Abstract
A 17-yr-old young woman was referred to our hospital with a 2-yr history of claudication of the lower extremities and severe arterial hypertension. Physical examination revealed significantly different blood pressures between both arms (160/92 and 180/95 mmHg) and legs (92/61 and 82/57 mmHg). The hematological and biochemical values were within their normal ranges, except for the increased erythrocyte sedimentation rate (83 mm/hr) and C-reactive protein (6.19 mg/L). On 3-dimensional computed tomographic angiography, the ascending aorta, the aortic arch and its branches, and the thoracic and, descending aorta, but not the renal artery, were shown to be stenotic. The diagnosis of type IIb Takayasu's arteritis was made according to the new angiographic classification of Takayasu's arteritis, Takyasu conference 1994. Percutaneous transluminal angioplasty with stenting was performed on the thoracic and abdominal aorta. After the interventional procedures, the upper extremity blood pressure improved from 162/101 mmHg to 132/85 mmHg, respectively. She has been free of claudication and there have been no cardiac events during 2-yr of clinical follow-up.
Takayasu's arteritis is a well known, yet rare chronic inflammatory arteritis that affects the large vessels, predominantly the aorta and its main branches and the pulmonary arteries, and it leads to vessel wall thickening, fibrosis, stenosis, and thrombus formation. The symptoms of this disease reflect the patient's high blood pressure and end organ ischemia, such as coronary ischemia, cerebral ischemia, and extremity ischemia. The natural mortality rate of this disease is between 0 and 30% at five years, and the cause of death can be with congestive heart failure, myocardial infarction, cerebrovascular disease, and renal failure, which can be caused by ischemia based on stricture or closure (angiostenosis) of arteries (1). Therefore, aggressive medical and surgical treatment is required for patients suffering with major complications and a progressive disease course. The initial reports have revealed excellent results of percutaneous transluminal angioplasty (PTA) for treating patients with Takayasu's arteritis (2).
We report here on a case of type IIb Takayasu's arteritis, as determined by using the new angiographic classification of Takayasu's arteritis (3), in a 17-yr-old young woman. Her disease involved the ascending aorta, the aortic arch and its branches, and the thoracic and descending aorta, but not the renal artery.
A 17-yr-old young woman was referred to our hospital with a 2-yr history of claudication of the lower extremities and severe arterial hypertension. Physical examination revealed significantly different blood pressures between the both arms and legs: 160/92, 180/95, 82/57, and 92/61 mmHg in the right arm, left arm, right leg and left leg, respectively. The patient's body temperature was 36.8℃, the heart rate was 80 beats per min, and the respiratory rate was 20 per min. Levine grade III/IV bruits were audible over the left submandibular lesions. A grade 2/6 systolic murmur along the right sternal border and abdomen bruits were also detected. The pulses in the upper extremities were normal, however, the pulse in each of the lower extremity dorsalis arteries was absent. Ecchymosis was observed on the fundus of the eye and hypertensive retinopathy was not noted. The neurological examination was normal. The chest radiography showed mild cardiomegaly. The electrocardiography showed normal sinus rhythm. On admission, her hematological and biochemical values were within their normal ranges, except for the erythrocyte sedimentation rate (ESR) 83 mm/hr (normal, 0-9 mm/hr) and, C-reactive protein (CRP) 6.19 mg/L (normal, 0-0.36 mg/L). The urinalysis was normal. The 2-D transthoracic echocardiograpy showed trivial aortic regurgitation, mild left ventricular hypertrophy and a left ventricle (LV) ejection fraction of 70%, according to the modified Simpson's method.
After admission to the hospital, it was observed on 24 hr-ambulatory blood pressure monitoring (24-hr ABPM) that there was more than a 30 mmHg average difference between the upper extremity blood pressure and lower extremity blood pressure, which were 162/101 mmHg and 132/85 mmHg, respectively. On 3D-computed tomographic (CT) angiography, the ascending aorta, aortic arch and its branches, and the thoracic and descending aorta, but not the renal artery, were stenotic. The diagnosis of type IIb Takayasu's arteritis was made according to the new angiographic classification of Takayasu's arteritis (3). Neck magnetic resonance (MR) angiography showed the cut-off and near total occlusion at the osteal lesions of the left common carotid artery (Fig. 1). The left common carotid artery showed marked wall thickening and luminal narrowing, with a pinpoint lumen being seen on carotid Doppler sonography (Fig. 2). PTA was performed in the thoracic and abdominal aorta with using a 4.0/12 mm balloon catheter. Stenting with a 4.0/14 mm Niti-S stent in the aorta was then performed (Fig. 3).
The patient was discharged from the hospital on the 12th post-procedure day, with oral antiplatelet (plavix® 75 mg/day) therapy, steroid (40 mg/day) and immunosuppressive therapy (cyclophosphamide 100 mg/day, methotrexate 10 mg/mmHg and 130/78 mmHg, respectively (Fig. 4). On 3D-CT scanned after 2nd months of the procedures, the lower thoracic and abdominal aorta showed an intact lumen and good stent alignment (Fig. 5). The bruit from the abdomen disappeared and the pulse in each lower dorsalis artery was also monitored. Just prior to discharge, the laboratory findings were within normal levels for the ESR (2 mm/hr) and the CRP (0.32 mg/L) (Fig. 6).
The patient has been free of symptoms and there have been no cardiac events with ESR at 0.5 mm/hr and CRP at 0.1 mg/L during the 2-yr of clinical follow-up.
Takayasu's arteritis can be defined as chronic inflammatory arteritis that attacks the aorta, the coronary artery that originates from the aortic bifurcation, the pulmonary artery, and so on. In terms of the gold standard for diagnosis, according to the American college of Rheumatology 1990 criteria for the classification of Takayasu arteritis (4). If these criteria are satisfied, then there is 90.5% sensitivity and 97.8% specificity. According to the new angiographic classification of Takayasu's arteritis that depends on the angiographic finding and vessel involvement, the disease is divided into Type I, the branches from the aortic arch; Type IIa, the ascending aorta, aortic arch, and its branches; Type IIb, the ascending aorta, aortic arch, and its branches and, the thoracic descending aorta; Type III, the thoracic descending aorta, abdominal aorta; and/or renal arteries; Type IV, abdominal aorta and/or renal arteries; and Type V, combined features of types IIb and IV (3). These systems are useful in that they allow comparison of patients' characteristics according to the involved vessels and they are helpful in planning surgery, but they offer little information on the prognosis. Ishikawa defined clinical groups based on the natural history and complications of the disease. This case was type IIb Takayasu's arteritis. However, this classification, based on angiographic finding, may offer less information than Ishikawa clinical classification, based on the natural history and complication in prognosis.
The activity of Takayasu's arteritis can be measured by the ingravescence of the symptoms, an angiogram, and an increase in the ESR, CRP, interleukin-6, regulated on activation, normal T cell expressed and secreted (RANTES), etc (5, 6). Recently, the disease activity can also be measured by CT, MR, and [18F] fluorodeoxyglucose positron emission ([18F] FDG-PET) imaging in a non-invasive manner. The intensity of MR enhancement of the arterial wall and [18F] FDG-PET show a positive correlation with both the ESR and CRP levels, therefore, they may be correlated with the disease activity and so represent useful diagnostic indicators (7-9).
The standard medical treatment for Takayasu's arteritis include steroid treatment with methotrexate, azathioprin, cycloposphamide, and so on (10, 11). Recent reports have indicated that infliximab treatment can be applied when the patients experiences a relapse of the disease in spite of steroid treatment (12).
In the case of Takayasu's arteritis with vascular stenosis, it can be positively treated by internal treatment and operational treatments such as angioplasty. Although the diseases that are susceptible to operational treatments are not well established, they usually include renal arterial stenosis, ischemia that hinders daily life, cardiac ischemia caused by coronary arterial stenosis, ischemia caused by cerebrovascular stenosis, and aortic regurgitation (13-15). PTA has recently been being used for treatment along with invasive surgical operations (16). Surgical bypass of the stenosed segment is often complicated by graft reocclusion, anastomotic site aneurysm, and morbidity (17). Angioplasty offers a less invasive, cost-effective, and safe method for relief of stenotic lesions in patients with Takayasu's arteritis (18). Stent placement has been reported for the treatment of stenosis of the abdominal aorta and small arteries such as the carotid, mesenteric, or renal arteries in Takayasu's arteritis (19).
In summary, our patient was treated with PTA after treatment with steroid and methotrexate cycloposphamide, and her blood pressure became under control. Continuous follow-up is needed to assess the effect of steroid reduction on the disease activity.
Figures and Tables
Fig. 1
Neck MR angiography demonstrates the cut-off, filling and near total occlusions (arrow) at the osteal lesions of the left common carotid artery on the posterior-anterior view.
Fig. 2
The neck carotid Doppler sonogram. (A) Right common carotid artery shows normal luminal diameter without abnormalities. (B) and (C) Color flow doppler ultrasound scan (B) and spectral analysis (C) show a normal arterial flow in the right common carotid artery. (D) Left common carotid artery shows marked wall thickening and luminal narrowing. (E) and (F) Decreased blood flow on Color flow Doppler ultrasound scan (E) and decreased peak systolic pressure on spectral analysis (F) are noted in the left common carotid artery.

Fig. 3
(A) 3D-CT angiography shows focal stenosis in the descending aorta, but not the renal artery. (B) Percutaneous transluminal angioplasty was performed in the descending aorta using a 4.0/12 mm balloon catheter. (C) A 4.0/14 mm Niti-S stent in the aorta was inserted after ballooning.

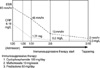
Fig. 4
24-hr ABPM shows more than a 30 mmHg mean difference between the upper extremity blood pressure and the lower extremity blood pressure. (A) 24-hr ABPM of an arm before and after PTA (B) 24-hr ABPM of a leg before and after PTA. 24-hr ABPM, 24 hr-ambulatory blood pressure monitoring; PTA, percutaneous angioplasty.

Fig. 5
(A) CT angiography shows the focal stenosis in the descending aorta beyond both renal arteries. (B) 3D reconstruction of CT angiography shows severe stenosis of the abdominal aorta, beyond both renal arteries. (C) After the insertion of a stent-graft, CT angiography shows the dilation of stenotic segments in the descending aorta. (D) 3D reconstruction of CT angiography after the insertion of a stent-graft.
References
1. Ishikawa K, Maetani S. Long-term outcome for 120 Japanese patients with Takayasu\'s disease Clinical and statistical analysis of related prognostic factors. Circulation. 1994. 90:1855–1860.
2. Sawada S, Tanigawa N, Kobayashi M, Morioka N, Kotani K, Senda T, Okuda Y, Ohta Y. Treatment of Takayasu's arteritis with self-expanding metallic stent (Giant-urco stent) in two patients. Cardiovasc Intervent Radiol. 1994. 17:102–105.

3. Moriwaki R, Noda M, Yajima M, Sharma BK, Numano F. Clinical manifestations of Takayasu arteritis in India and Japan--new classification of angiographic findings. Angiology. 1997. 48:369–379.
4. Arend WP, Michel BA, Bloch DA, Hunder GG, Calabrese LH, Edworthy SM, Fauci AS, Leavitt RY, Lie JT, Rightfoot RW Jr, Masi AT, Mcshane DJ, Mills JA, Stevens MB, Wallace SL, Zvaifler NJ. The American College of Rheumatology 1990 criteria for the classification of Takayasu arteritis. Arthritis Rheum. 1990. 33:1129–1134.

5. Hoffman GS, Ahmed AE. Surrogate markers of disease activity in patients with Takayasu arteritis. A preliminary report from The International Network for the Study of the Systemic Vasculitides (INSSYS). Int J Cardiol. 1998. 66:Suppl 1. S191–S194.
6. Andrew J, Al-Nahhas A, Pennell DJ, Hossain MS, Davies KA, Haskard DO, Mason JC. Non-invasive imaging in the diagnosis and management of Takayasu's arteritis. Ann Rheum Dis. 2004. 63:995–1000.
7. Noris M, Daina E, Gamba S, Bonazzola S, Remuzzi G. Interleukin-6 and RANTES in Takayasu arteritis a guide for therapeutic decisions? Circulation. 1999. 100:55–60.
8. Choe YH, Han BK, Koh EM, Kim DK, Do YS, Lee WR. Takayasu's arteritis: assessment of disease activity with contrastenhanced MR imaging. Am J Roentgenol. 2000. 175:505–511.
10. Shelhamer JH, Volkman DJ, Parrillo JE, Lawley TJ, Johnston MR, Fauci AS. Takayasu's arteritis and its therapy. Ann Intern Med. 1985. 103:121–126.

11. Hoffmann GS, Leavitt RY, Kerr GS, Rottem M, Sneller MC, Fauci AS. Treatment of glucocorticoid-resistant or relapsing Takayasu arteritis with methotrexate. Arthritis Rheum. 1994. 37:578–582.
12. Della Rossa A, Tavoni A, Merlini G, Baldini C, Sebastiani M, Lombardi M, Neglia D, Bombardieri S. Two Takayasu arteritis patients successfully treated with infliximab: a potential disease-modifying agent? Rheumatology. 2005. 44:1074–1075.

13. Koh KK, Hwang HK, Kim PG, Lee SH, Cho SK, Kim SS, Han JJ, Lee YT, Park PW, Yoon DH. Isolated left main coronary ostial stenosis in Oriental people: operative, histopathologic and clinical findings in six patients. J Am Coll Cardiol. 1993. 21:369–373.

14. Pyun WB, Yoon YS, Park KJ, Kim SY, Shim WH. Carotid artery stenting in patients Takayasu's arteritis: early and long-term follow-up results. Korean Circ J. 2000. 30:592–598.
15. Kerr GS, Hallahan CW, Giordano J, Leavitt RY, Fauci AS, Rottem M, Hoffman GS. Takayasu arteritis. Ann Intern Med. 1994. 120:919–929.

16. Tyagi S, Kaul UA, Nair M, Sethi KK, Arora R, Khalilullah M. Balloon angioplasty of the aorta in Takayasu's arteritis: initial and long-term results. Am Heart J. 1992. 124:876–882.

17. Giordano JM. Surgical treatment of Takayasu's arteritis. Int J Cardiol. 2000. 75:Suppl 1. S123–S128.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download