INTRODUCTION
Stress urinary incontinence (SUI) is defined by the International Continence Society as the complaint of involuntary urinary leakage on effort or exertion, or on sneezing or coughing (
1). The causes of SUI are urethral hypermobility, in which there is laxity of pelvic floor support, and intrinsic sphincter dysfunction caused by the inability of the urethral sphincter itself to close (
2). One well-accepted technique for surgical management of urethral hypermobility is the open Burch colposuspension (
3-
5).
In an effort to reduce the morbidity associated with open surgical procedures, the laparoscopic bladder neck suspension was first described by Vancaille and Schuessler (
6). Since then, there have been numerous reports on the results of laparoscopic colposuspensions (
7). However, there are not many reports on the long-term outcomes of laparoscopic colposuspensions. The purpose of this study was to present the long-term results of laparoscopic Burch colposuspension for SUI.
MATERIALS AND METHODS
From September 1995 to August 1999, extraperitoneal laparoscopic Burch colposuspension was performed by an operator on 99 women, all of whom suffered from SUI or mixed urinary incontinence. The colposuspension was exclusively performed by non-absorbable sutures. All women had urodynamically proven SUI. Idiopathic detrusor overactivity was not an exclusion criterion. None of the patients had undergone any previous anti-incontinence operations, except one who had undergone an anterior colporrhaphy. Women with pure intrinsic sphincter dysfunction (abdominal leak point pressure less than 60 cm H
2O), severe degrees of combined pelvic organ prolapse were not considered candidates for this procedure. The preoperative evaluation of all the patients included a history, SEAPI-QMM incontinence classification system (
8), urinalysis and urine culture, physical examination, cough stress test, voiding cystourethrography (
9), and full urodynamic assessment. We retrospectively reviewed the medical records and symptom questionnaires, including the SEAPI incontinence classification, time to recurrence of stress incontinence, and subjective satisfaction, either by a mail or telephone interview. Stress-related leakage determined by patient's history of urine loss during physical activity was scored as follows; S0=no urine loss, S1=loss with strenuous activity, S2=loss with moderate activity, S3=loss with minimal activity or gravitational incontinence (
8). The follow-up period was undertaken at a single point in time. A total of 68 patients, who were contacted and followed-up for more than 3 yr, were included in this study.
Surgical result was evaluated by cough stress test with a comfortably full bladder and symptoms questionnaire. The outcome of surgical treatment was divided into the three groups: Cured, improved, and failed. The patients were considered to be cured of SUI if they had a negative cough stress test result and there were no reports of urine leakage during physical exertion. The patients who were considered to be improved were those who did not leak on the cough stress test but may have had occasional urine leakage during stress. This occasional leakage did not, however, influence their daily activities and require any further treatment. Patients who did not meet these criteria were considered to be failed. Patients were asked to describe their overall satisfaction with the surgical outcome, with three possible choices: very satisfied, satisfied, or not satisfied. All patients, except those not satisfied, were considered as having been satisfied.
The procedure was performed with the patient under general anesthesia in a dorsal lithotomy position. A 16-Fr Foley catheter was inserted preoperatively. The laparoscopic Burch colposuspension was performed through an extraperitoneal approach. A midline 1.5 cm incision was made just below the umbilicus. The preperitoneal distention balloon (PDB) cannula (Origin Medsystems; Menlo Park, CA, U.S.A.) was inserted along the posterior rectus sheath toward the pubis. A 10-mm Hasson-style blunt tip balloon trocar (Origin Medsystems) with a 0-degree laparoscope was introduced after expansion of the Retzius space by balloon pumping. Two additional 5 mm trocars were placed, one in each lower quadrant at a point one third lateral to the rectus muscle. With insufflation of carbon dioxide at a pressure of 8-10 mmHg, the bladder was mobilized and the periurethral fat was cleared from the pubocervical fascia. Cooper's ligaments were exposed and cleansed of the surrounding areolar tissue and fat.
All the patients underwent laparoscopic Burch colposuspension had same types of fixation: we placed two paravaginal non-absorbable sutures (1-0 polypropylene) on each side. The sutures between the anterior vaginal wall and Cooper's ligament were placed 2 cm laterally on each side of the urethra and 2 cm distal to the bladder neck, which is the technique described by Tanagho (
10). An intraoperative cystoscopy was performed on all the women at the end of the procedure to exclude any urethral and bladder injuries. The Foley catheter was removed 24 hr after the operation, and then intermittent self-catheterizations were performed until the postvoid residual urine was less than 50 mL.
Normally distributed continuous variables were analyzed using the unpaired Student's t-test. Continuous variables that were not normally distributed were analyzed using the non-parametric Mann-Whitney U-test. Categorical variables were compared using the chi-square test or Fisher's exact test. As time passed, the accumulated cure rates were assessed by using a Kaplan-Meier survival analysis and were compared by using the log-rank test. The statistical significance was set at P<0.05.
RESULTS
The preoperative characteristics of the patients are summarized in
Table 1. Of the total number of patients, urge urinary incontinence was combined in 21 (30.9%). In 5 patients (7%), detrusor overactivity was demonstrated on urodynamic evaluations. A total of 54 (79.4%) patients reported that they used of pads daily for protection from incontinence.
The cure and improvement rates following laparoscopic Burch colposuspension were 72.1% and 20.6% respectively, with a mean follow-up period of 51.6 months (range, 36 to 83 months). The overall satisfaction rate was 82.3%. The comparison of the cured group (S0) with the non-cured group (S1 or S2), based on the various clinical parameters, is shown in
Table 2. There were no significant differences in the demographic parameters, urodynamic findings, and peri-operative characteristics between the groups. The cure rate tended to be lower in initial 20 cases than subsequent cases. However, there was a difference in the mean follow-up period between the earlier group and the latter group (70.6 months vs. 51.6 months;
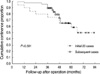
P<0.001). Therefore, the actuarial cure rates were determined by survival analysis, and were compared between the groups (
Fig. 1). According to the result of survival analysis, there is no statistical difference between the initial and subsequent cases (
P=0.591, log-rank test). The cure rate was inversely related to the time interval following the colposuspension. When the results were analyzed based on the duration of the follow-up period, the cure rates indicated that the patients tended to develop urinary leakage considerably 4 yr after their surgeries.
Of the 54 patients who required pads preoperatively, 49 (90.7%) no longer required the routine application of pad. Detrusor overactivity was demonstrated in 5 patients on preoperative urodynamic evaluations. Among these patients, two patients were freed from urge incontinence. Of the 21 patients with preoperative urge urinary incontinence, 13 (61.9%) demonstrated postoperative dissipation of symptoms. But, 3 patients (6.4%) developed de novo urge urinary incontinence. All the patients with de novo urge urinary incontinence experienced a resolution of symptoms after undergoing medication with antimuscarinic agent. Eight patients (11.8%) required a longer time to regain complete bladder emptying, but their voiding ability returned within 3 weeks postoperatively. One patient received a pubovaginal sling because of recurrent urinary leakage 40 months postoperatively.
There were operative-related complications documented in 3 (4.4%) patients: bleeding at the port site in one, a peritoneal laceration in one, and respiratory acidosis in one. All of them recovered without any major surgical manipulation.
DISCUSSION
The open Burch colposuspension, first described in 1961 (
3), had been widely employed for the surgical treatment of women with SUI caused by urethral hypermobility. A long-term series of Burch colposuspensions have demonstrated excellent durability (
4,
5). Lapitan et al. (
11) reviewed 33 trials that involved a total of 2,403 women, who underwent open retropubic colposuspensions and found an overall cure rate between 68.9% and 88.0%. They reported that the overall continence rates were approximately 85-90% within the first year and 70% after five years of treatment.
Since the early 1990s, laparoscopic colposuspension has emerged as a treatment modality in an effort to reduce the surgical morbidity associated with the open Burch colposuspension and to achieve a comparable cure rate (
6,
12). There are more than 150 published reports about laparoscopic colposuspensions. However, the long-term outcomes of laparoscopic colposuspension are uncertain, due to the limited duration of follow-up in most series. In 2006, the Cochrane Incontinence Group suggested that the laparoscopic colposuspension may be as good as open colposuspension at two years post surgery according to the currently available data (
13).
The overall long-term results of our study indicated that 72% of patients were cured by the laparoscopic Burch colposuspension with a mean follow-up of 52 months. Of the total patients, 34 (50%) had at least 4 yr of follow-up. However, we could obtain subjective information on approximately 70% of all patients who were performed laparoscopic colposuspension during the same period. If we assume that all patients who missed data were considered to be failed, cure rate decreased to 50%. Although subjective cure rate was comparable with previously reported open Burch series by 24 months, it tended to decrease steadily over time (
Fig. 1). It was more pronounced 4 yr after surgery. These findings suggest that the cure rate with laparoscopic colposuspension is inferior to the open procedure when the duration of the follow-up period is extended. The poorer outcomes might be related to the failure of the laparoscopic technique to adhere exactly to the same anatomical principles as the open procedure.
It is unclear whether the steep learning curve associated with laparoscopic Burch colposuspension affects the long-term outcomes. In the present study, there was a trend for operation time to be longer in the initial 20 cases than subsequent series (mean, 115 min vs. 87 min, respectively;
P=0.062). But after the initial 20 cases, the operation time was similar throughout the remainder of study. As previously mentioned, we did not find any statistical difference of cure rates when divided into early 20 cases and the latter cases. Therefore, the surgeon's performance with the laparoscopic approach may not affect the long-term results. Rather, the time after the colposuspensions was more important than the other variables in the assessment of the cure rates. In addition, this time-dependent outcome was demonstrated in the long-term follow-up cases of open Burch colposuspensions (
4).
Lower cure rates in the laparoscopic colposuspension have been reported previously when fewer than two sutures were used or when mesh, instead of sutures, was utilized for the fixation to Cooper's ligament (
14-
17). We had utilized polypropylene surgical mesh and tacks in the early cases of laparoscopic colposuspension. Therefore, an operator had an experience of approximately 30 laparoscopic colposuspension with mesh at the start of this study. In this study, we had routinely placed two paravaginal sutures on each side. We did not include the outcomes of mesh using group in terms of cure rate for laparoscopic colposuspension because it might act as a confounding bias.
The results of randomized controlled trial comparing the laparoscopic colposuspension and open procedure were recently reported (
18,
19). A total of 227 women received a laparoscopic and 247 women an open colposuspension. These two trials had 24 months of follow-up on approximately 80% of all randomized women. They showed that laparoscopic colposuspension has comparable outcomes in mid-term follow-up. The objective cure (negative 1-hr pad test) rates for open and laparoscopic were 70% and 80% in COLPO (Colposuspension; is Laparoscopic Preferable to Open?) Trial with 24-month data (
19).
There are several limitations of this study. First, our study design was not a comparative study, but a case series. In general, case series are retrospective in nature and any form of bias may have an influence on the interpretation of the results. Second, there was no consideration given to the objective measurement of clinical efficacy. Only subjective outcomes were conducted, either by a postal questionnaire or telephone interview. Although the patient's perception is more important than the physician's assessment when incontinence-related problems are evaluated (
20), this may cause some difficulty in understanding the true outcome. Lastly, we obtained the time to recurrent incontinence by tracing back in the patient's memory. Thus, the time lapse to urinary leakage may not represent the actual time because patients might have difficulty to trace back the real time of failure.
Over the last decade, laparoscopic colposuspension has been performed due to its benefits, such as a low morbidity, quicker recovery, and short-term outcomes that are equivalent to the open procedure. Recently, a number of new, minimally invasive procedures for anti-incontinence surgery have been developed, due to the requirements of both the patients and physicians. The mid-urethral sling procedure has become a well established, less invasive surgery for the management of stress urinary incontinence. The objective cure rate appears to be in favor of the mid-urethral slings compared with laparoscopic colposuspension (
13). At the present time, when considering the indications for laparoscopic colposuspension, it may be the treatment of choice in special situations. First, when concomitant pelvic floor reconstruction is being performed, laparoscopic colposuspension in conjunction with paravaginal repair can correct anterior compartment prolapse (
21). Second, when concomitant pelvic surgery such as hysterectomy or ovariectomy is being performed, laparoscopic colposuspension can be performed with the same route. Third, current meshs are foreign bodies and have potential complications of mesh erosion over time. Therefore, laparoscopic colposuspension avoids the potential, long-term complications of mesh in childbearing young women or patients with poor vaginal tissue vascularity due to high risk of mesh erosion. Lastly, laparoscopic colposuspension might be another option for women after failed suburethral tape procedure (
22). In fact, the frequency of laparoscopic colposuspension has markedly decreased. However, we could not overlook both its historical significance as a less invasive surgical treatment for SUI and possible role in a selected patient.
Out of the 68 patients who underwent laparoscopic Burch colposuspensions, more than two thirds were cured, with a mean follow-up period of 52 months. There was no significant difference between the continent and incontinent group in terms of clinical variables. The outcomes of laparoscopic Burch colposuspensions were time-dependent. Although the cure rate was comparable with open Burch by mid-term, it decreased significantly 4 yr after the procedures. Based on these results, we suggest that long-term follow-up is necessary when evaluating the clinical efficacy of anti-incontinence surgery.






 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download