Abstract
Although unilateral antegrade selective cerebral perfusion (UASCP) is considered a safe cerebral protection strategy during aortic surgery, an optimum temperature remains to be defined. This study compared outcomes in patients undergoing UASCP at either <24℃ or ≥24℃. Between 2000 and 2007, 104 consecutive patients underwent aortic surgery using UASCP. Patients were divided into two groups according to systemic temperature: group A comprised 64 patients undergoing deep hypothermia (<24℃); and group B comprised 40 patients undergoing moderate hypothermia (≥24℃). Both groups were similar in terms of the extent of aortic replacement and mean UASCP time. The total cardiopulmonary bypass time and aortic cross clamp time were longer in group A. Both groups were similar in terms of 30-day mortality rate (9.4% group A, 10.0% group B), and in terms of temporary (6.7% group A, 7.7% group B) and permanent (11.3% group A, 2.6% group B) neurological deficits. Multivariate analysis showed preoperative shock status was a risk factor for in-hospital mortality, and a preoperative history of a cerebral incident was a risk factor for permanent neurological deficit. UASCP under moderate hypothermia is a relatively safe and effective cerebral protective strategy during aortic surgery.
Strategies for cerebral protection during aortic surgery include deep hypothermic circulatory arrest (DHCA), retrograde cerebral perfusion (RCP), and antegrade selective cerebral perfusion (ASCP) (1-3). ASCP is considered the best of these methods, and various ASCP approaches are used depending on surgeon preference (3-5). The two major issues surrounding the use of ASCP are the adequacy of unilateral perfusion for the contralateral hemisphere, and the ideal degree of systemic hypothermia.
Unilateral antegrade selective cerebral perfusion (UASCP) through the axillary artery has been used by several groups with excellent clinical results. During UASCP the left hemisphere blood supply is provided not only by intracranial collateral circulation ("circle of Willis") but also from an extracranial vascular bed mostly dependent on the external carotid arteries (6, 7). The risk of hypoperfusion via UASCP can be minimized using preoperative magnetic resonance angiography (MRA), intraoperative cranial Doppler study, and assessment of backflow through the left common carotid artery and left subclavian artery during surgery.
To assist in identifying the optimum UASCP temperature, the present study assessed postoperative neurological outcomes following UASCP and aortic surgery at either <24℃ or ≥24℃.
Between March 2000 and November 2007, 104 consecutive patients underwent aortic surgery and UASCP with or without other procedures. Patients undergoing bilateral antegrade selective cerebral perfusion (BASCP) or RCP were excluded from the study.
Patients were divided into two groups according to the systemic temperature used: group A=64 patients treated using deep hypothermia (<24℃; mean temperature 18.4±2.1℃); group B=40 patients treated using moderate hypothermia (≥24℃; mean temperature 25.2±1.9℃).
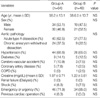
The preoperative clinical features for each group are presented in Table 1. For both groups, the main surgical indications were acute type A dissection and chronic aortic aneurysm, while other preoperative conditions did not differ between the groups.
Arterial pressure, systemic temperature, and brain protection were monitored. Double arterial monitoring was used, where the right radial artery was used for monitoring right innominate arterial perfusion, and the left femoral artery was used for systemic body perfusion. Esophageal and rectal probes were inserted to monitor systemic temperature. Cerebral oximetry and bispectral index monitoring were performed to reflect brain perfusion.
A median sternotomy was performed in 102 patients (98.1%) and a left anterior thoracotomy was performed in 2 patients (2.1%) for arch and descending aorta replacement. The right axillary artery was exposed through a subclavicular incision and cannulated with an 8 mm vascular graft after systemic heparinization (300 IU/kg). Cardiopulmonary bypass (CPB) was initiated using a double venous cannulation, after which three arch vessels were dissected and encircled with loops. Myocardial protection was established using antegrade selective blood cardioplegia, and maintained using continuous retrograde blood cardioplegia via the coronary sinus. In the absence of significant atherosclerotic change in the ascending and aortic arch, an aortic cross clamp was performed before inducing hypothermia. Procedures such as proximal anastomosis, Bentall procedure, and coronary artery bypass surgery were performed once the systemic temperature was lowered.
UASCP was commenced at a rate of 10 mL/kg/min after clamping of the right innominate artery and left common carotid artery, and the right radial arterial pressure was monitored (≒50 mmHg). During distal aortic anastomosis, systemic perfusion to the lower body was arrested. Any sign of inadequate left cerebral perfusion (i.e., low level of left cerebral oxymeter or BIS and poor backflow from the left subclavian artery) resulted in prompt conversion to bilateral cerebral perfusion with an additional 16Fr. Foley catheter into the left common carotid artery. BASCP cases were excluded from the present study.
Open distal anastomosis was performed in most cases. In the case of total arch replacement, distal lower body perfusion and rewarming was commenced following completion of the anastomosis of the three arch vessels.
Temporary neurologic dysfunction was defined as the presence of symptoms such as confusion, agitation, and delirium that resolved before discharge. Permanent neurological deficit was defined as a stroke with persistent localizing neurological deficit and a new defect according to computed tomography (CT) or magnetic resonance image (MRI). Mental recovery time was defined as the time when a patient could obey a command after spontaneous eye opening.
Descriptive statistics for technological quantities are presented as mean±standard deviation. Student's t-tests were used for comparisons between groups. Independent risk factors for in-hospital mortality and neurological outcome were derived from pre- and postoperative variables and analyzed using multivariate analysis involving a stepwise logistic regression model. All statistical analysis was performed using SPSS software (version 12.0), and P values <0.05 were considered to indicate significance.
Groups A and B were similar in terms of the extent of aortic replacement, except that hemiarch replacement was more common in Group B (62.5% group A, 82.5% group B; P=0.046). The groups were also similar in terms of the rate of concomitant procedures (Table 2).
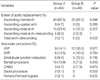
Although mean UASCP times were similar for both groups (56.3±40.1 min in group A, 46.9±35.5 min in group B; P=0.239), the total cardiopulmonary bypass time (274.7±119.5 min in group A, 190.2±76.5 min in group B; P<0.001) and aortic cross clamp time (157.5±79.4 min in group A, 118.3±45.6 min in group B; P=0.002) were longer in group A (Table 3).
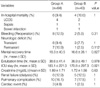
The two groups were similar in terms of 30-day mortality rates (9.4% in group A, 10.0% in group B) and causes of death (Table 4). Postoperative bleeding requiring surgical revision occurred in 8 (12.5%) in group A and 2 (2.5%) in group B patients (P>0.05).
Mental recovery, ventilator, and ICU stay times were similar for both groups. Both groups were similar in terms of the incidence of temporary (6.7% in group A, 7.7% in group B) and permanent (11.3% in group A, 2.6% in group B) neurological deficits. The overall incidence of other complications did not differ between the two groups (Table 4).
Multivariate analysis showed that preoperative shock status was a risk factor for in-hospital mortality (odds ratio 7.07, 95% confidence interval: 1.3-38.2), and a preoperative history of a cerebrovascular incident was a risk factor for a permanent neurological deficit (odds ratio 8.99, 95% confidence interval: 1.6-50.2). There were no independent determinants for temporary neurological deficit (Table 5).
DeBakey and colleagues (8) first applied ASCP using direct cannulation of arch vessels in 1957, and this technique has become the preferred method for many surgeons for brain protection during aortic surgery.
A standard ASCP method has not been established, and ASCP can be applied unilaterally or bilaterally under different hypothermic conditions. Surgeons at our institution routinely use right axillary cannulation for aortic surgery, and the physiological level of perfusion pressure and the monitoring systems follow closely those described by Dr. Kazui et al. (9, 10). However, we prefer to use UASCP with clamping of the left common carotid artery.
Controversy surrounds the adequacy of UASCP for contralateral cerebral perfusion. Spielvogel and colleagues (11) reported that UASCP was inadequate for aortic arch replacement, in contrast with the excellent outcomes using BASCP under deep hypothermia. Dr. Kazui (12) also questioned the safety of UASCP for cerebral, spinal cord and visceral perfusion, although he suggested UASCP may be a good substitute for DHCA in cases of hemiarch replacement.
BASCP is a widely used cerebral protective strategy during aortic surgery. While it provides greater time for complex and extensive aortic procedures, the main drawbacks are that it may clutter the surgical field, injure the arch vessel related with cannulation, and increase the risk of particulate embolization.
Perfusion of the contralateral hemisphere during UASCP depends on an uninterrupted circle of Willis channel. Using angiography and silicone casts, Merkkola and associates (13) demonstrated in 87 cadavers that when the right axillary artery is used for perfusion, circulation to the left side appears to be good in most cases. Using magnetic resonance imaging on an Italian population, Macchi and associates (14) demonstrated that the anterior communicating artery was absent in 3% of the population, and that hypoplasia of both anterior and posterior communicating arteries existed in approximately 2% of cases. Hypothetically, the absence of one of three communicating arteries does not carry any risk for hypoperfusion because the blood coursing through the right upper brachial artery will perfuse the whole brain through the vertebral, basilar, and internal carotid arteries. The only combination that will carry the potential for contralateral hypoperfusion would be the absence of both anterior and posterior communicating arteries, and even if that is the case, only the frontal and temporal regions of the left hemisphere would be affected. This specific combination has not been mentioned in the literature, suggesting it is a very rare condition.
During the study period, 3 cases required conversion from UASCP to BASCP due to a decrease in brain oximetry on the left cerebral hemisphere. All of the patients recovered without neurological problem. The postoperative brain MRI showed mild intracaranial vascular atherosclerosis which had no significant consequence except in one patient in which a prompt drop in cerebral oximetry was noted after initiation of UASCP. The patient's brain MRA showed complete interruption of right internal carotid artery, which was subsequently revascularized by stent insertion, demonstrating a rare case in which UASCP may fail to provide sufficient protection to the contralateral hemisphere (Fig. 1). Based on our clinical experience, carotid arterial disease has been found to be associated with a higher risk of hypoperfusion to the contralateral hemisphere during UASCP than the absence of the three communicating arteries. Significant carotid artery disease may be readily detected by preoperative MRA or carotid Doppler study. However, in acute type A dissection the urgency of the situation or the odd hours in which the patients are presented usually result in practical limitations which make these studies unavailable. Similarly in the more than 70% of patients presenting with acute type A dissection in the current series, surgery was performed without preoperative carotid artery studies.
In our experience, conversion to BASCP was easily performed by preparing an additional cannulation line and insertion of another catheter to left common carotid artery a few seconds. But, we do not agree routine use of BASCP, as mentioned above, because of its drawbacks during operation.
Another issue for ASCP is the determining ideal level of systemic hypothermia. While deep hypothermia provides a safe period for the procedure, the extensive cooling and rewarming periods not only prolong the already long CPB and operating times, but also increase negative side-effects of CPB which can influence postoperative outcomes.
Cerebral oxygen consumption decreases by 50-60% at a core temperature of 25-28℃, and further cooling does not decrease brain oxygen consumption (15, 16). However, the regional cerebral blood flow with antegrade perfusion decreases to 62% of baseline at 28℃ and to 36% at 18℃ (17).
Previous studies showed excellent clinical and neurological outcomes with ASCP under moderate hypothermia (6, 7, 18, 19). In the present study, the clinical and neurological outcomes under moderate hypothermia were comparable to those under deep hypothermia. The clinical results by Kazui and colleagues (20) investigating ASCP and moderate hypothermia indicated that a period of 90 min was safe in terms of spinal cord protection and hepatic and renal function preservation. In the present study, the period of lower body ischemia was less than 60 min for both groups, and there was no spinal ischemia. Each group had one case of bowel infarction, and this was due to malperfusion syndrome after type A aortic dissection, and not due to hypoperfusion during surgery.
The present clinical and neurological outcomes were comparable to other similar studies. Most mortality cases were associated with a preoperative shock status due to a long arrival time from other hospitals. In addition, patients with permanent neurological deficits had a previous history of cerebral vascular incidents that are significant risk factors. The transient neurological deficits were simple delirium while in the intensive care unit.
The current study was retrospective in design and involved a relatively small number of patients. Despite these limitations, the study indicates that UASCP is a relatively safe and effective cerebral protective strategy during aortic surgery in terms of hospital mortality and neurological outcomes. Possible hypoperfusion of the left hemisphere can be monitored, and prompt conversion to BASCP is mandatory when warning signs occur. Additional brain protection measures may be necessary in patients who had history of cerebral vascular incidents. Further randomized prospective studies are necessary to identify the optimal systemic temperature.
In conclusion, moderate systemic hypothermia appears to be safe and also beneficial for reducing cardiopulmonary bypass time and hypothermia-related side effects.
Figures and Tables
Fig. 1
Postoperative brain magnetic resonance angiography showing complete obstruction of the right internal carotid artery.

References
1. Griepp RB, Stinson EB, Hollingsworth JF, Buehler D. Prosthetic replacement of aortic arch. J Thorac Cardiovasc Surg. 1975. 70:1051–1053.
2. Ueda Y, Miki S, Kusuhara K, Okita Y, Tahata T, Yamanaka K. Surgical treatment of aneurysms or dissections involving the ascending aorta and aortic arch, utilizing circulatory arrest and retrograde cerebral perfusion. J Cardiovasc Surg (Torino). 1990. 31:553–558.
3. Kazui T, Kimura N, Yamada O, Komatsu S. Surgical outcome of aortic arch aneurysms using selective antegrade perfusion. Ann Thorac Surg. 1994. 57:904–911.
4. Griepp RB. Cerebral proctection during aortic arch surgery. J Thorac Cardiovasc Surg. 2001. 121:425–427.
5. Di Eusanio M, Schepens MA, Morshuis WJ, Dossche KM, Di Bartolomeo R, Pacini D, Pierangeli A, Kazui T, Ohkura K, Washiyama N. Brain protection using antegrade selective cerebral perfusion: a multicenter study. Ann Thorac Surg. 2003. 76:1181–1189.

6. Kucuker SA, Ozatik MA, Saritas A, Tasdemir O. Arch repair with unilateral antegrade cerebral perfusion. Eur J Cardiothorac Surg. 2005. 27:638–643.

7. Panos A, Murith N, Bednarkiewicz M, Khatchatourov G. Axillary cerebral perfusion for arch surgery in acute type A dissection under moderate hypothermia. Eur J Cardiothorac Surg. 2006. 29:1036–1039.

8. DeBakey ME, Crawford ES, Cooley DA, Morris GC Jr. Successful resection of fusiform aneurysm of aortic arch with replacement by homograft. Surg Gynecol Obstet. 1957. 105:657–664.
9. Tanaka H, Kazui T, Sato H, Inoue N, Yamada O, Komatsu S. Experimental study on the optimum flow rate and pressure for selective cerebral perfusion. Ann Thorac Surg. 1995. 59:651–657.

10. Kazui T, Washiyama N, Muhammad BA, Terada H, Yamashita K, Takinami M, Tamiya Y. Total arch replacement using aortic arch branched grafts with the aid of antegrade selective cerebral perfusion. Ann Thorac Surg. 2000. 70:3–9.

11. Spielvogel D, Etz CD, Silovitz D, Lansman SL, Griepp RB. Aortic arch replacement with a trifurcated graft. Ann Thorac Surg. 2007. 83:S791–S795.

12. Kazui T. Editorial comment: which is more appropriate as a cerebral method-unilateral or bilateral perfusion? Eur J Cardiotherac Surg. 2006. 29:1039–1040.
13. Merkkola P, Tulla H, Ronkainen A, Soppi V, Oksala A, Koivisto T, Hippelainen M. Incomplete circle of Willis and right axillary artery perfusion. Ann Thorac Surg. 2006. 82:74–79.

14. Macchi C, Catini C, Federico C, Gulisano M, Pacini P, Cecchi F, Corcos L, Brizzi E. Magnetic resonance angiographic evaluation of circulus arteriosus cerebri (circle of Willis): a morphologic study in 100 human healthy subjects. Ital J Anat Embryol. 1996. 101:115–123.
15. McCullough JN, Zhang N, Reich DL, Juvonen TS, Klein JJ, Spielvogel D, Ergin MA, Griepp RB. Cerebral metabolic suppression during hypothermic circulatory arrest in humans. Ann Thorac Surg. 1999. 67:1895–1899.

16. Ehrlich MP, McCullough JN, Zhang N, Weisz DJ, Juvonen T, Bodian CA, Griepp RB. Effect of hypothermia on cerebral blood flow and metabolism in the pig. Ann Thorac Surg. 2002. 73:191–197.

17. Usui A, Oohara K, Murakami F, Ooshima H, Kawamura M, Murase M. Body temperature influences regional tissue blood flow during retrograde cerebral perfusion. J Thorac Cardiovasc Surg. 1997. 114:440–447.

18. Jacobs MJ, de Mol BA, Veldman DJ. Aortic arch and proximal supraaotic arterial repair under continous antegrade cerebral perfusion and moderate hypothermia. Cardiovasc Surg. 2001. 9:396–402.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download