Abstract
The purpose of this study was to compare the effects on astigmatism after penetrating keratoplasty with three different suture techniques. In this prospective study, 38 eyes of 38 patients underwent penetrating keratoplasty with three suturing techniques: interrupted, single running, and double running. Topographic astigmatism was measured at 2, 6, 12, and 18 months after keratoplasty. During 18 months after surgery, the interrupted suture group had higher astigmatism than the double running suture group. There was no significant difference in the amounts of astigmatism during the first year after keratoplasty between the single running and the double running suture group. However, at 18 months after surgery, when all sutures were out, the double running suture group (3.60±1.58 diopters) showed significantly less astigmatism than the single running group (5.65±1.61 diopters). In conclusion, post-keratoplasty astigmatism was the least in the double running suture group of the three suturing techniques at 18 months after penetrating keratoplasty.
Visual acuity after successful penetrating keratoplasty depends mainly on the clarity of the graft and the refractive error, particularly the astigmatic component. Severe irregular astigmatism is often seen after keratoplasty and can delay visual rehabilitation, even with a clear graft. A variety of factors affect postoperative astigmatism, including disparity between donor button and recipient bed, graft diameter, malposition of donor and recipient corneas, underlying diagnosis of the recipient, wound configuration abnormality, and the suture technique employed (1-5).
There are three commonly used major suture techniques such as interrupted, single running, and double running. Many studies have shown that the interrupted suture technique results in higher astigmatism than the single or double running suture techniques (6-9). However, the difference in the results between the single running and double running sutures remains largely controversial. Indeed, various results have been obtained depending on study duration and time of suture removal: less astigmatism have been found with single running sutures while the sutures are still in place (10), whereas no differences (11) or less astigmatism in early period with double running sutures (12). Herein, we prospectively studied the cases with penetrating keratoplasty, to compare the amount of astigmatism after the operation with three different suture techniques: interrupted, single running, and double running. In addition, we investigated the final astigmatic outcome after suture removal.
This prospective study was performed on patients who underwent penetrating keratoplasty between January 2003 and June 2005 by one surgeon. All the protocols of our current study were concordant with the tenets of the Declaration of Helsinki and informed consent was obtained from the included subjects. In cases of vascularized cornea, interrupted sutures were done. Otherwise, patients were randomly assigned to two suturing techniques; single running and double running. Patients with combined cataract or glaucoma surgery, corneal scarring including peripheral cornea, and the subject who underwent therapeutic keratoplasty for infectious keratitis were excluded at the beginning of study. During investigation, the subjects who showed delayed wound healing more than 3 weeks, graft rejection, newly developed intractable glaucoma, or with wound problems such as dehiscence were excluded. The patients were followed up for at least 18 months. Finally, 38 eyes of 38 patients were included.
There were 16 eyes with the interrupted suture technique, 12 eyes with the double running suture technique, and 10 eyes with the single running sutures (Fig. 1). Diagnosis, age, and gender of patients included are listed in Table 1. There was no significant difference in diagnosis among the three groups (p=0.859, χ2 test).
The mean donor age was 45.5±12.9 yr (22-74), average postmortem time was 4.8±1.9 hr (1-9), and the mean preservation time was 124.8±29.4 hr (72-144). All donor corneas were stored in Optisol (Chiron Ophthalmics, Irvine, CA, U.S.A.). The mean trephine size of the recipient was 7.34±0.35, 7.10±0.21, and 7.21±0.21 mm for the interrupted, single running, and double running sutured eyes, respectively, and these differences were not significant. The mean trephine size of the donor was 7.73±0.32, 7.60±0.21, and 7.65±0.20 mm for the interrupted, single running, and double running, respectively, and these differences were not significant. The mean donor-recipeint disparity was 0.39±0.13, 0.50±0.0, and 0.44±0.11 mm (oversized) for the interrupted, single running, and double running, respectively, and these were not significantly different (p>0.05, Mann-Whitney U test between each of two groups).
Penetrating keratoplasty was performed by a standard technique using a Hessburg-Barron trephine (JedMed Instrument Co., St. Louis, MO, U.S.A.). For the interrupted suture group, 16 bites were placed with 10-0 nylon. Selective removal of interrupted nylon sutures along the steepest meridian was performed, if associated with greater than 3 diopters of astigmatism in that meridian, starting two months after surgery, until the resultant astigmatism reached 3.0 diopters or less. For the double running suture group, two running sutures of 12 bites each were placed with 10-0 nylon by the anti-torque mode, and one 10-0 nylon suture was removed 6 to 10 months after keratoplasty and the other 12 to 16 months after surgery. For the single running suture group, a 10-0 nylon running suture with 16 to 24 bites was used with the torque mode, and the sutures were removed 10 to 18 months after surgery. At the end of surgery, the suture was adjusted to make the hand-held keratometer ring mires round.
Sim K's astigmatism was measured with the Orbscan (Orbtek Inc. Salt Lake City, UT, U.S.A.) at 2, 6, 12, and 18 months after surgery (Fig. 2). Sim K's astigmatism was also measured before and three months after each suture removal. Final astigmatism at 18 months after surgery was obtained at least one month after complete suture removal. The Mann-Whitney U test was used to compare the astigmatism between two groups and Wilcoxon matched pairs signed ranks test was done to analyze changes in astigmatism after suture removal. A value of p<0.05 was considered statistically significant.
The final astigmatism values at 18 months after surgery following removal of all sutures were: 6.16±2.32 diopters in the interrupted suture group (n=16), 5.65±1.61 diopters in the single running (n=10), and 3.60±1.58 diopters in the double running suture group (n=12) (Table 2). There was no significant difference in the amounts of astigmatism between the double and single running suture groups at 2, 6, and 12 months after surgery (Table 2). However, at 18 months, the double running suture group showed significantly less astigmatism than the single running group (p=0.014, Mann-Whitney U test, Table 2). The single running suture group showed less astigmatism than the interrupted group with borderline significance at 6 months (p=0.060, Mann-Whitney U test) after surgery; however, at 18 months, there was no difference in the amounts between these two groups (Table 2, Fig. 3). The double running suture group showed significantly less astigmatism throughout the study period than the interrupted suture group (p<0.05, Mann-Whitney U test, Fig. 3). During the study period, astigmatism in all three suture groups tended to decrease gradually; however, astigmatism in the single running suture group increased at 18 months compared to 12 months after surgery (Fig. 3). The interrupted suture group showed significantly less astigmatism after selective suture removal (Table 3, Fig. 4). However, the single running suture group showed increased astigmatism at three months after surgery with borderline significance (Table 3, Fig. 4).
This prospective study was undertaken to investigate the difference in astigmatism among patients who underwent penetrating keratoplasty by three different suturing techniques: interrupted, single running, and double running sutures. During 18 months after surgery, the interrupted suture group showed significantly higher astigmatism than the double running suture group. During 6 months after surgery, the interrupted suture group showed significantly higher astigmatism than the single running suture group. However, when the sutures were out, the interrupted sutures no longer showed significantly higher astigmatism than the single running group. There was no significant difference in the amounts of astigmatism between the single running and double running suture groups during the first year after keratoplasty. However, at 18 months after surgery, when all sutures were out, the double running suture group showed less astigmatism than the single running group.
In this study, astigmatism in the single running group was found to increase at 18 months than 12 months after surgery when the suture was out. For the single running suture technique, there are some contradictory reports on changes of astigmatism after suture removal: Solano et al. (11) reported that, in a single running suture group, astigmatism increased to as high as 1.7 diopters one month after suture removal. On the other hand, Spadea et al. (12) reported no significant change of astigmatism after suture removal. Moreover, Mader et al. (13) reported an average decrease of 0.52 diopters in astigmatism, however, the astigmatism in 62% of eyes changed two or more diopters after suture removal, therefore, they concluded that corneal astigmatism may change unpredictably and, by large amounts, when all remaining sutures are removed. These findings suggest that direct suture tension may play an important role in maintaining corneal configuration in single running suture technique.
For the double running suture, a double radial suture was placed with a diagonal pattern in which the second suture ran in the opposite direction of the first one. Hoffmann (14) described that the double running suture with a diagonal pattern overcomes vertical factors with regard to radial and diagonal continuous sutures, which by necessity leads to gaping of the inner and outer wound fissure. The double continuous diagonal suture (cross-stitch suture) can neutralize the forces in the direction toward the surface and the deep stroma, thus providing a uniform seal for the wound fissure. On the other hand, however, the single running suture does not have such an effect, and this might be responsible for increasing astigmatism after suture removal in the single running suture group. Conversely, the fact that no significant changes were observed after suture removal in the double running group might imply that this neutralizing effect helps to stabilize the graft configuration.
In all three groups, there was a decreasing tendency of astigmatism during the first postoperative year. For the interrupted suture group, this may be partially due to a selective suture removal along the steepest meridian, because this suture removal method has been known to significantly reduce astigmatism (15). In the single running suture group, postoperative suture adjustment was not done because of safety reason, even though postoperative suture adjustment has been reported to reduce the corneal astigmatism (16). In contrast to the interrupted or double running suture, rupture or loosening of suture, which can be induced by suture manipulation, is a much more serious problem requiring additional bites in the single running suture, because no other suture material supports the tightness of the button.
There are some limitations in this study. Interrupted suturing technique was not randomly assigned, although other two techniques were randomly assigned. Therefore, diagnoses of interrupted suture group were different compared to other groups. Contrary to the fact that preoperative diagnoses are relatively evenly distributed in single and double running groups, the number of keratoconus cases was relatively lower in interrupted suture group than the numbers in other suturing technique groups (Table 1). This uneven distribution of preoperative diseases might probably affect the results. To minimize the effect on peripheral wound healing, we excluded patients with corneal scarring including the peripheral cornea. Moreover, peripheral vascularization in the interrupted suture group might affect the astigmatism value. However, we excluded patients with an wound problem during the follow-up period that can be potentially related to changes in configuration. Thus, the presence of peripheral vascularization may not affect astigmatism significantly. Although some limitations mentioned above, we strongly believe that our study still provides informative data for understanding the effect of suture on astigmatism.
In summary, at 18 months after penetrating keratoplasty following removal of all sutures, the double running suture technique showed less astigmatism than the single running and interrupted suture techniques. The single running suture group showed increased astigmatism at 18 months that may be related to suture removal, even though it showed small astigmatism similar to double running suture group during 12 months after surgery.
Figures and Tables
Fig. 1
Three suturing techniques in penetrating keratoplasty; interrupted (A), double running (B), and single running (C).

Fig. 2
Topographic astigmatism of representative cases with three different suture techniques by the Orbscan topographic system (A: interrupted suture, B: double running suture, C: single running suture). All three were done 12 to 18 months after surgery, when all the sutures were removed.

Fig. 3
The changes in astigmatism measured with the Orbscan (Orbtek Inc. Salt Lake City, UT, U.S.A.) at 2, 6, 12, and 18 months after penetrating keratoplasty in three groups. INT, DRS, and SRS represent interrupted suture, double running, and single running suture, respectively. Horizontal bars represent two standard errors of mean (SEM).
*, Significantly different (p<0.05, Mann-Whitney U test) compared to other two groups, respectively; †, significantly different (p<0.05, Mann-Whitney U test) between INT and DRS groups.
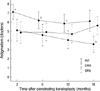
Fig. 4
Topographic astigmatism (Diopters, mean±SD) before initial suture removal and three months after suture removal in each suturing technique groups. INT, DRS, and SRS represent interrupted suture, double running, and single running suture, respectively. Horizontal bars represent two standard errors of mean (SEM).
*, Significantly different astigmatism between before initial suture removal and three months after suture removal (p<0.05, Wilcoxon matched pairs signed ranks test).
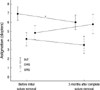
Table 1
Preoperative diagnosis of recipients and demographic variables in each suture technique group

Table 2
Topographic astigmatism (diopters, mean±standard deviation) over time in each suturing technique groups

References
2. Serdarevic ON, Renard GJ, Pouliquen Y. Randomized clinical trial comparing astigmatism and visual rehabilitation after penetrating keratoplasty with and without intraoperative suture adjustment. Ophthalmology. 1994. 101:990–999.

3. Hoppenreijs VP, Van Rij G, Beekhuis WH, Rijneveld WJ, Rinkelvan Driel E. Causes of high astigmatism after penetrating keratoplasty. Doc Ophthalmol. 1993. 85:21–34.

4. Murta JN, Amaro L, Tavares C, Mira JB. Astigmatism after penetrating keratoplasty. Role of the suture technique. Doc Ophthalmol. 1994. 87:331–336.
5. Seitz B, Langenbucher A, Kuchle M, Naumann GO. Impact of graft diameter on corneal power and the regularity of postkeratoplasty astigmatism before and after suture removal. Ophthalmology. 2003. 110:2162–2167.

6. Filatov V, Steinert RF, Talamo JH. Postkeratoplasty astigmatism with single running suture or interrupted sutures. Am J Ophthalmol. 1993. 115:715–721.

7. Boruchoff SA, Jensen AD, Dohlman CH. Comparison of suturing techniques in keratoplasty for keratoconus. Ann Ophthalmol. 1975. 7:433–436.
8. Van Meter WS, Gussler JR, Soloman KD, Wood TO. Postkeratoplasty astigmatism control. Single continuous suture adjustment versus selective interrupted suture removal. Ophthalmology. 1991. 98:177–183.
9. Frost NA, Wu J, Lai TF, Coster DJ. A review of randomized controlled trials of penetrating keratoplasty techniques. Ophthalmology. 2006. 113:942–949.

10. Ramirez M, Hodge DO, Bourne WM. Keratometric results during the first year after keratoplasty: adjustable single running suture technique versus double running suture technique. Ophthalmic Surg Lasers. 2001. 32:370–374.

11. Solano JM, Hodge DO, Bourne WM. Keratometric astigmatism after suture removal in penetrating keratoplasty: double running versus single running suture techniques. Cornea. 2003. 22:716–720.
12. Spadea L, Cifariello F, Bianco G, Balestrazzi E. Long-term results of penetrating keratoplasty using a single or double running suture technique. Graefes Arch Clin Exp Ophthalmol. 2002. 240:415–419.

13. Mader TH, Yuan R, Lynn MJ, Stulting RD, Wilson LA, Waring GO 3rd. Changes in keratometric astigmatism after suture removal more than one year after penetrating keratoplasty. Ophthalmology. 1993. 100:119–126.

14. Hoffmann F. Suture technique for perforating keratoplasty. Klin Monatsbl Augenheilkd. 1976. 169:584–590.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download