Abstract
The aim of this study was to compare the rate of incomplete resection and treatment outcome of the second-pass technique with those of single-pass technique in loop electrosurgical excisional procedure (LEEP). From 1997 to 2002, 683 women were diagnosed as squamous dysplasia via LEEP in our institution. Age, parity, LEEP technique, grade of lesion, glandular extension, margin status, residual tumor and recurrence were obtained by reviewing medical records. Positive margin was defined as mild dysplasia or higher grade lesions at resection margin of the LEEP specimen. In women who underwent hysterectomy, residual tumor was defined as mild dysplasia or higher grade lesions in hysterectomy specimen. In women who did not underwent hysterectomy, Pap smear more than atypical squamous cells of undetermined significance or biopsy result more than mild dysplasia within two years after LEEP were regarded as cytologic or histologic recurrences, respectively. Treatment failure of LEEP was defined as residual tumor or histologic recurrence. The second-pass technique significantly reduced the endocervical margin positivity (odds ratio [OR], 0.36; 95% confidence interval [CI], 0.21-0.63). However, the second-pass technique did not reduce the treatment failure (OR, 0.62; 95% CI, 0.29-1.32). In conclusion, the second-pass technique markedly reduced the endocervical margin positivity, but did not reduce the treatment failure rate of LEEP.
Due to its many advantages over other techniques, the loop electrosurgical excisional procedure (LEEP) is the most popular method for treating and diagnosing cervical dysplasia in the United States (1). The LEEP is technically easy, requires short operation time, has a low complication rate, and can be done in the office setting. However, LEEP also has some disadvantages. For example, deep endocervical lesions are hard to remove with a single pass of a loop. Therefore, for deep endocervical lesions, some authors reported use of a second pass with a smaller-diameter loop (2-5). The second-pass technique is also known as "apical excision", "top hat shaped excision", and "LEEP-cone" (1).
Because more endocervical tissues are removed, the second pass technique has been believed to reduce the incomplete resection than the conventional single-pass technique. In addition, the second-pass technique has been shown to be equivalent to a cold-knife conization if performed properly (6). However, to our knowledge, there have been few studies that compared the second-pass technique with the single-pass technique.
We hypothesized that, compared to the single-pass technique, the second-pass technique could reduce the incomplete resection and treatment failure of LEEP. The aim of this study was to compare the incomplete resection rate and treatment outcome of second-pass technique with those of single-pass technique.
Between January 1997 and June 2002, 683 women were diagnosed as squamous dysplasia via LEEP in our institution. The LEEP was performed with a variable sized loop electrode. LEEP technique was chosen considering the location of lesion, the size and shape of cervix, the plan for childbearing, and the operators' preferences. When the second-pass technique was used, specimens from the first- and second-passes were labeled separately. The orientation of specimens was indicated using a stitch on anterior, exocervical margin of a specimen.
Age, parity, LEEP technique, grade of lesion, glandular extension, and margin status were obtained by reviewing medical records. In women who underwent hysterectomy within three months after LEEP, the presence of residual tumor in hysterectomy specimen was investigated. In women who did not undergo immediate hysterectomy, Pap smear results within two years after LEEP were obtained. 'Adequate follow-up' was defined as three or more Pap smears within two years after LEEP. 'Inadequate follow-up' was defined as Pap smears less than three times within two years. Women with abnormal Pap smear or biopsies within two years were regarded as 'adequate follow-up' even if she received Pap smear less than three times. Pap smear more than atypical squamous cells of undetermined significance (ASCUS) was regarded as cytologic recurrence and biopsy result more than mild dysplasia was defined as histologic recurrence. Treatment failure of LEEP was defined as residual tumor in hysterectomy specimen or histologic recurrence in women who were under adequate follow-up.
All specimens were evaluated at the department of pathology. Margin status was reported as positive if mild dysplasia or higher grade lesions were present at resection margin of LEEP specimen. In women who underwent hysterectomy, the residual tumor was defined as the presence of mild dysplasia or higher grade lesions.
Results were considered statistically significant if a p value of ≤0.05 was obtained. Chi-square test and linear by linear association method were utilized to test for univariate relationships between clinicopathologic characteristics and LEEP techniques. Univariate and multivariate logistic regression analysis were used to evaluate the associations of clinicopathologic risk factors with endocervical margin positivity on LEEP specimen or treatment failure. Chi-square test and Fisher's exact test were used to evaluate the univariate associations of LEEP technique with residual tumor or recurrences. Analysis of the data was performed using SPSS for Windows Version 12 (SPSS Inc., Chicago, IL, U.S.A.).
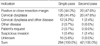
The single-pass technique was used in 550 women (80.5%) and the second-pass technique was used in 133 women (19.5%). Age distribution of single-pass group was not different from that of second-pass group (p=0.942). Records on parity were available in only 463 women (67.8%). Parity of single pass group was not different from that of second-pass group (p=0.181). The portions of mild, moderate, severe dysplasia, and carcinoma in situ (CIS) were similar between the single-pass and second-pass groups (p=0.911). Glandular extension was present in about half of women from both the single-pass and second-pass groups (p=0.866). Endocervical margin positivity was 27.6% in single-pass group and 12.8% in second-pass group (p=0.000). In the single-pass group, over half of women underwent hysterectomy within three months after LEEP. However, in the second-pass group, only one third of women underwent hysterectomy (p=0.000) (Table 1).
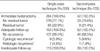
Compared to single-pass technique, the second-pass technique significantly reduced the endocervical margin positivity (odds ratio [OR], 0.36; 95% confidence interval [CI], 0.21-0.63). However, higher grade lesion and glandular extension increased endocervical margin positivities. Moderate, severe dysplasia, and CIS had about four, eight, and seventeen times more endocervical margin positivities than mild dysplasia, respectively. Glandular extension increased endocervical margin positivity nearly twice (Table 2).
Before comparing the rate of residual tumor in hysterectomy specimen, we examined the indication of hysterectomy in both groups. The indication was mainly positive resection margin or cervical dysplasia (mostly CIS) itself. The portion of each indication in single-pass group was similar with that of second-pass group (Table 3).
Rate of residual tumor or recurrence in single-pass group was similar with that of second-pass group. In women who underwent immediate hysterectomy, the rate of residual tumor was not different between two groups (p=0.833). In women with adequate follow-up, the rate of cytologic or histologic recurrence was not different between two groups (p=0.828 for cytologic+histologic recurrence; p=0.682 for histologic recurrence) (Table 4). The rate of treatment failure defined as residual tumor or histologic recurrence was similar between two groups (p=0.155, data not shown)
According to univariate and multivariate analysis, the endocervical margin positivity was the only independent risk factor for treatment failure (OR, 3.40; 95% CI, 2.00-5.80). Glandular extension was associated with treatment failure in univariate analysis (OR, 1.86; 95% CI, 1.11-3.12) but not in multivariate analysis (OR, 1.35; 95% CI, 0.78-2.33). Age, parity, grade of lesion, LEEP techniques were not associated with treatment failure (Table 5).
In this study, we showed that the second-pass technique markedly reduced the endocervical margin positivity after LEEP. It is well known that the endocervical margin positivity is a strong indicator of recurrence after LEEP (7). Therefore, we anticipated that the second-pass technique could also reduce the treatment failure after LEEP which is defined as residual tumor or histologic recurrence. However, the second-pass technique did not reduce the treatment failure. There could be some explanations. First, the small sample size could be a problem. Considering that only a small portion of women actually have residual tumor or recurrence even when the endocervical margin was positive, the sample size of this study could be insufficient to reach a statistical significance. Second, the selection bias could be a possibility. In the second-pass group, significantly fewer women underwent hysterectomy than in the single-pass group. It is possible that, by reducing the endocervical margin positivity, the second-pass technique excluded low risk women from hysterectomy. As a result, among the 326 women who underwent the hysterectomy, the second-pass group may contain relatively more high risk women than the single-pass group. Third, skipped lesions could have been present. A study about the second-pass technique also reported that the second-pass did not reduce the recurrences (7). In addition, the cold knife conization resecting nearly twice more tissue than LEEP did not reduce the residual tumor in hysterectomy specimen (8). These results could be easily explained by assuming skipped lesions.
We also confirmed that the higher grade lesion and the glandular extension were indicators of the endocervical margin positivity. In addition, endocervical margin positivity was an indicator of treatment failure after LEEP. These findings were roughly concordant with the previous studies (9-12).
Although the second-pass technique seemed to have some advantages over single-pass technique, the second-pass technique also has disadvantages. Because the second-pass resects more endocervical tissues, it could cause more complications such as incompetent cervix, cervical stenosis. Therefore, complete topographic evaluation of lesion before LEEP is mandatory. In addition, we thought that the second-pass technique should be cautiously used in women whose childbearing is not completed.
In conclusion, the second pass technique markedly reduced the endocervical margin positivity after LEEP, but did not reduce the residual tumor or recurrences.
Figures and Tables
References
1. Tillmanns TD, Falkner CA, Engle DB, Wan JY, Mannel RS, Walker JL, Johnson GA, McMeekin DS, Zuna R, Gold MA. Preoperative predictors of positive margins after loop electrosurgical excisional procedure-Cone. Gynecol Oncol. 2006. 100:379–384.

2. Baggish MS, Noel Y, Brooks M. Electrosurgical thin loop conization by selective double excision. J Gynecol Surg. 1991. 7:83–86.

3. Keijser KG, Kenemans P, van der Zanden PH, Schijf CP, Vooijs GP, Rolland R. Diathermy loop excision in the management of cervical intraepithelial neoplasia: diagnosis and treatment in one procedure. Am J Obstet Gynecol. 1992. 166:1281–1287.

4. Murdoch JB, Grimshaw RN, Morgan PR, Monaghan JM. The impact of loop diathermy on management of early invasive cervical cancer. Int J Gynecol Cancer. 1992. 2:129–133.

5. Vergote IB, Makar AP, Kjorstad KE. Laser excision of the transformation zone as treatment of cervical intraepithelial neoplasia with satisfactory colposcopy. Gynecol Oncol. 1992. 44:235–239.

6. Gold M, Dunton CJ, Murray J, Macones G, Hanau C, Carlson JA Jr. Loop electrocautery excisional procedure: therapeutic effectiveness as an ablation and a conization equivalent. Gynecol Oncol. 1996. 61:241–244.

7. Gonzalez DI Jr, Zahn CM, Retzloff MG, Moore WF, Kost ER, Snyder RR. Recurrence of dysplasia after loop electrosurgical excision procedures with long-term follow-up. Am J Obstet Gynecol. 2001. 184:315–321.

8. Hillemanns P, Kimmig R, Dannecker C, Noorzai T, Diebold J, Thaler CJ, Hepp H. LEEP versus cold knife conization for treatment of cervical intraepithelial neoplasias. Zentralbl Gynakol. 2000. 122:35–42.
9. Costa S, De Nuzzo M, Terzano P, Santini D, De Simone P, Bovicelli A, Bovicelli L, Bucchi L. Factors associated with cone margin involvement in CIN patients undergoing conization-equivalent electrosurgical procedure. Acta Obstet Gynecol Scand. 2000. 79:586–592.





 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download