Abstract
The permanent impairment evaluation for children in developmental stage is very difficult and it is even impossible in some cases. The impairment evaluation for developing children has not yet been included in the guideline of the American Medical Association. Due to frequent medical and social demands in Korea, we developed an impairment evaluation guideline for motor impairment, intellectual disability/mental retardation, developmental speech-language disorder and epilepsy caused by pediatric cerebral injuries, or cerebral lesions other than the developmental disorders such as autism. With the help of various literature and foreign institutions, we developed our in order to develop a scientific guideline for pediatric impairment that is suited to Korean cultural background and social condition.
The Disability Rating System which was enacted by Korean government (2003) has by far, been limited to few developmental disabilities including the mental disorder such as autism, and developmental speech-language disorder and epilepsy are the two currently available scopes of the disability rating system (1). The definition and range of socially negotiated pediatric developmental impairment are indeed necessary because of different ranges of pediatric impairments, social agenda for a welfare society, and the change of cultural background by country (2, 3). In addition, a scientifically appropriate impairment evaluation guideline is necessary. For the first time, all related academic societies gathered together to develop a scientific and objective impairment evaluation guideline that fits to the conditions of our country and developed a guideline for motor impairment, intellectual disability/mental retardation, developmental speech-language disorder and epilepsy by focusing more on impairment evaluation (4) than on impairment evaluation for the scientific evaluation which has been done by the American Medical Association (AMA).
Under the supervision of Korean Academy of Medical Sciences, the following pediatric impairment evaluation research team was formed (Table 1).
The team received an education for the background and purpose of developing the impairment evaluation guideline, along with the fundamental concept of impairment and the method and principles of impairment evaluation. An addition to the guideline to permanent impairment evaluation which was published by the AMA in 2001 (5th edition), various systems in several European, American and Asian countries were studied for the analysis. By actively utilizing these guidelines, comparative reviews for the currently used methods in the impairment evaluation-related legislations of our country have been made to develop the pediatric impairment evaluation guideline that is suited to the culture of our country, as shown below.
Due to less motor development than the mean of one's age by the causes of cerebral palsy, pediatric brain injuries and other pediatric brain lesions occurring before 18 yr old, it is pediatric motor impairment that is characterized by severe functional limitations on the movements of upper limb, lower limb and body trunk (5).
Since there are many difficulties to adopt adult's guideline, it has to be complemented. There are several forms of epileptic syndromes which exist only in pediatric ages (6). The seizure pattern is different from that of adult. Global developmental delay, mental retardation, learning disorder, language disability, behavioral disability, body injury, and motor skill impairment could develop in spite of treatment with antiepileptic drugs (7), which can cause impediments in normal growth and development (8). Therefore, an evaluation guideline with consideration of these problems is necessary.
It indicates the communication disorders by the delay in acquirement of language because of abnormal cerebral physiological processes in understanding or expressing speech and language (9). The developmental speech-language disorder could be diagnosed inclusively for language problems that appear during the age of children and adolescence less than 18 yr old. It could be classified by the secondary causes when it appears in the presence of several factors such as mental retardation (intellectual impairment), autism, hearing loss and epilepsy. Furthermore, a specific language impairment occurs without any specific causes (10, 11).
The evaluation for pediatric motor impairment is available when a child received continuous medical treatments for more than 12 months after the occurrence of the disease caused by cerebral lesions. The impairment has to last or to be expected to last for a continuous period of not less than 6-12 months. If significant functional improvements were found to be progressed, impairment assessment has to be postponed even if the treatments have lasted for more than 12 months (15).
A specialist diagnosing the evaluation has to confirm that more than a defined period has passed for each disease and the evaluation has been solidified by continuous and active treatments, with a letter of diagnosis, a letter of clinical findings, and medical records. At the medical record, the solid evidence of classifying seizures (detailed description of seizure pattern, findings of electroencephalography, findings of cerebral imaging, statement of reliable eyewitness etc.), accurate frequency of seizures, and evidence of active treatment (patient's compliance, drug prescription, drug level in blood and sincerity in life style management) have to be described.
Since the language in children has the characteristics of showing continuous development by 7 yr old, a significant mistake could be made if the current age of a child was not considered at the evaluation of language disorder (16). Therefore, the percentile consideration of the current delay level of language ability, compared to average language development of one's age, becomes the main guideline for the degree of language disorder.
To diagnose intellectual disability/mental retardation, significantly sub-average intellectual functioning (intelligence quotient ≤70-75) and the significant limitations of adaptive skills, which manifests before the age of 18 yr, need to be simultaneously confirmed (12-14). If one has limitations of adaptive behaviors with intelligence quotient above 70-75, it could not be diagnosed as intellectual disability/mental retardation. If one could be observed with less than average intellectual ability along with severe limitations of adaptive skills which were caused by accidents or diseases occurring after the age of 18 yr, intellectual disability/mental retardation could not be diagnosed.
There are 1) Symptoms caused by the persistence of primitive reflexes and abnormal postural reactions, 2) Change of muscle tone occurring by the invasion of specific motor pathways in brain, and 3) Delay or Derangement of motor milestone caused by the developing brain injuries or brain lesions. Unlike adults, the evaluation for pediatric motor impairment is very difficult since the aspects of growth and development of children have to be considered in the interpretation of an assessed result. Namely, the motor ability of a child could be differently interpreted since it depends upon the age of the child who performed the motion. With the growth of a child, an abnormal movement pattern(s) found at earlier age could be changed to other abnormal movement pattern(s), and the motor development could be affected and interrupted by the other developmental impairments such as Intellectual disability/mental retardation or behavioral disorder. Therefore, the precise evaluation for pediatric motor impairment is not an easy task at all.
Diagnosis of basic seizures follows the diagnosis guideline of International League against Epilepsy (ILAE) prepared in 1981 (8). In case of partial seizure, it is classified into the 'simple partial seizure' without the loss of consciousness while having a seizure, and into 'complex partial seizure' that occurs with loss of consciousness while having a seizure. In the forms of generalized seizures, there are 'absence seizure' that a patient loses consciousness for few seconds; the 'generalized tonicclonic seizure' that a patient collapses with complete loss of consciousness with tonic and clonic muscular contraction; 'tonic seizure', 'clonic seizure', 'myoclonic seizure' that a patient experiences the sudden occurrence of non-voluntary contraction of the muscles in four limbs or in body trunk, and 'atonic (or akinetic/astatic) seizure' which shows the pattern that a patient drops his head to the front by losing muscular tone or bending his legs.
For the diagnosis of epilepsy, it follows the ILAE diagnosis guideline prepared in 1989 (17).
Developmental speech-language disorder could be divided into various fields including developmental language delay, articulation disorder, stuttering (fluency disorder), resonance disorder, and voice problem (9). To achieve scientific and objective evaluation, oral motor function evaluation and other evaluations for language and speech, by using language diagnostic tools which have been standardized for the characteristics of Korean language, have to be performed to assess the grade for each developmental speech-language disorder.
Language delay could be the early symptom of intellectual disability/mental retardation. As a child is getting older, he/she might be brought to a hospital for the problems on acquisition of academic skills. Majority of children with intellectual disability/mental retardation show some degree of clumsiness in gross and fine motor areas. Significant limitations in adaptive function end up with significant functional limitations which require supports in terms of independent living.
In the clinical assessment for children, there are a neurological examination that evaluates cortical motor systems and a method of using child motor function assessment tool that was developed to evaluate the motor function for children in different age (19). Recently, brain Magnetic Resonance Imaging (MRI) is used as an important assessment tool to examine the presence of brain lesions (20, 21).
As the neurological examination, it was evaluated in 4 stages by assigning total 16 points for the presence of plegia in 4 limbs. Abnormal movement patterns, which as muscle tone, dystonia, choreoathetosis and ataxia/dysmetria, occurs at each limb. As the child motor function assessment tool, the Gross Motor Function System Classification (GMFCS) that was already translated into Korean was used (19). The system adopted 5 stages of classification for 4 age ranges to assign 8 points for each classification, which makes total point of 40. The brain imaging findings was classified by assigning total 4 points according to the presence of ventricular enlargement, parenchymal injuries and bilateral injuries.
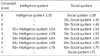
For severity evaluation for child motor impairment, 3 types of tests described above are conducted, and each test result is scored according to the degree of its effect on motor impairment and summed to determine the severity of motor impairment in a child. We considered the presence of motor functions, that a child can perform, as the most important category of the evaluation (40 points: 66.7%), and the degree of plegia in 4 limbs and the degree of abnormal movement pattern were evaluated (16 points: 26.7%). Finally, the presence and degree of brain injuries in brain image test were evaluated (4 points: 6.6%) to assign maximum 60 points as the highest severity of motor impairment (Table 2). In addition, the total points that were calculated by summing up the points acquired from 3 types of assessment tools could be divided into 8 steps of grade by using the conversion table listed below (Table 3).
Evaluation time (evaluation period and reevaluation period) is described below. 1) Many cases of epileptic encephalopathies such as infantile spasm and Lennox-Gastaut syndrome, which have been known to have worse prognosis, are not controlled by antiepileptic drugs. Therefore, the evaluation is available after 6 months of treatment period from the first diagnosis of the syndromes, and the reevaluation period is set as 1 yr. 2) Epileptic children under 6 yr old with symptom that belongs to epileptic encephalopathy could be evaluated after 1 yr of treatment period from the first diagnosis of the epilepsy, and the reevaluation period is set as 2 yr. 3) Epileptic children under 6 yr old with symptom that belongs to epileptic encephalopathy could be evaluated after 1 yr of treatment period from the first diagnosis of the epilepsy, and the reevaluation period is set as 2 yr. 4) However, if a child receives a same grade evaluation from the 2 rounds of reevaluations as the first evaluation (the same grade evaluations from 3 rounds of reevaluations including the first evaluation), the case could be excluded from the later obligative reevaluation.
The method of impairment evaluation for pediatric epilepsy is described below. Other than the interviews for medical examination, brain images (brain CT and brain MRI) and electroencephalogram results are integrated for the evaluation. If seizure lasts despite active treatment with antiepileptic drugs, it is judged according to seizure types shown in Table 4.
If a child older than 2 yr old shows a persistent problem even after receiving continuous speech therapy for more than 12 months due to the major symptoms including developmental language delay, speech articulation disorder and stuttering, the child could have evaluation for the impairment of language. The impairment evaluated has to be delayed if language ability is significantly improved even though the treatment period has been passed for more than 12 months (22). For the language assessment, several standardized tools have been introduced, however, Preschool Receptive-Expressive Language Scale (PRES) and Sequenced Language Scale for Infants (SELSI) which can evaluate the integrated language abilities (syntax, semantics and pragmatics) have been recommended. To differentiate the grade of developmental language delay, the expressive and receptive language age (months), that is divided by developmental age (months), could be used: it is called the developmental index of language (expressive language index and receptive language index). The age matched percentile method by using PRES or SELSI is also available, however, the age matched percentile method is recognized to be more reasonable method. As the evaluation tool for speech articulation disorder, the Picture Consonant Articulation Test (PCAT), Assessment of Phonology and Articulation for Children (APAC), and Urimal Test of Articulation and Phonology (U-TAP) could be used to recognize speech articulation accuracy. Stuttering Severity Instrument (SSI), Stuttering Interview test (SI) and Paradise-Fluency Assessment test (P-FA) are available for the grade of stuttering severity in the speech fluency disorder. Since the clarity of articulation could interfere with the severe hyper-nasality by cleft palate, it might be accepted as one of the causes of the speech articulation disorder. The grading by using a Nasometer is the most universal evaluation method of the resonance disorder. Since voice disorder does not become significant for children, the impairment is accepted only in case of tracheotomy or esophageal speech.
Developmental speech-language disorder is not assessed by summing up developmental language delay, speech articulation disorder, speech fluency disorder, resonance disorder, and voice disorder. Therefore, it is principally classified by dividing into eight graded according to each problem (Table 5).
It is recommended that impairment evaluation associated with intellectual disability/mental retardation should be done after the age of 5 yr. The impairment could be evaluated at the time when significant functional limitations compared to persons of the same age, have been noticed even after adequate medical, educational and environmental interventions for over 12 months or more. Therefore, impairment evaluation associated with intellectual disability/mental retardation needs to be postponed for cases where significant functional improvements are expected or noticed with medical, educational and environmental interventions.
For children with definite etiologies of intellectual disability/mental retardation such as trisomy 21 or chromosome 5p deletion, impairment evaluation for intellectual disability/mental retardation could be made at the age from 3 yr old to less than 5 yr old. However, it is approved as a temporary impairment in this case, and the reevaluation of impairment needs to be made again after 5 yr of age.
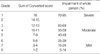
Impairment associated with intellectual disability/mental retardation is rated as follows; 1) The intellectual function and adaptive skills are evaluated by individual intelligence tests such as the Wechsler intelligence scale and social maturity test, respectively; 2) Both intelligence quotient and social quotient yield converted scores according to Table 6; 3) The converted scores are summed to rate impairment according to Table 7.
For children of older than 5 yr whose intellectual function is too low to be tested with a standardized intelligence test, the development quotient in cognitive area (cognitive function in months/chronologic age in months×100) which is calculated with a development assessment tool such as the Bayley Scales of Infant and Toddler Development, could be used as an equivalent intelligence quotient.
Since the developmental children are under the growth and development period different from adults, their permanent impairment evaluations are extremely difficult. Probably due to such a reason, it is very difficult to find the impairment evaluation for children in the Guides to the Evaluation of Permanent Impairment issued by the AMA. Unlike the U.S.A. or European countries where the pediatric impairment is totally managed by the government, the management for impairments of developmental children in Korea is mainly relying upon guardians. Under this circumstance, faster impairment evaluation may be necessary for even developing children if medical impairment evaluation could be done. Therefore, we aimed to prepare an impairment evaluation proposal for children with cerebral lesions within available scopes after analyzing the developmental procedures of normal children and the development mechanisms of cerebral lesions or cerebral injuries, and the limitations and disagreements on the study procedures are discussed.
Applying the findings of brain images into pediatric motor impairment is the problem in Pediatric motor impairment evaluation. Since the cerebral nerve system of children has been known to have more neuroplasticity than adults (20), the degree of cerebral injury represented in brain imaging findings has been shown to have a limitation in evaluating the severity of children. However, a recent study reported abnormal findings in 89% of children with cerebral palsy (21) in the brain imaging tests, and the relationship with the degree of brain parenchymal injuries has been reported (23). Therefore, it could be used as one of individual evaluation methods to complement the drawbacks of several evaluation categories in evaluating the pediatric motor impairment. Secondly, there are neurological findings used to evaluate the severity or the presence of diseases in cerebral motor nervous system. Namely, spasticity pathological reflexes, primitive reflexes, presence of abnormal movement patterns and muscle strength could be listed. Although these items could be used to evaluate the abnormal findings and depend on the lesion of developmental motor nervous system, there may be some debates on whether this could be used to judge the severity of impairment by the presence or intensity. The use of the motor function evaluation system has limitations, and the accuracy is downgraded for the children in younger age. Because this functional evaluation could be affected by diverse factors other than rehabilitation training, environment and motor impairment, it should be pointed out that the evaluation could largely be affected by the role of evaluators compared to other evaluation items.
Pediatric epilepsy has the characteristics of changing its pattern by age. So, there is a limitation in evaluating the solidified permanent evaluation. However, since intractable epilepsy is essentially accompanied with multiple disorders, it has to be evaluated. For example, the pediatric epilepsy is commonly accompanied with global developmental delay, mental retardation, learning disorder, language disorder, and behavioral disorder. Therefore, it has been suggested that these cases should separately be evaluated by using the guideline for multiple disabilities. In cases of patients with body injury and motor skill impairment due to intractable epilepsy, each evaluation has to separately be evaluated by following the guideline for multiple disabilities. Further discussions should be made on this matter.
An evaluating developmental speech-language disorder, the following problems could be encountered; 1) the difficulty of accepting permanent evaluation before 7 yr of age, 2) the lack of evaluation tool which enables age-matched percentile and its difficulty in detailed differentiation by grade, 3) the proportion of diagnosis for the specific language impairment could vary by its close relationship to other disabilities and by the time of diagnosis, 4) the evaluation for developmental speech-language disorder has difficulties to tie all evaluating items into one scoring system, because of their strong heterogeneity between items, compared to the evaluation for motor evaluation and intellectual disability. Therefore, the group wide reviews by specialists are required.
The present impairment rating guideline for intellectual disability/mental retardation uses adaptive skills along with intellectual function which is based on the current definition of intellectual disability/mental retardation, and the impairment caused by intellectual disability/mental retardation is quantified by using intelligence quotient, and social quotient as shown in Table 6, 7.
Although persons with mild degree of intellectual disability/mental retardation usually show independent adaptive skills through rehabilitation and education, they might need supports during their life-span on an episodic basis or on a regular basis. Evaluation tools for adaptive skills have been developed in some countries. However, with cultural difference and little experience of using these tools, the social maturity test was selected for the evaluation of adaptive skills in Korea. However, as described above, the social maturity test is not a sensitive tool to evaluate significant limitations of adaptive skills which may occur intermittently or for a short period of time during life-span. Therefore, it is necessary in near future to develop an appropriate tool for Koreans for the evaluation of adaptive skills.
Figures and Tables
References
1. Guideline to Governmental Disability Rating System. 2003. Ministry of Health and Welfare: Republic of Korea.
2. Suh T. Current status and direction of the expansion of statutory disabilities in the disability act. Indep Med Exam. 2005. 2:12–63.
3. Patel B, Buschbacher R, Crawford J. National variability in permanent partial impairment ratings. Am J Phys Med Rehabil. 2003. 82:302–306.

4. Lee KS. Assessment of physical impairment and disability evaluation: problem of present system and design for better system. J Korean Neurosurg Soc. 1994. 23:276–282.
5. United States. Social security administration, general information. Disability evaluation under social security. 1999. 2nd ed. Baltimore: Social Security Administration, Office of Disability;2–3.
6. Roger J, Thomas P, Hirsch E. Epileptic syndromes in Infancy, childhood, and adolescence. 2005. 4th ed. Montrouge: J. Libbey.
7. Nehlig A, Motte J, Moshe SL, Plouin P. Childhood Epilepsies and Brain Development. 1999. Malaysia: John Libbey & Company Ltd;93–141.
8. Schwartzkroin PA, Moshe SL, Noebels JL, Swann JW. Brain Development and Epilepsy. 1995. PA.: Oxford University Press Inc;9–33.
9. Accardo PJ. Accardo PJ, Rogers BT, Capute AJ, editors. The child who does not talk. Disorders of language development. 2002. Baltimore: York Press Inc;113–124.
10. Shevell MI, Majnemer A, Rosenbaum P, Abrahamowicz M. Etiologic determination of childhood developmental delay. Brain Dev. 2001. 23:228–235.

11. Leonard LB, Sabbdini L, Leonard JS, Volterra V. Specific language impairment in children: a cross-linguistic study. Brain Lang. 1987. 32:233–252.

12. Definition of mental retardation. American Association on Intellectual and Developmental Disabilities. 2007. Accessed 2 July 2007. Washington, DC: American Association on Intellectual and Developmental Disabilities;Available at:
http://www.aaidd.org/.
13. American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 1994. 4th ed. Washington, DC: American Psychiatric Association.
14. ICD-10 guide for mental retardation. World Health Organization. 1996. Accessed 2 July 2007. Geneva, Switzerland: World Health Organization;Available at:
http://www.who.int/mental_health/media/en/69.pdf.
15. Bleecker M. Cocchiarella L, Anderson GBJ, editors. The central and peripheral nervous system. Guides to the evaluation of permanent impairment. 2001. 5th edition. USA: American Medical Association;338–340.

16. Beitchman JH, Brownlie EB, Inglis A, Wild J, Mathews R, Schachter D, Kroll R, Martin S, Ferguson B, Lancee W. Seven-year follow-up of speech/language impaired and control children: speech/language stability and outcome. J Am Acad Child Adolesc Psychiatry. 1994. 33:1322–1330.
17. Commission on Classification and Terminology of the International League against Epilepsy. Proposal for revised classification of epilepsies and epileptic syndromes. Epilepsia. 1989. 30:389–399.
18. Farrell K, William O, Tatum IV. Wyllie E, Gupta A, Lachhwani DK, editors. Encephalopathic Generalized Epilepsy and Lennox-Gastaut Syndrome. The Treatment of Epilepsy: Principles & Practice. 2006. 4th edition. Philadelphia: Lippincott Williams & Wilkins;429–440.
19. Wood E, Rosenbaum P. The gross motor function classification system for cerebral palsy: a study of reliability and stability over time. Dev Med Child Neurol. 2000. 42:292–296.

20. Ashwal S, Russman BS, Blasco PA, Miller G, Sandler A, Shevell M, Stevenson R. Practice parameter: diagnostic assessment of the child with cerebral palsy: report of the Quality Standards Subcommittee of the American Academy of Neurology and the Practice Committee of the Child Neurology Society. Neurology. 2004. 62:851–863.

21. Bax M, Tydeman C, Flodmark O. Clinical and MRI correlates of cerebral palsy: the European Cerebral Palsy Study. JAMA. 2006. 296:1602–1608.




 PDF
PDF Citation
Citation Print
Print







 XML Download
XML Download