Abstract
We present a recurrence prediction model using multiple clinical parameters in patients surgically treated for non-small cell lung cancer. Among 1,578 lung cancer patients who underwent complete resection, we compared the early-recurrence group with the 3-yr non-recurrence group for evaluating those factors that influence early recurrence within one year after surgery. Adenocarcinoma and squamous cell carcinoma were analyzed independently. We used multiple logistic regression analysis to identify the independent clinical predictors of recurrence and Cox's proportional hazard regression method to develop a clinical prediction model. We randomly divided our patients into the training and test subsets. The pathologic stages, tumor cell type, differentiation of tumor, neoadjuvant therapy and age were significant factors on the multivariable analysis. We constructed the model for the training set with adenocarcinoma (n=236) and squamous cell carcinoma (n=305), and we applied it to the test set with adenocarcinoma (n=110) and squamous cell carcinoma (n=154). It was predictive for the in adenocarcinoma (P<0.001) and the squamous cell carcinoma (P=0.037), respectively. Our results showed that our recurrence prediction model based on the clinical parameters could significantly predict the individual patients who were at high risk or low risk for recurrence.
Lung cancer is the leading cause of cancer-related deaths in the world, and non-small cell lung cancer (NSCLC) accounts for nearly 80% of the disease (1). The clinicopathologic staging system has been the standard for determining lung cancer treatment, but it includes heterogenous groups of patients within one stage (2). Nearly 25-80% of NSCLC patients experience recurrences and they have poor prognosis despite curative resection (3, 4).
Adjuvant therapy after surgery has shown a survival benefit for the stage II to IIIA groups, but not for the stage I group (5, 6). Thus, we need to select those patients who can achieve a real survival advantage as weighted against the risk of undergoing adjuvant cytotoxic chemotherapy. In the treatment of NSCLC, in order to achieve more highly selective treatment especially for the high-risk patients for recurrence and to reduce unnecessary toxic treatment to the low-risk patients, we need the ability to predict the surgical outcome of an individual patient. Recent studies have focused on the identification of risk factors that influence postoperative survival and recurrence in a large group of patients, and multiple factors have been proposed, which were not only clinical factors but also biologic markers and gene-expression profiles using microarray (7-9). However, these risk factors could not be applicable to each patient, and any single, definite factor has failed to explain the prognosis. Thereafter, we considered a prediction model using multiple clinical factors, which can be applicable to individual patients at the bedside.
We especially evaluated the early recurrence within one year after surgery and purposed to evaluate the predictability and to find out the limitations of retrospective clinical information.
Our Institutional Review Board approved this study and waived the requirement for individual patient consent (IRB No. 2006-12-038). From 1994 to 2004, a total of 1,640 patients underwent pulmonary resections for the treatment of NSCLC at the Samsung Medical Center in Korea. In every case, after mediastinal nodal staging using a mediastinoscopic biopsy, we performed curative resection and lymph nodes dissection. If mediastinal nodal metastasis was detected from the mediastinoscopic result, then neoadjuvant concurrent chemo-radiation therapy followed. After surgery, patients were regularly followed-up. We scheduled the performance of clinical reevaluations two weeks after surgery and then every three months for the first two years, every six months for the next three years, and once every year thereafter. Each follow-up visit was supplemented by chest radiography. A restaging evaluation including chest computed tomography performed at diagnosis was scheduled in all subjects six months after their operation. Recurrence was defined as any unequivocal occurrence of new cancer foci in a disease-free patient and included all patterns of recurrences (local, regional, and distant). We defined early tumor recurrence as a tumor relapse that occurred within one year of the operation. This cut-off time was clearly an arbitrary one, which we chose based on biological considerations and after a preliminary inspection of our database. Among 1,640 patients, sixty-two patients (3.8%) experienced operative mortality (operative mortality was defined to include all deaths directly related to the surgical procedures regardless of time of occurrence, within thirty days or after thirty days, and of type of hospitalization, intrahospital or extrahospital), and they were excluded from analysis. Therefore, we retrospectively reviewed the charts and radiological findings of 1,578 NSCLC patients and contacted the patients and their families to gather recent information. Clinical variables such as age, gender, pathologic TNM stage, cell type, differentiation, neoadjuvant therapy, adjuvant therapy, presence or absence of double primary malignancies, and completeness of resection were selected for the consideration of recurrence (Table 1).
After we analyzed and performed a predictive model using all the data from 1,578 patients, we classified it into recurred patients and non-recurred patients to evaluate recurrence-predicting factors more definitely. We defined the early recurrence group as patients who had recurred diseases detected within one year postoperatively and the non-recurrence group as the survivors who were recurrence-free more than three years after curative surgery (Fig. 1). Histology was limited to adenocarcinoma (ADC, n=346) and squamous cell carcinoma (SQC, n=459). There were 349 patients (169 in ADC, 180 in SQC) in the early-recurrence group and 456 (177 in ADC, 279 in SQC) in the non-recurrence group.
We first performed univariate and multivariate analysis for the clinical factors affecting recurrence. The statistical algorithm for the recurrence prediction model is constituted by Cox's proportional hazard regression model using a stepwise variable selection method that takes into consideration clinical factors that affect the time to recurrence such as age, gender, cell type, pathological stage, differentiation, and curative resection. All clinical characteristics were considered in a multiple Cox model to determine which demonstrated the strongest associations with recurrence. The clinical parameters other than age were applied without modification as the categorical data. When the hazard ratio calculated by Cox's proportional hazard model was greater than 1.0, the patients were classified as belonging to the high-risk group for early recurrence, and when the hazard ratio was smaller than 1.0, they were classified as belonging to the low-risk group (10). A log-rank test was carried out to compare the survival rates of the two risk groups. For constructing the model, 346 ADC patients and 459 SQC patients were divided into a 2:1 ratio between the training sets (236 in the ADC group, and 305 in the SQC group) and the test sets (110 in the ADC group, and 154 in the SQC group). Each group was stratified by random sampling to equally distribute all the clinical parameters; models were constructed with the training sets, and applied to the test sets. To evaluate the performance of the models, we applied the Kaplan-Meier survival curve and the log-rank test between the risk groups, where 5% was accepted as the significance level.
In this study, we retrospectively analyzed 1,578 patients, who were followed-up at the outpatient clinic after curative lung cancer surgery. The clinical information is listed in Table 1. There were 1,217 men (77.1%), and the mean age of the patients was 61.1 yr (SD, 9.5 yr). The most common histopathologic type was SQC (48.5%), and ADC was the next most common (42.3%). Most patients underwent complete resection at the first surgery (96.8%). During a mean of 40.1 months (SD, 28.1 months) for the follow-up period, 742 patients (47.0%) were diagnosed with recurred diseases, and 349 (47.0%) among them were detected within one year of surgery. During the same period, 527 patients (33.4%) died of cancer-related causes. Before the modeling process, we analyzed the significant factors influencing recurrence. Univariate analysis of the relationship between recurrence and the clinical parameters showed statistically significant for advanced TNM stage (P<0.001, respectively), cell type (P<0.001), differentiation (P<0.001), undergoing neoadjuvant therapy (P<0.001), and adjuvant therapy (P<0.001) (Table 2). Multivariate analysis revealed that age (P<0.001), TNM stage (P<0.001, respectively), cell type (P<0.001), differentiation (P<0.007), and neoadjuvant therapy (P<0.001) were related to the recurrence (Table 2).
Among the total 1,578 patients, there were 349 (22.1%) in the early-recurrence group and 456 (28.9%) in the non-recurrence group, and the early-recurrence group could be further divided with 169 in ADC and 180 in SQC (25.3% vs. 23.5%; ratio to total patients in each cell type). Table 3 shows patients' characteristics for each cell type. There were more male patients in SQC than in ADC. The significant clinical factors associated with recurrence on the univariate and multivariate analyses agreed with those of the total patients.
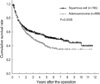
There were 346 ADC patients (of whom 169 belonged to the early recurrence subset and 177 belonged to the subset showing non-recurrence after more than 3 yr). We performed a Cox's model with a training group of 236 and then evaluated the model by applying it to a test group of 110. Stage factors (tumor and nodal factors) and tumor differentiation were finally entered into the model as possible predictive factors (as demonstrated in Table 4). Test group patients were divided into two risk groups (high- and low-risk) using 1.0 as cut-off value with statistically significant results (where the P value is less than 0.001 in the log-rank test). Fig. 2-1 is the Kaplan-Meier curve for the recurrence-free survival instances in high- and low-risk groups.
There were 459 SQC patients (of whom 180 displayed early recurrence and 279 continued to show non-recurrence after more than 3 yr). We performed a recurrence prediction model using on the training set of 305 the same methods as on the ADC patients and then applied the model to the test set of 154. The test set was then divided into two groups, a high-risk group and a low-risk group with statistically significant results (with a P value equal to 0.037 in the log-rank test). The Kaplan-Meier curve for recurrence-free survival is shown in Fig. 2-2.
There has been much recent development in the diagnosis and treatment of NSCLC. However, all patients diagnosed with NSCLC are managed in a uniform manner based on the stage of the disease, regardless of cell type or other heterogeneous characteristics. Neoadjuvant therapy as well as adjuvant therapy has been applied to the advanced stage patient but not to the early stage patient with a high-risk for recurrence. The purpose of our study is to identify the patients who are more likely to recur and may benefit from neoadjuvant or adjuvant therapy. A few studies have investigated a survival prediction in surgically resected patients with NSCLC (9, 11-13). However, a postoperative recurrence prediction has not been studied as much. We focused our predictions of early recurrence to indicate recurrence within one year after curative resection. Early recurrence means that a patient might have a generalized disease before surgery and would benefit from systemic treatment such as chemotherapy.
We used Cox's proportional hazard regression models to see how the factors correlated with the instances of recurrence after surgery. We analyzed several clinical factors as well as current pathologic stage systems, which have been regarded as the most important factors of deciding the prognosis of NSCLC. Since many of the clinical factors associated with NSCLC are related to each other, it is very difficult to separate one factor from the others or to identify all relationships between the factors. So we considered all the factors and tried to make the most optimal model to accurately predict recurrence.
Our prediction model using the total patients' information could distinguish the high-risk group of recurrence from the low-risk group in the test subgroup (data was not shown). We specified the data because there are heterogenous groups in NSCLC. First, we stratified our data according to histology. Many studies have investigated the prognostic significance of different histologies in surgically resected NSCLC patients, but there still remains controversy (14-16). ADC has different characteristics from SQC and their respective recurrence patterns along with them (16). Forty-two percent of the ADC patients were female whereas only 4.8% of the SQC patients were female in this study. The tumor size of the ADC patients was smaller than that of the SQC patients. Okamoto and his colleagues demonstrated that the prognosis after complete resection is different between ADC and SQC (16). In this study, Fig. 3 shows the differences in recurrence between ADC and SQC patients. Second, we limited the cases to include the patients who have recurred within one year and those who did not detect any recurrence after more than three years. The early recurrence group has more aggressive features and is a good candidate for adjuvant treatment. In the ADC patients, there were more cases of early recurrence (25.3% vs. 23.5%, ratio to total patients in each cell type) and fewer cases of three years passing without recurrence (26.5% vs. 36.5%) than for the patients with SQC. For both ADC and SQC, we could predict early recurrence in training and test subgroups, and pathologic TNM stage was the most significant prognostic factor to determine an early recurrence. Comparing the recurrence-free survival curves (Fig. 2), the presence of ADC had a tendency to more accurately distinguish the high-risk group from the low-risk group than did SQC. Yokouchi and his colleagues suggested that in ADC, survival was dominantly affected by N factor, while in SQC, survival was strongly correlated with size, or T factor (17). Fig. 4 shows survival difference in SQC according to tumor size in this study. We used the T stage factor in modeling, instead of size, because tumor size was conceptually included in the T factor. Tumor size has been proposed to be important in new revised staging system, and there may be need to study more about it.
We tried to predict recurrence within clinical parameters. However, there exist several limitations in our retrospective study. First, we gained the information from the charts, the radiological reports, and the patients and their family members, so it was difficult to get certain information, such as the performance status and smoking habits. Second, since the current TNM stage is the most important factor to affect the prognosis, other factors were ruled out during the modeling procedure.
In conclusion, we could predict the individual prognosis of NSCLC patients using only clinical information and predict early recurrence in each cell type. The prediction model was reproducible and reliable. However, to improve the completeness of the prediction model, we need further study including more factors like genetic factors as well as biologic markers.
Figures and Tables
Fig. 1
This shows subgroups of patients. Among 1,578 patients, 1,433 patients had adenocarcinoma or squamous cell carcinoma, and 688 patients were detected recurred disease during follow-up period.
*, The early recurrence group is defined as patients who had recurred diseases detected within one year posteperatively; †, The non-recurrence group is defined as the survivors who were recurrence-free more than three years after curative surgery.
Fig. 2
Recurrence-free survival as a result of prediction in each cell types. Both (A) training set and (B) test set were divided into a high- and a low-risk groups significantly by our prediction model.

Table 1
Clinicopathologic characteristics of the all 1,578 patients with non-small cell lung cancer and who underwent complete resection

Table 2
Univariate and multivariate analyses of 1,578 patients using Cox's proportional hazard regression model

References
1. Bennett WP, Hussain SP, Vahakangas KH, Khan MA, Shields PG, Harris CC. Molecular epidemiology of human cancer risk: gene-environment interactions and p53 mutation spectrum in human lung cancer. J Pathol. 1999. 187:8–18.
2. Mountain CF. Revisions in the international system for staging lung cancer. Chest. 1997. 111:1710–1717.

3. Nesbitt JC, Putnam JB Jr, Walsh GL, Roth JA, Mountain CF. Survival in early-stage non-small cell lung cancer. Ann Thorac Surg. 1995. 60:466–472.

4. Park I, Kim DJ, Chung KY, Kim KD, Joo HC. Risk factors for recurrence in completely resected pT1/2N1 non-samll cell lung cancer. Korean J Thorac Cardiovasc Surg. 2005. 38:421–427.
5. Arriagada R, Bergman B, Dunant A, Le Chevalier T, Pignon JP, Vansteenkiste J. Cisplatin-based adjuvant chemotherapy in patients with completely resected non-small-cell lung cancer. N Engl J Med. 2004. 350:351–360.

6. Winton T, Livingston R, Johnson D, Rigas J, Johnston M, Butts C, Cormier Y, Goss G, Inculet R, Vallieres E, Fry W, Bethune D, Ayoub J, Ding K, Seymour L, Graham B, Tsao MS, Gandara D, Kesler K, Demmy T, Shepherd F. Vinorelbine plus cisplatin vs. observation in resected non-small-cell lung cancer. N Engl J Med. 2005. 352:2589–2597.

7. Brundage MD, Davies D, Mackillop WJ. Prognostic factors in non-small cell lung cancer: a decade of progress. Chest. 2002. 122:1037–1057.
8. Potti A, Mukherjee S, Petersen R, Dressman HK, Bild A, Koontz J, Kratzke R, Watson MA, Kelley M, Ginsburg GS, West M, Harpole DH Jr, Nevins JR. A genomic strategy to refine prognosis in early-stage non-small-cell lung cancer. N Engl J Med. 2006. 355:570–580.

9. Pfannschmidt J, Muley T, Bulzebruck H, Hoffmann H, Dienemann H. Prognostic assessment after surgical resection for non-small cell lung cancer: experiences in 2083 patients. Lung Cancer. 2007. 55:371–377.

10. Abel U, Berger J, Wiebelt H. CRITLEVEL: an exploratory procedure for the evaluation of quantitative prognostic factors. Methods Inf Med. 1984. 23:154–156.

11. Birim O, Kappetein AP, Waleboer M, Puvimanasinghe JP, Eijkemans MJ, Steyerberg EW, Versteegh MI, Bogers AJ. Long-term survival after non-small cell lung cancer surgery: development and validation of a prognostic model with a preoperative and postoperative mode. J Thorac Cardiovasc Surg. 2006. 132:491–498.

12. Harpole DH Jr. Prognostic modeling in early stage lung cancer: an evolving process from histopathology to genomics. Thorac Surg Clin. 2007. 17:167–173.

13. Padilla J, Calvo V, Penalver JC, Zarza AG, Pastor J, Blasco E, Paris F. Survival and risk model for stage IB non-small cell lung cancer. Lung Cancer. 2002. 36:43–48.

14. Charloux A, Hedelin G, Dietemann A, Ifoundza T, Roeslin N, Pauli G, Quoix E. Prognostic value of histology in patients with non-small cell lung cancer. Lung Cancer. 1997. 17:123–134.

15. Khan OA, Fitzgerald JJ, Field ML, Soomro I, Beggs FD, Morgan WE, Duffy JP. Histological determinants of survival in completely resected T1-2N1M0 nonsmall cell cancer of the lung. Ann Thorac Surg. 2004. 77:1173–1178.

16. Okamoto T, Maruyama R, Suemitsu R, Aoki Y, Wataya H, Kojo M, Ichinose Y. Prognostic value of the histological subtype in completely resected non-small cell lung cancer. Interact Cardiovasc Thorac Surg. 2006. 5:362–366.

17. Yokouchi H, Kodama K, Higashiyama M, Takami K. Prognostic assessment of resected lung cancer based on the new international staging system: analysis by histologic types. Kyobu Geka. 2000. 53:899–904.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download