This article has been
cited by other articles in ScienceCentral.
Abstract
The estimation of plasma hemoglobin concentration (Hb) is among one of the daily activities in the practice of clinical anesthesiology. The near-infrared spectroscopy of the brain (rSO2) represents a balance between cerebral oxygen delivery and consumption. This study was designed to assess the value of rSO2 in the prediction of the Hb level while other variables were mathematically controlled. Thirty healthy adult patients undergoing spine surgery, expected to have a moderate degree of intraoperative bleeding, were enrolled in this study. General anesthesia was given and ventilation was mechanically controlled. Measurement of Hb and PaCO2 were performed at random periods of time. We obtained a total of 97 data combinations for the 30 study patients. The Hb was regressed by independent variables including rSO2 and PaCO2. A multilinear regression analysis was performed and the final regression equation was expressed only with statistically significant variables. The measured Hb was tightly regressed with three variables. The final regression equation was Hb=+8.580+0.238 rSO2-0.338 PaCO2-0.004 anesthetic exposure duration (Tmin) (p=0.000, r2=0.809). Near-infrared spectroscopy was shown to be a valuable predictor of plasma Hb in the clinical anesthesiology setting.
Keywords: Spectroscopy, Near-Infrared, Hemoglobins, Noninvasive Monitoring
INTRODUCTION
Bleeding is inevitable during most surgical procedures and estimation of the amount of bleeding is an important part of an anesthesiologists' daily work. Anesthesiologists tend to depend on their own educated guess as an index for estimating the amount of blood loss. The plasma hemoglobin concentration (Hb) represents a standard measurement that is used to estimate blood loss and the current status of oxygen carrying capacity of arterial blood. Measurement of Hb is costly and takes a few minutes. At times, time-delay can interfere with patient management.
Research on a noninvasive in vivo estimation of Hb is very limited. In addition, the utility of any methods studied frequently requires unfamiliar instrument (
1-
3) or is applicable to very specific situations (
4-
6). We have assessed the Hb value as a factor that influences near-infrared spectroscopy referred to as cerebral oximetry, and abbreviated as rSO
2 during a series of clinical investigations using cerebral oximetry. rSO
2 is a well known important variable used to predict oxygen balance in the brain. We postulated that rSO
2 would indicate Hb levels when the cerebral metabolic rate and cerebral blood flow were assumed to be constant.
Our attempt to predict Hb noninvasively was based on a simple assumption. The values of rSO2 represent regional cerebral field oxygen saturation; these values can be confounded by several factors such as arterial oxygen saturation (SaO2), arterial carbon dioxide tension (PaCO2), and Hb levels. We have evaluated the potential usefulness of rSO2 to predict Hb levels by controlling and excluding the confounders. This study was designed to test our assumption that changes in the rSO2 can predict changes in the Hb level when PaO2 and PaCO2 are constant, and to provide a mathematical model that demonstrates the correlation of rSO2 with Hb levels during general anesthesia.
MATERIALS AND METHODS
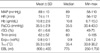
After approval from the Institutional Ethics Committee, we recruited thirty, American Society of Anesthesiologists (ASA) physical status I or II, adult patients (
Table 1) who were scheduled for elective spine surgery, with an expectation of a moderate degree of intraoperative bleeding (20-30% of estimated blood volume). Patients with cardiovascular, endocrine or cerebral disease were excluded. General anesthesia was induced with intravenous administration of propofol (1.5 mg/kg) and vecuronium (0.1 mg/kg) and inhalation of isoflurane via a face mask. The trachea was intubated and ventilation was mechanically controlled. Anesthesia was maintained with isoflurane and 50% oxygen with air and intermittent administration of vecuronium. An emitter-sensor couplet of a cerebral oximeter was attached to the right forehead.
Blood loss was estimated by naked eyes. The amount of homologous blood transfusion was not regulated but performed by in-hospital protocols. Average 2-4 repeats of blood samplings in a patient for the measurement of Hb and PaCO2 were performed by anesthesiologist's subjective judgment at irregular periods. Full arterial oxygen saturation was confirmed at every period. At the time of skin closure, the amount of blood loss was guessed by an experienced anesthesiologist, unaware of the purpose of this study. Measured Hb and PaCO2 were recorded alongside of rSO2, esophageal temperature (TESO), potency of vapor anesthetic (ExpISO; expired concentration of isoflurane), mean arterial pressure (MAP) and anesthetic exposure duration expressed by minutes (Tmin).
Statistical analyses
Total 97 data combinations in 30 patients were obtained. Measured Hb (Hb) was analyzed by independent variables such as rSO
2, PaCO
2, T
ESO, MAP, Tmin, sex, age and Exp
ISO. Sex data were also included as a dummy variable. Multilinear regression analysis was performed. Variables were selected by a stepwise method and final regression equation was expressed only with statistically significant variables. Standardized residuals (sR=predicted Hb-Hb) of final regression equation were also calculated. sR were compared with zero by one-sample t-test (z-test) then smoothed by locally weighted scatterplot smoothing (lowess) technique (
7). Linear regression analyses were performed between Hb and sR, and between smoothed Hb (sHb) and sR (ssR).
All statistical tests were performed using S-PLUS 8.0 for Windows (Insightful Corp, Seattle, WA, U.S.A.). The lowess parameter f was chosen to be 0.2 as a practical choice considering our sample size (
7). Statistical significance of all inferential statistics was judged when
p<0.05 and goodness-of-fit tests were considered to be passed when
p≥0.05.
RESULTS
Hb, MAP, T
ESO, rSO
2, Exp
ISO, PaCO
2, and estimated blood loss (EBL) were recorded (
Table 2). Hb was tightly regressed with three variables. Resultant regression equation was proved as follows (
p=0.000, r
2=0.809):
Hb=+8.580+0.238 · rSO2-0.338 · PaCO2-0.004 · Tmin (Eq. A)
Ignoring the minute contribution of Tmin (substituting Tmin with mean Tmin), equation A can be simplified as follows:
Hb=+8.332+0.238 · rSO
2-0.338 · PaCO
2 (Eq. B), (
Fig. 1)
Standardized residuals between Hb and predicted Hb were 0.086 ± 1.100 gm/dL (p=0.443) and were regressed by Hb as follows (p=0.000, r2=0.20):
sR=-2.7705+0.2492 Hb
However, goodness-of-fit test for above equation was failed (
p=0.0274). Lowess was performed (
Fig. 2). Regression equation of lowess'ed pairs of residuals (ssR) and Hb (sHb) was proved as follows (
p=0.000, r
2=0.14):
ssR=0.9730-0.1032 · sHb (Eq. C)
Test statistic for goodness-of-fit of equation C was 0.6877 (
Fig. 3).
DISCUSSION
In this study, we evaluated whether rSO
2 could predict the true or measured Hb levels using a prediction equation that was compared with clinically relevant levels of measured Hb. We successfully derived a mathematical equation that showed a correlation of Hb and rSO
2. Arterial carbon dioxide tension and anesthetic duration also affected the predicted Hb levels. Other potential variables that could affect the equation were excluded or included by stepwise selection. By the analysis of the residuals according to the measured Hb levels, the predicted Hb level by equation A had a tendency to underestimate the Hb level when the measured Hb levels were high, and to overestimate the Hb level when the hematocrit was low. Interestingly, our results are consistent with the classical concept of an inverse correlation between cerebral blood flow and hematocrit in animals (
8,
9) and humans (
10). For the level of measured Hb that appears to be cut-off point for overestimation was 9.4 gm/dL (0.9730/0.1032 from equation C). We predict that 1) low Hb below 9.4 gm/dL causes the cerebral vessels to dilate and raises the rSO
2, and 2) high Hb over 9.4 gm/dL may impede cerebral blood flow and lowers rSO
2 and thereby lowers the predicted Hb level.
Arterial carbon dioxide tension is another important variable that affects the result of our equation, and also a potential confounding factor, which made Dullenkopf et al. (
11) fail to prove the relationship of rSO
2 and Hb. We believe that an anesthesiologist can manage the arterial carbon dioxide tension within 5 mmHg, which affects Hb level ± 1.6 gm/dL (5 × 0.338 from equation A).
Anesthetic duration also affects the equation. Most vapor anesthetics increase cerebral blood flow (CBF) initially but decrease CBF to a steady state near pre-exposure levels in animals (
12). This finding was not evident in humans (
13). Our results show that prolonged exposure of isoflurane caused small increases of rSO
2. This finding is not consistent with previous reports (
12,
13). Possible explanation includes the inevitable failure of statistical independence of time-effect; the measured Hb decreases as a function of time in every patient. However, our result confined the time-effect within 0.004; this would suggest that the rSO
2 increased spontaneously up to +1% during 180 min of anesthesia despite a steady state of Hb; therefore, the time effect can be ignored in clinical decisions.
Our findings are compatible with the basic understanding on cerebral physiology and rheology. However, we do not suggest that our equation should be used to predict Hb levels for everyday anesthesia procedures; but rather provide additional information to better understand noninvasive prediction of Hb levels. Potential bias should be eliminated by further studies with a controlled study design and larger clinical database.
In conclusion, the value of near-infrared spectroscopy, rSO2 as an accurate, easy-to-read, noninvasive, real-time, and continuous predictor of Hb levels in clinical anesthesia has been demonstrated in this study. PaCO2 and anesthetic duration should also be considered as important factors for predicting Hb by rSO2. The Hb levels tend to be overestimated at lower Hb levels with the model presented here. Users of this model should keep in mind the assumptions of this design which includes a normal cerebral vasculature and blood pressure.







 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download