Abstract
Transvenous left ventricular (LV) lead implantation is on the increase due to cardiac resynchronization therapy (CRT). However, there has been paucity of data on the prognosis of LV lead. Consecutive 32 patients with LV lead for CRT (n=22) or pacemaker (n=10) were subjected. Serial changes in pacing threshold and impedance along with lead-related complications were evaluated. Over 2 yr follow-up, there was no significant change in relative threshold voltage to the initial value (100%, 110%, 89.6%, and 79.6% at baseline, 1, 6, and 24 months respectively, P=0.62) as well as lead impedance (816±272, 650±178, 647±191, and 590±185 ohm at baseline, 1, 6, and 24 months respectively, P=0.80). The threshold change was not affected by lead position, lead polarity, and indication of lead implantation. The cumulative rates of lead revision were 6.3% (n=2) and 9.4% (n=3) in 6 month and 2 yr follow-up, respectively. One case of phrenic nerve capture at left lateral decubitus position was detected 1 month after the implantation. However, there were no serious complications over 2 yr period. In conclusion, transvenous LV lead implantation showed favorable long-term prognosis. Pacing parameters remained stable without significant changes over 2 yr follow-up.
Transvenous left ventricular (LV) lead implantations have occasionally been used when permanent cardiac pacing is needed for those whom endocardial right ventricular (RV) pacing is contraindicated by the presence of a tricuspid valve (TV) prosthesis (1, 2). Cardiac resynchronization therapy (CRT) has been demonstrated to be beneficial for selected patients with advanced heart failure through several randomized trials. Thereafter, number of implantation cases has been increased worldwide (3-5). Therefore, information on the efficacy and safety of LV leads is becoming much more necessary than ever. There has been paucity of data, however, on the prognosis of transvenous LV leads after their implantation (6). The aim of this study was to evaluate the long-term performance of LV leads implanted into cardiac veins and their related complications.
From November 1996 to December 2008, consecutive 32 patients (M:F=14:19, 59.4±12.3 yr) who underwent transvenous LV lead implantation at Seoul National University Hospital and Asan Medical Center, were enrolled. All the patients underwent the procedure either for CRT (n=22) as an adjunctive therapy of severe LV dysfunction (New York Heart Association functional class III or IV heart failure despite optimal medical treatment), or for permanent pacemaker (PM, n=10) due to complete atrioventricular block (CAVB) or sinus node dysfunction. The study was approved by the hospital ethics committee (IRB No. H-1003-054-313).
Leads utilized in our study were Attain Unipolar OTW leads (model 4193, St. Paul, MN, USA), Attain Bipolar OTW leads (model 4194, Medtronic), Attain 2187 leads (Medtronic), and QuickSite leads (model 1506T, St. Jude Medical, Sylmar, CA, USA).
All implantation procedures were done in cardiac electrophysiology laboratory under conscious sedation with local anesthesia. Axillary or subclavian vein was punctured for the transvenous deployment of a specialized lead delivery system into the cardiac veins. To facilitate the LV lead insertion into the target sites, cardiac venograms in multiple fluoroscopic projections were acquired. If the pacing threshold in a coronary vein was considered too high (>5 V at 0.4 ms), deployment into another branch was tried. When the values of LV pacing threshold, R-wave sensing, and lead impedance were acceptable, the lead was connected to a pulse generator.
To assess the LV leads performance, serial changes in pacing threshold and impedance were analyzed at the time of implantation, 1, 6, 12, and 24 months after the index procedure. Threshold test was performed at 0.4 ms pulse width, and relative threshold voltages to the initial value (%) were obtained at each follow-up time point.
Continuous variables were presented as mean±standard deviation and were compared using non-parametric Mann-Whitney test. The results for categorical variables were described as percentages, and the Fisher's exact test was used to compare them when appropriate. Differences in pacing parameters at each follow-up period were tested by analysis of variance (ANOVA) and followed by a Scheffe's post-hoc test. All statistical analyses were performed using SPSS software, version 17 (SPSS Inc., Chicago, IL, USA), and P values of <0.05 were considered statistically significant.
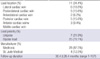
Baseline clinical characteristics of the patients who underwent transvenous LV lead implantation (n=32) are summarized in Table 1. Patients with ischemic cardiomyopathy accounted for about 16% of total population whereas non-ischemic cardiomyopathy did 84%. The LV ejection fraction (EF) of CRT group and PM group were 23±8% and 55±8%, respectively. All patients in the PM group (n=10) had TV prosthesis, which composed of 4 cases of mechanical valves and 6 cases of tissue valves (Fig. 1). They had already experienced multiple open heart surgery (OHS) prior to PM insertion with mean number of OHS and of replaced valve were 2.4±0.8 and 2.5±0.5 respectively.
Table 2 shows baseline LV lead characteristics. Seven unipolar (22%) and 25 bipolar leads (78%) were used for the patients enrolled in the present study. Final deployment sites were as follows; 11 in the lateral, 6 in posterolateral, 5 in anterolateral, 2 in posterior, 5 in anterior, and 3 in middle cardiac vein respectively.
Follow-up period was 30.4±26.4 months (1-107 months). As shown in Fig. 2, the serial values of pacing parameters of LV leads remained stable without significant changes during the follow-up period. Relative threshold voltage to the baseline value (%) at each follow-up point were 110%, 89.6%, and 79.6% at 1, 6, and 24 months respectively (P=0.62 by ANOVA). The changing pattern of impedance showed stepwise decreasing trend from the initial value of 816±272 ohm to 590±185 ohm during the follow-up period (P=0.80 by ANOVA).
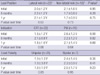
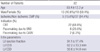
In addition, there were no significant changes in the threshold voltage over time within several subgroups divided by some variables such as LV lead location, procedure indication, or lead polarity (Table 3, Fig. 3). For example, in the lateral location group (lateral, posterolateral, or anterolateral cardiac vein) LV pacing thresholds were 2.0±1.2 V, 2.2±1.2 V, and 2.1±1.2 V at index procedure, 6 months, and 1 yr, respectively (P=0.63). Similarly, change in pacing threshold was not great in the other subgroups as well during the follow-up. On the other hand, its values between the subgroups at the specific follow-up points did not show significant differences; lateral versus non-lateral location group, CRT versus PM group, and unipolar versus bipolar group at baseline, 6 month, and 1 yr respectively (Table 3).
The cumulative rates of lead revision due to capture failure were 3.1% (n=1), 6.3% (n=2), and 9.4% (n=3) in 1 month, 6 month, and 2 yr follow-up. At 1 week after the implantation, capture failure was developed in the 56 yr-old female patient who had a unipolar lead in the lateral cardiac vein for CRT. The other cases occurred at 6 week and 19 months after the procedure; 73 yr-old male with a unipolar lead in the anterolateral cardiac vein for CRT and 39 yr-old female with a unipolar lead in the lateral cardiac vein for PM. However, any other serious complications such as intractable diaphragmatic pacing, coronary sinus perforation, or LV lead-related infections requiring lead revision were not observed over the two-year follow-up period. Only one case of phrenic nerve capture at left lateral decubitus position (50 yr-old female with a lead in the lateral cardiac vein) was detected 4 weeks after the implantation. She was educated to avoid lying on the left side. Then she has been well managed till now (up to 30 months) with the pacing parameters remained within stable range (threshold of 1.25 V and impedance of 569 ohm).
According to the recent study that enrolled 136 consecutive patients who underwent TV replacement surgery, need for permanent pacemaker was as high as 21% after the operation (7). Moreover, multivalve procedure, especially when including TV operation, was one of the strongest independent predictors for the need of a pacemaker (8-10). Transvenous RV pacing is, however, generally contraindicated when the TV prosthesis (especially mechanical valve) is present, out of concern that the mechanical valve and pacemaker lead system might damage each other. Epicardial LV pacing through a thoracotomy or sternotomy could be a possible alternative in this situation. However, these invasive approaches may be too risky (11) and infeasible, especially when the patients have already undergone multiple open heart surgery. In our study population, mean number of operations and replaced valves were 2.4±0.8 and 2.5±0.5 respectively in PM group. Therefore, implantations of cardiac pacing leads into the coronary sinus would be the best option for these specific situations. However, there have been only a few case reports about the LV leads implanted in the presence of TV prosthesis and their long-term performance (1, 2).
Aside from the cases with mechanical TV prosthesis, transvenous LV lead implantation rate is continuously increasing as CRT has been known to improve survival and quality of life in patients with advanced heart failure and dyssynchrony (3, 4). This increasing enthusiasm for CRT makes data on the long-term performance and safety of transvenous LV lead implantation more important. Of course, epicardial LV lead placement through surgical approach is also possible alternative for CRT. However, open chest surgery must be a great burden on the patients with advanced symptomatic heart failure. Despite these situations, little is still known on the stability of leads deployed into the cardiac veins for CRT as is for PM after TV replacement surgery. Although a multicenter study over 2,000 patients on this subject was carried out, its result was in part limited by short follow-up duration of 6 months (6).
In this study, long-term performance of LV lead was stable and favorable with no significant changes in its position (Fig. 1C) and in pacing parameters over the 2 yr (Fig. 2). The LV lead revision rate due to capture failure were 6.3% (n=2) and 9.4% (n=3) in 6 month and 2 yr follow-up respectively, which are very similar to the outcomes of previous reports (6, 12, 13). Although limited by small sample size, lead revision rate of PM group (1 out of 10) did not seem to be significantly different from that of CRT group (2 out of 22). This revision rate might be thought somewhat high compared to that of RV pacing lead, which was recently reported to be 1.5% to 3.3% (14, 15). However, LV lead revision rate is sure to decrease to a lower level in the near future through rapid advancement in lead design and technology as was true with RV lead; dislodgement rate of first generation RV lead once reached 18% (16). In terms of the other complication, we detected one case of phrenic nerve capture (3.1%) over 2 yr observation, which is also comparable to the previous reports (1% to 3%) (6, 12). Any other serious problems such as cardiac vein perforation or infection were not found in this study.
As already mentioned, LV lead pacing threshold remained stable over 2 yr without significant changes. This stability was still maintained in various subgroups divided according to some variables including lead deployment position, indication of implantation, or lead polarity (Table 3).
Although present study is a retrospective analysis of small sized cohort, this was the first report on the long-term prognosis of LV lead in Korea and our data represent an addition to a very limited number of published reports on this subject. In addition, to the best of our knowledge, this is the largest case series study worldwide on the performance of transvenous LV lead in the presence of TV prosthesis.
Taken all together, transvenous LV lead implantation seems safe and feasible procedure with favorable stability for CRT or PM in the presence of TV prosthesis. Systematic, larger-scale studies are needed for the future considering the steep increase in the rate of LV lead procedure.
Figures and Tables
Fig. 1
Long-term stability of a left ventricular lead implanted in lateral cardiac veins. LV lead implantation was performed due to both complete atrioventricular block and mechanical tricuspid valve (A, B). The lead remained stable without dislodgement for 42 months (C).
mAV, mechanical aortic valve; mMV, mechanical mitral valve; mTV, mechanical tricuspid valve.
Fig. 2
Pacing parameters remain stable without significant changes over 2 yr follow-up. There was no significant change in relative threshold voltage to the initial value as well as lead impedance over 2 yr follow-up.
*Relative threshold (%)=follow-up voltage/initial voltage×100.
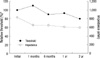
Fig. 3
Serial changes in LV pacing threshold and impedance in various subgroups. Long-term stabilities in threshold voltage and lead impedance are still maintained in various subgroups divided depending on lead position, lead polarity, and indication of lead implantation.

Table 3
Serial changes in LV lead threshold* in various subgroups
Data are number (%) or mean±standard deviation.
*Threshold tests were done at 0.4 ms pulse width; †Lateral position indicates the cases in which the pacing leads were implanted into lateral, posterolateral, or anterolateral cardiac vein whereas non-lateral position posterior, anterior, or middle cardiac vein; ‡P value between subgroups at each time point.
CRT, cardiac resynchronization therapy; LV, left ventricular; PM, permanent pacemaker.
ACKNOWLEDGMENTS
We are grateful to the specialized registered nurse and radiology technologists in the cardiac electrophysiology laboratories of Asan Medical Center (Soon-Hee Kim) and Seoul National University Hospital (Ji-Young Lee, Dong-Hyun Kim).
References
1. Bos HS, Pop GA, Stel EA, van Gelder BM. Dual site coronary sinus pacing in a patient with an artificial tricuspid valve prosthesis. Pacing Clin Electrophysiol. 2004. 27:1451–1452.

2. Yoda M, Hansky B, Schulte-Eistrup S, Koerfer R, Minami K. Left ventricular pacing through the anterior interventricular vein in a patient with mechanical tricuspid, aortic and mitral valves. Ann Thorac Surg. 2005. 80:328–330.

3. Cleland JG, Daubert JC, Erdmann E, Freemantle N, Gras D, Kappenberger L, Tavazzi L. Cardiac Resynchronization-Heart Failure (CARE-HF) Study Investigators. The effect of cardiac resynchronization on morbidity and mortality in heart failure. N Engl J Med. 2005. 352:1539–1549.

4. McAlister FA, Ezekowitz J, Hooton N, Vandermeer B, Spooner C, Dryden DM, Page RL, Hlatky MA, Rowe BH. Cardiac resynchronization therapy for patients with left ventricular systolic dysfunction: a systematic review. JAMA. 2007. 297:2502–2514.
5. Ko JS, Jeong MH, Lee MG, Lee SE, Kang WY, Kim SH, Park KH, Sim DS, Yoon NS, Yoon HJ, Hong YJ, Park HW, Kim JH, Ahn Y, Cho JG, Park JC, Kang JC. Left ventricular dyssynchrony after acute myocardial infarction is a powerful indicator of left ventricular remodeling. Korean Circ J. 2009. 39:236–242.

6. León AR, Abraham WT, Curtis AB, Daubert JP, Fisher WG, Gurley J, Hayes DL, Lieberman R, Petersen-Stejskal S, Wheelan K. MIRACLE Study Program. Safety of transvenous cardiac resynchronization system implantation in patients with chronic heart failure: combined results of over 2,000 patients from a multicenter study program. J Am Coll Cardiol. 2005. 46:2348–2356.
7. Jokinen JJ, Turpeinen AK, Pitkänen O, Hippeläinen MJ, Hartikainen JE. Pacemaker therapy after tricuspid valve operations: implications on mortality, morbidity, and quality of life. Ann Thorac Surg. 2009. 87:1806–1814.

8. Koplan BA, Stevenson WG, Epstein LM, Aranki SF, Maisel WH. Development and validation of a simple risk score to predict the need for permanent pacing after cardiac valve surgery. J Am Coll Cardiol. 2003. 41:795–801.

9. Jung SH, Lee JW, Je HG, Choo SJ, Chung CH, Song H. Surgical outcomes and post-operative changes in patients with significant aortic stenosis and severe left ventricle dysfunction. J Korean Med Sci. 2009. 24:812–817.

10. Shinn SH, Oh SS, Na CY, Lee CH, Lim HG, Kim JH, Yie KS, Baek MJ, Song DS. Short- and long-term results of triple valve surgery: a single center experience. J Korean Med Sci. 2009. 24:818–823.

11. Daoud EG, Kalbfleisch SJ, Hummel JD, Weiss R, Augustini RS, Duff SB, Polsinelli G, Castor J, Meta T. Implantation techniques and chronic lead parameters of biventricular pacing dual-chamber defibrillators. J Cardiovasc Electrophysiol. 2002. 13:964–970.

12. Nof E, Gurevitz O, Carraso S, Bar-Lev D, Luria D, Bachar S, Eldar M, Glikson M. Comparison of results with different left ventricular pacing leads. Europace. 2008. 10:35–39.

13. Bulava A, Lukl J. Single-centre experience with coronary sinus lead stability and long-term pacing parameters. Europace. 2007. 9:523–527.

14. Pavia S, Wilkoff B. The management of surgical complications of pacemaker and implantable cardioverter-defibrillators. Curr Opin Cardiol. 2001. 16:66–71.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download