1. McBride ED. Disability evaluation and principles of treatment of compensable injuries. 1963. 6th ed. Philadelphia: JB Lippincott Co.
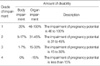
2. Gunnar A, Linda C. American Medical Association. Guides to the Evaluation of Permanent Impairment. 2000. 5th ed. New York: American Medical Association;143–171.
3. Ministry of Health and Welfare. Guidance for the disability grading. 2003.
4. Li Z, Kang SH, Lee SD. Review of Korean Disability Evaluation Systems and Suggestions for the Improvement Direction. Korean J Leg Med. 2007. 31:16–30.
5. American Medical Association. Guides to the evaluation of permanent impairment. 2007. 6th ed. New York: American Medical Association;129–158.
6. Lee KS. Assessment of physical impairment and disability evaluation: problem of present system and design for better system. J Korean Neurosurg Soc. 1994. 23:276–282.
7. Ministry of Health, Labor and Welfare in Japan. Outline of the Systems and Basic Statistics in Annual Reports on Health and Welfare 1998-1999 Social Security and National Life from white paper and reports. 2007. Volume 2-II:(
www-admin@mhlw.go.jp).
8. Rosen RC, Hatzichristou D, Broderick G, et al. Lue TF, Basson R, Rosen R, editors. Clinical evaluation and symptom scales: Sexual dysfunction assessment in men. Sexual Medicine: Sexual Dysfunctions in Men and Women. 2004. Paris: Health Publications;173–220.
9. Baker LA, Sigman D, Mathews RI, Benson J, Docimo SG. An analysis of clinical outcomes using color Doppler testicular ultrasound for testicular torsion. Pediatrics. 2000. 105:604–607.

10. Carter SS, Shinohara K, Lipshultz LI. Transrectal ultrasonography in disorders of the seminal vesicles and ejaculatory ducts. Urol Clin North Am. 1989. 16:773–790.
11. Korean Medical Association. Guides to the Evaluation of Permanent Impairment. 2005. 1st ed. Seoul: Korean Medical Association.
12. Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL Jr, Jones DW, Materson BJ, Oparil S, Wright JT Jr, Roccella EJ. Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. National Heart, Lung, and Blood Institute. National High Blood Pressure Education Program Coordinating Committee. Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension. 2003. 42:1206–1252.

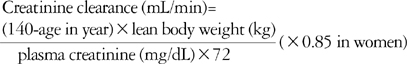
13. Denker BM, Brenner BM. Kasper DL, Braunwald E, Fauci AS, Hauser SL, Longo DL, Jameson JL, editors. Azotemia and urinary abnormalities. Harrison's Principles of Internal Medicine. 2005. 16th ed. New York: McGraw-Hill.
14. Schwartz GJ, Haycock GB, Edelmann CM Jr, Spitzer A. A simple estimate of glomerular filtration rate in children derived from body length and plasma creatinine. Pediatrics. 1976. 58:259–263.
15. Andrew C, Peterson MD, George D, Webster MD. Wein AJ, Kavoussi LR, Novick AC, Partin AW, Peters CA, editors. Urodynamic and Videourodynamic Evaluation of Voiding Dysfunction. Campbell-Walsh urology. 2007. 9th ed. Philadelphia: Saunders;1986–2010.




 PDF
PDF Citation
Citation Print
Print

















 XML Download
XML Download