell PB, Walters PE, Donowitz GR, Farr BM. Risk factors for infection of adult patients with cancer who have tunnelled central venous catheters. Cancer. 1995. 75:1367–1375.

14. Bodey GP, Buckley M, Sathe YS, Freireich EJ. Quantitative relationships between circulating leukocytes and infection in patients with acute leukemia. Ann Intern Med. 1966. 64:328–340.

15. Samaras P, Dold S, Braun J, Kestenholz P, Breitenstein S, Imhof A, Renner C, Stenner-Liewen F, Pestalozzi BC. Infectious port complications are more frequent in younger patients with hematologic malignancies than in solid tumor patients. Oncology. 2008. 74:237–244.

16. Camargo LF, Marra AR, Büchele GL, Sogayar AM, Cal RG, de Sousa JM, Silva E, Knobel E, Edmond MB. Double-lumen central venous catheters impregnated with chlorhexidine and silver sulfadiazine to prevent catheter colonisation in the intensive care unit setting: a prospective randomised study. J Hosp Infect. 2009. 72:227–233.

17. Lee DH, Jung KY, Choi YH. Use of maximal sterile barrier precautions and/or antimicrobial-coated catheters to reduce the risk of central venous catheter-related bloodstream infection. Infect Control Hosp Epidemiol. 2008. 29:947–950.

18. Bern MM, Lokich JJ, Wallach SR, Bothe A Jr, Benotti PN, Arkin CF, Greco FA, Huberman M, Moore C. Very low doses of warfarin can prevent thrombosis in central venous catheters. A randomized prospective trial. Ann Intern Med. 1990. 112:423–428.
19. Monreal M, Alastrue A, Rull M, Mira X, Muxart J, Rosell R, Abad A. Upper extremity deep venous thrombosis in cancer patients with venous access devices prophylaxis with a low molecular weight heparin (Fragmin). Thromb Haemost. 1996. 75:251–253.
20. Couban S, Goodyear M, Burnell M, Dolan S, Wasi P, Barnes D, Macleod D, Burton E, Andreou P, Anderson DR. Randomized Placebo-Controlled Study of Low-Dose Warfarin for the Prevention of Central Venous Catheter-Associated Thrombosis in Patients With Cancer. J Clin Oncol. 2005. 23:4063–4069.

21. Heaton DC, Han DY, Inder A. Minidose (1 mg) warfarin as prophylaxis for central vein catheter thrombosis. Intern Med J. 2002. 32:84–88.

22. Young AM, Billingham LJ, Begum G, Kerr DJ, Hughes AI, Rea DW, Shepherd S, Stanley A, Sweeney A, Wilde J, Wheatley K. WARP Collaborative Group, UK. Warfarin thromboprophylaxis in cancer patients with central venous catheters (WARP): an open-label randomised trial. Lancet. 2009. 373:567–574.

23. Svoboda P, Barton RP, Barbarash OL, Butylin AA, Jacobs BR, Lata J, Haire WD, Jaff MR, Firszt CM, Mouginis TL, Schuerr DM, Schulz GA, Schwartz LB, El-Shahawy MA. Recombinant urokinase is safe and effective in restoring patency to occluded central venous access devices: a multiple-center, international trial. Crit Care Med. 2004. 32:1990–1996.

24. Schindler J, Bona RD, Chen HH, Feingold JM, Edwards RL, Tutschka PJ, Bilgrami S. Regional thrombolysis with urokinase for central venous catheter-related thrombosis in patients undergoing high-dose chemotherapy with autologous blood stem cell rescue. Clin Appl Thromb Hemost. 1999. 5:25–29.

25. Grove JR, Pevec WC. Venous thrombosis related to peripherally inserted central catheters. J Vasc Interv Radiol. 2000. 11:837–840.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download