Abstract
A extragonadal malignant teratoma of the extremity is a rare pheonemenon. We describe a extremely rare case of malignant teratoma of the left proximal humerus in a 14-yr-old female. Radiologic evaluations, including magnetic resonance imaging, suggested a malignant bone tumor, but a pathological examination revealed an immature bony teratoma. Bone scintigraphy and positron emission tomography computed tomography scan showed increased uptake of proximal humerus but no other abnormal lesion.
Teratomas are congenital tumors that are usually found in the gonads, and are only rarely detected in extragonadal areas, such as, the mediastinal, retroperitoneal and sacrococcygeal regions. To the best our knowledge, an extragonadal teratoma of the long bone has not been previously reported in the literature. We describe clinical, radiologic and pathologic findings of an exceedingly rare case of malignant teratoma of the proximal humerus.
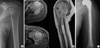
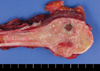
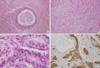
A 14-yr-old female was admitted with painful limited motion of the left shoulder joint. She was transferred to our institute for further study and proper management under impression of malignant bone tumor. On physical examination, the patient had slightly reduced shoulder joint motion, but no palpable protruding mass. A chest radiograph revealed no abnormality. However, a radiograph of the humerus showed ill defined moth eaten to permeative destructive lesion associated with cortical perforation of proximal humerus (Fig. 1A). Magnetic resonance imaging (MRI) well demonstrated the entire extent of the tumor, which showed inhomogeneous enhancement after contrast agent administration. Both the intraossoeus and extraosseous tumor components were evident on transaxial gradient-echo MR images (Fig. 1B). 99 m Tc-MDP scintigraphy and an 18F-FDG whole body positron emission tomography (PET) scan showed uneven increased uptake at the left proximal humerus, but no other abnormality was detected. Routine blood tests and urinalysis were all within normal limits. Initial diagnostic considerations included; leukemic infiltration, lymphoma, osteomylelitis, and a malignant bone tumor, such as, an osteosarcoma. A subsequent surgical biopsy was performed and the pathological report revealed an immature bony teratoma. On gross inspection, the cut surface of the resected proximal humerus showed a homogenous grayish white flesh-like tissue that had replaced the whole epimetaphysis and a part of the diaphysis (Fig. 2). Malignant teratoma were graded using a method described by Robboy and Scully (1); degree of immaturity, presence and quantity of a neuroepithelial component. Grade 1 tumors with rare foci of immature neuroepithelial tissue occupy less than one low power field (40x), grade 2 tumors occupy 1 to 3, and grade 3 tumors occupy more than 3 low power fields. Microscopically, teratomas are characterized by the presence of squamous cell nests (Fig. 3A), neuroglial proliferation (Fig. 3B) and endodermal glandular structure (Fig. 3C), as was found in the present case. The latter looked immature in appearance, which is not found in normal adult tissue. However, true neuroepithelial nests were not identified in the present case. Immunohistochemical staining demonstrated the expressions of glial fibrillarary acidic protein (GFAP) and CD56 expression in neuronal tissue (Fig. 3D). Based on the above-mentioned grading system, the tumor of the present case was classified as a grade 1 immature teratoma bearing immature endodermal glandular structures. Wide excision and reconstruction with tumor prosthesis and bone cement were performed (Fig. 1C). The surgical margin was free of tumor. There was no evidence of local recurrence or distant metastasis at 30 months postoperatively. According to the Musculoskeletal Tumor Society Scoring System (2), final functional score was 27 (90% of normal). Chemotherapy was not administered postoperatively due to the low grade malignancy in this case.
Teratomas are germ cell neoplasms that include tissues arising from the three germ cell layers (3). They usually originate from pluripotent cells, which can differentiate to a wide variety of tissues. The majority of extragonadal teratomas develop from germinal elements, and they usually occur along the migration pathway of the germ cells (4). Resultantly, the sacrococcygeal region is the most frequent extragonadal location; other sites include the mediastinum and retroperitoneum (5). Exceptionally rarely intraosseous teratoma has reported but there has been no reported case involving a long bone in the literature. In 1992, Chinoy et al. (6) reported a case of an extragonadal malignant teratoma of the foot and in 2000, Vazquez et al. (7) described an intraosseous teratoma of the iliac bone. In these previously published reports, initial diagnostic considerations included fibrous dysplasia, Langerhans' cell histiocytosis, aneurysmal bone cyst and a malignant bone tumor, such as, an osteosarcoma. Most skeletal germ cell tumors are metastatic (8) but the pathogenesis of teratoma in the appendicular skeleton is still enigmatic. We failed to detect any other tumors after painstaking effort to find primary site. Another possible pathogenetic theory concerns the heterotopic location of extragonadal germ cells. However, the humerus is not in the migration path of germ cells, and in fact, no teratoma has been identified previously at this site. Thus, we are uncertain about the pathogenesis of the bony teratoma in this case. Nevertheless, since the tumor was confirmed as a grade 1 immature teratoma, a wide surgical excision only was undertaken for comprehensive treatment. She is doing well without evidence of local recurrence or distant metastasis at final follow-up examination.
Figures and Tables
Fig. 1
(A) A radiograph revealing ill defined moth eaten to permeative destructive lesion associated with cortical perforation in the epiphysis and metaphysic of the humerus. (B) Consecutive transaxial T2-weighted gradient-echo MR images showing the intraosseous and extraosseous extent of the tumor, which displayed inhomogeneous high signal intensity. The tumor has penetrated the cortex and lifted the periosteal membrane. This coronal T1-weighted spine echo MR image obtained after intravenous gadolinium administration reveals inhomogeneous tumor enhancement. Note the diaphyseal tumor extension. (C) Reconstruction after wide excision was undertaken using a tumor prosthesis.
References
1. Robboy SJ, Scully RE. Ovarian teratoma with glial implants on the peritoneum. An analysis of 12 cases. Hum Pathol. 1970. 1:643–653.
2. Enneking WF, Dunham W, Gebhardt MC, Malawar M, Pritchard DJ. A system for the functional evaluation of reconstructive procedures after surgical treatment of tumors of the musculoskeletal system. Clin Orthop Relat Res. 1993. 286:241–246.

3. Gatcombe HG, Assikis V, Kooby D, Johnstone PA. Primary retroperitoneal teratomas: a review of the literature. J Surg Oncol. 2004. 86:107–113.

4. Batsakis JG, el-Naggar AK, Luna MA. Teratomas of the head and neck with emphasis on malignancy. Ann Otol Rhinol Laryngol. 1995. 104:496–500.

5. Taori K, Rathod J, Deshmukh A, Sheorain VS, Jawale R, Sanyal R, Bhagat M, Jumle S. Primary extragonadal retroperitoneal teratoma in an adult. Br J Radiol. 2006. 79:e120–e122.

6. Chinoy RF, Soman CS, Swaroop D, Badwar RA. Extragonadal malignant teratoma of the foot. Indian J Cancer. 1992. 29:96–99.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download