Abstract
The increasing prevalence of methicillin-resistant Staphylococcus aureus (MRSA) has become of great concern in both hospital and community settings. To evaluate the prevalence and risk factors for methicillin resistance among Staphylococcus aureus, blood isolates in our Emergency Department (ED) were collected. All patients with S. aureus bacteremia (SAB) who presented to the ED from January 2000 to August 2005 were included, and a retrospective study was performed. A total of 231 patients with SAB were enrolled (median age, 59 yr; M:F, 125:106). Among these patients, methicillin-resistant strains accounted for 27.3% (63 patients). Catheter-related infection was the most frequent primary site of SAB (39.0%), followed by skin and soft tissue infection (16.5%). In multivariate analysis, recent surgery (OR, 3.41; 95% CI, 1.48-7.85), recent hospitalization (2.17; 1.06-4.62), and older age (≥61 yr) (2.39; 1.25-4.57) were independently associated with the acquisition of methicillin-resistant strains. When antimicrobial therapy is considered for the treatment of a patient with suspected SAB, clinicians should consider obtaining cultures and modifying empirical therapy to provide MRSA coverage for patients with risk factors: older age, recent hospitalization, and recent surgery.
Staphylococcus aureus is one of the most common causes of nosocomial infection and community-acquired infection. Antimicrobial resistance has been a problem primarily in the healthcare setting. In recent years, however, community-acquired S. aureus infection has been a problem due to the rapidly increasing emergence and spread of antimicrobial resistance (1-4). In the United States, S. aureus infections associated with skin and soft tissue infection (SSTI) in the community-acquired settings showed a methicillin resistance rate higer than 50%, and the initial treatment with glycopeptide for severe SSTI was recommended (3, 5). A few groups have investigated the proportion of clinical isolates of S. aureus that are of methicillin-resistant Staphylococcus aureus (MRSA) among non-hospitalized or hospitalized patients in Korea (6-10). In the United States, a an article was recently reported about MRSA infections among patients in the Emergency Department (ED) (11). However, there have been no data published about the prevalence of MRSA bacteremia in the ED.
In ED settings, where the initial triage of patients occurs, the diagnosis of bacteremia is presumptive, and antimicrobial agents are often prescribed empirically. It is important to select appropriate antibiotics for patients admitted to the ED. Several studies have demonstrated that appropriate empirical antibiotic treatment had a favorable effect on the outcome in patients with S. aureus bacteremia (SAB) (12, 13). Many physicians have difficulties in deciding whether vancomycin or other glycopeptides should be included in the empirical antibiotic regimen until preliminary microbiology reports become available (1, 2). Identification of risk factors that are associated with the presence of methicillin resistance in S. aureus isolates recovered from patients with bacteremia could help infection control efforts and in choosing empirical therapeutic agents with pending culture and susceptibility results.
We performed this study to reveal the prevalence and characteristics of MRSA isolates, and the risk factors that are associated with methicillin resistance among SAB patients in the ED to give better information about the choice of empirical therapeutic agents for suspicious SAB patients.
Our study was based on all adults who had visited the ED at the Samsung Medical Center (SMC) in Korea. The SMC is a tertiary-care teaching hospital with 1,350 hospital beds. The hospital provides specialized medical and surgical care, including bone marrow and solid organ transplantation, for children and adult patients. The annual ED census is approximately 55,000 visits.
All patients admitted through the ED who had S. aureus recovered from blood cultures (1 or more sets) within the first 72 hr of their hospital stay were included by means of a retrospective review of medical records and of the electronic records of the Clinical Microbiology Laboratory between 1 January 2000 and 31 August 2005. A retrospective case-control analysis was made on all patients. Those patients with SAB as part of polymicrobial bloodstream infection (BSI) were excluded.
The recovery of S. aureus isolates from blood was accomplished by the processing of blood cultures in the BACTEC Model 9240 (BD Diagnostic Instrument Systems, 7 Loveton Circle, Sparks, MD, U.S.A.) or BacT/ALERT 3D (Bio-Merieux Inc., Hazelwood, MO, U.S.A.). Identification of S. aureus was carried out using standard methods (coagulase test and latex kit test). Antibiotic susceptibility test of S. aureus isolates was performed on the VITEK II automated system with GPI Cards (BioMerieux) using the modified broth microdilutional method. Minimum inhibitory concentration breakpoints and quality-control protocols were used according to standards established by the Clinical and Laboratory Standards Institute (14).
Patients were considered to have staphylococcal BSI when one or more blood cultures were positive for S. aureus and when the clinical course was consistent with staphylococcal infection (that is, the clinicians or the infectious disease consultant judged the organism to be a pathogen), and when the antibiotic therapy directed against the organism was administered.
Among the primary foci of infection, catheter-related infection was defined according to the IDSA guidelines (15); infective endocarditis was defined according to the modified Duke criteria (16); skin and soft tissue infection, bone and joint, lung, gastrointestinal or genitourinary lesion were defined when such sites were found with clinical findings or imaging abnormalities and S. aureus strains were isolated from blood and/or those sterile specimens (17).
The status of the following parameters was determined based on medical records and the electronic records of the Clinical Microbiology Laboratory: age, sex, underlying illness, history of hospitalization, operation and mechanical ventilation care within previous 1 yr, existence of implanted catheter, patient outcomes including mortality, and antimicrobial susceptibilities of the microorganisms.
In order to identify the risk factors associated with methicillin resistance in SAB, data were compared between two groups, patients with MRSA and those with MSSA. The results were analyzed using the SPSS 11.0 for Windows software package (SPSS Inc, Chicago, IL, U.S.A.). The categorical variables were compared using a Pearson χ2-test or Fisher's exact test, as appropriate, and the continuous variables were analyzed with Student's t-test or the Mann-Whitney U-test. Predictor variables associated with MRSA infection were initially assessed by univariate analysis. Factors found to be associated with MRSA bacteremia by univariate analysis were then analyzed by multivariate analysis to identify any significant independent associations. A two-tailed p value of less than 0.05 was considered to be statistically significant.
This study was approved by the Institutional Review Board at Samsung Medical Center (# 2006-04-025). Informed consent form from patients was waived because no direct patient contact was anticipated and no follow-up interviews were conducted. All data collected for the purpose of this study were kept confidential.
During this study period, 630 cases of SAB were identified in the ED. A total of 399 episodes of SAB were excluded because they represented recurrent SAB in the same patient, or demonstrated a single culture without significant signs of infection, or the strain was identified after 72 hr. Thus, a total of 231 patients with SAB were analyzed.
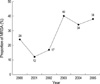
Of the 231 patients, 168 (72.7%) isolates were MSSA. MRSA accounted for 27.3% (63 patients) of SAB. Fig. 1 shows the proportion of MRSA isolates among SAB per study year. The proportion of MRSA isolates recovered from the blood within 72 hr of the ED visit increased significantly over the study period; from 12-24% during 2000-2001 to 34-38% during 2004-2005 (p=0.019).
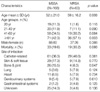
The incidence of MRSA was significantly higher among older (especially ≥61 yr) patients (p=0.003). Catheter-related BSIs were the most frequent known underlying sources of SAB (39.0%), followed by SSTI (16.5%) and bone and joint infections (13.0%). There was no significant difference between the two groups in primary foci of SAB, even though the frequency of MRSA tended to be higher among catheter-related BSI (Table 1).
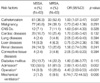
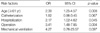
Factors associated with an increased risk for recovery of MRSA strains by univariate analysis were: age over 61 yr, the presence of any type of catheter (central venous catheter, urinary catheter etc.) at the time of ED visit, previous hospitalization or a history of surgical procedure, or use of mechanical ventilation within the past 1 yr (Table 2). Using multivariate analysis, a history of recent surgery (OR, 3.41; 95% CI, 1.47-7.85), recent hospitalization (2.17; 1.06-4.62), and older age (2.39; 1.25-4.57) were each independently associated with MRSA bacteremia (Table 3). Fifty nine (93.7%) of 63 patients with MRSA bacteremia had at least one of the independent risk factors described above. Ten (83.3%) of 12 patients who had all three risk factors were found to have MRSA bacteremia.
While MSSA strains remained susceptible to various antimicrobial agents, MRSA strains were resistant to many antimicrobials. Among MRSA isolates, there were 51 (81.0%) that were multidrug resistant (resistance to three or more antimicrobials). All 63 MRSA isolates were susceptible to vancomycin. In contrast to the high resistance rates to other antimicrobials, 90.6% and 84.1% of MRSA isolates were susceptible to rifampin and trimethoprim/sulfamethoxazole (TMP/SMX), respectively.
The crude mortality rate of patients who had S. aureus isolated from blood cultures within 72 hr of arrival in the ED was 22.5%. The crude mortality rate did not differ significantly between patients with MRSA and MSSA bacteremia, although it tended to be higher in MRSA patients (Table 1). Patients with indwelling catheterization (OR, 0.31; CI, 0.14-0.66) showed a low mortality rate associated with this disease; this could be attributable to early removal of the primary infection site.
The epidemiology of MRSA infection is changing. Strains of MRSA, which previously have been largely confined to hospitals and long-term care facilities, are emerging in the community (4, 18).
This study characterizes the epidemiology of MRSA bacteremia from the community, defined as recovery of MRSA from blood cultures within the first 72 hr of an ED visit. Previous reports in Korea found MRSA infection among patients with community-acquired SAB to be less than 20% (8, 19). Our data show a proportion of MRSA among patients with SAB within the first 72 hr of ED visit to be 27.3%.
So far, different patient populations have been the focus in several studies. In those studies, they have discussed potential risk factors of MRSA infections at the time of admission (20-22). These data indicated several predictor variables that were independently associated with MRSA bacteremia. MRSA bacteremia at the time of the ED visit was independently associated with older age, a history of admission to a hospital, and a history of surgery in the previous year. In our study population, the most frequent underlying source for MRSA bacteremia was infection from any type of catheter. Perhaps this result can be attributed to the fact that our hospital is a tertiary hospital with large numbers of patients with malignancy, chronic renal failure, and old age (prone to cerebrovascular accident or dementia).
Treatment of serious S. aureus infections can be challenging, and the associated mortality rate remains between 20 to 50 percent despite the availability of highly active antimicrobial agents (23, 24). In our study, the overall mortality of SAB seen in the ED was 22.5%.
The choice of agents is problematic since widespread use of glycopeptides in pending results from blood cultures is likely to raise the cost, spread of resistance, and affect the greater drug toxicity (25, 26). Of the 68 patients with MRSA bacteremia in this study, 30 (47.6%) were initially prescribed β-lactam drugs, to which the organism was resistant. Of the 168 patients with MSSA bacteremia, 53 (31.5%) were initially prescribed glycopeptide agents. This is similar to the results of other studies of SAB in which there were no differences in MSSA and MRSA mortality rates (13, 19, 27).
Effective antibiotic therapy and risk assessment may be needed, along with good infection control practices, to reduce the incidence of MRSA.
Several potential limitations should be considered when interpreting our results. Because this was a retrospective prevalence study, the temporal relationship between the acquisition of MRSA and exposure to medical attention was uncertain. Moreover, the prevalence of MRSA in the community at our ED may be substantially different from other Korean communities. The population at this hospital may be skewed because our hospital is a large, academic tertiary center. Nonetheless, this study is the first report concerning the prevalence, and risk factors of MRSA bacteremia ascertained through ED visits in Korea.
In summary, methicillin resistance was not uncommon in SAB among patients from our ED population. The proportion of MRSA among SAB seen at ED visit increased significantly over the study period. Risk factors for MRSA identified in this study were older age (over 61 yr), previous hospitalization, and a history of surgery. These factors can be helpful in the selection of empirical antimicrobial agents. A prospective study with a larger population is needed to overcome possible geographic variations in the epidemiology of MRSA colonization and/or infection in non-hospitalized or hospitalized populations.
Figures and Tables
Fig. 1
The proportion of MRSA among S. aureus isolates recovered from the blood within 72 hr of ED visit for the study years. The dashed line is a trend bar of proportions. MRSA, methicillin-resistant S. aureus.
References
1. Naimi TS, LeDell KH, Como-Sabetti K, Borchardt SM, Boxrud DJ, Etienne J, Johnson SK, Vandenesch F, Fridkin S, O'Boyle C, Danila RN, Lynfield R. Comparison of community- and health care-associated methicillin-resistant Staphylococcus aureus infection. JAMA. 2003. 290:2976–2984.
2. Sattler CA, Mason EO Jr, Kaplan SL. Prospective comparison of risk factors and demographic and clinical characteristics of community-acquired, methicillin-resistant versus methicillin-susceptible Staphylococcus aureus infection in children. Pediatr Infect Dis J. 2002. 21:910–917.

3. Fridkin SK, Hageman JC, Morrison M, Sanza LT, Como-Sabetti K, Jernigan JA, Harriman K, Harrison LH, Lynfield R, Farley MM. Methicillin-resistant Staphylococcus aureus disease in three communities. N Engl J Med. 2005. 352:1436–1444.
4. Salgado CD, Farr BM, Calfee DP. Community-acquired methicillin-resistant Staphylococcus aureus: a meta-analysis of prevalence and risk factors. Clin Infect Dis. 2003. 36:131–139.
5. Frazee BW, Lynn J, Charlebois ED, Lambert L, Lowery D, Perdreau-Remington F. High prevalence of methicillin-resistant Staphylococcus aureus in emergency department skin and soft tissue infections. Ann Emerg Med. 2005. 45:311–320.

6. Kim SH, Park WB, Lee KD, Kang CI, Choe YJ, Kim HB, Park SW, Kim US, Oh MD, Kim EC, Choe KW. The effects of initial empirical antibiotics regimens on the outcomes of Staphylococcus aureus bacteremia. Korean J Infect Dis. 2002. 34:293–304.
7. Kim HB, Kim T, Lee BB, Kim US, Park SW, Shin JW, Oh MD, Kim EC, Lee YS, Kim BS, Choe KW. Frequency of resistance to aminog lycoside antibiotics in staphy lococcus aureus isolated from tertiary hospitals. Korean J Infect Dis. 2002. 34:39–46.
8. Kim YJ. A study of prevalence and antibiotic susceptibilities of staphylococcus aureus in the bacterial skin infection of dermatology outpatients. Korean J Dermatol. 2001. 39:866–871.
9. Kim HB, Sa CM, Yoo J, Kim BS, Yun OJ, Yoon HR, Lee YS. Antibiotic resistance patterns of Staphylococcus aureus isolated from the patients admitted to non-tertiary hospitals. Korean J Infect Dis. 2000. 32:259–263.
10. Kim US, Bang JH, Kim HB, Park SW, Oh MD, Song YW, Kim CH, Kim EC, Choe KW. Epidemiology of and risk factors for methicillin resistance in community-acquired and nosocomial Staphylococcus aureus bacteremia. Korean J Infect Dis. 1999. 31:325–331.
11. Moran GJ, Krishnadasan A, Gorwitz RJ, Fosheim GE, McDougal LK, Carey RB, Talan DA. Methicillin-resistant S. aureus infections among patients in the emergency department. N Engl J Med. 2006. 355:666–674.
12. Lodise TP, McKinnon PS, Swiderski L, Rybak MJ. Outcomes analysis of delayed antibiotic treatment for hospital-acquired Staphylococcus aureus bacteremia. Clin Infect Dis. 2003. 36:1418–1423.

13. Rezende NA, Blumberg HM, Metzger BS, Larsen NM, Ray SM, McGowan JE Jr. Risk factors for methicillin-resistance among patients with Staphylococcus aureus bacteremia at the time of hospital admission. Am J Med Sci. 2002. 323:117–123.

14. Standards NCCLS. Performance Standards for Antimicrobial Disk Susceptibility Tests-Eight Deition: Approved Standard M100-S13 (M2). 2003. Wayne, PA, USA: NCCLS.
15. Mermel LA, Farr BM, Sherertz RJ, Raad II, O'Grady N, Harris JS, Craven DE. Guidelines for the management of intravascular catheter-related infections. Clin Infect Dis. 2001. 32:1249–1272.

16. Durack DT, Lukes AS, Bright DK. New criteria for diagnosis of infective endocarditis: utilization of specific echocardiographic findings. Duke Endocarditis Service. Am J Med. 1994. 96:200–209.
17. Garner JS, Jarvis WR, Emori TG, Horan TC, Hughes JM. CDC definitions for nosocomial infections. Am J Infect Control. 1988. 16:128–140.
18. Chambers HF. The changing epidemiology of Staphylococcus aureus? Emerg Infect Dis. 2001. 7:178–182.

19. Kim SH, Park WB, Lee KD, Kang CI, Bang JW, Kim HB, Kim EC, Oh MD, Choe KW. Outcome of inappropriate initial antimicrobial treatment in patients with methicillin-resistant Staphylococcus aureus bacteraemia. J Antimicrob Chemother. 2004. 54:489–497.

20. Jernigan JA, Pullen AL, Partin C, Jarvis WR. Prevalence of and risk factors for colonization with methicillin-resistant Staphylococcus aureus in an outpatient clinic population. Infect Control Hosp Epidemiol. 2003. 24:445–450.
21. Charlebois ED, Bangsberg DR, Moss NJ, Moore MR, Moss AR, Chambers HF, Perdreau-Remington F. Population-based community prevalence of methicillin-resistant Staphylococcus aureus in the urban poor of San Francisco. Clin Infect Dis. 2002. 34:425–433.

22. Goetz A, Posey K, Fleming J, Jacobs S, Boody L, Wagener MM, Muder RR. Methicillin-resistant Staphylococcus aureus in the community: a hospital-based study. Infect Control Hosp Epidemiol. 1999. 20:689–691.
23. Cosgrove SE, Sakoulas G, Perencevich EN, Schwaber MJ, Karchmer AW, Carmeli Y. Comparison of mortality associated with methicillin-resistant and methicillin-susceptible Staphylococcus aureus bacteremia: a meta-analysis. Clin Infect Dis. 2003. 36:53–59.
24. Blot SI, Vandewoude KH, Hoste EA, Colardyn FA. Outcome and attributable mortality in critically Ill patients with bacteremia involving methicillin-susceptible and methicillin-resistant Staphylococcus aureus. Arch Intern Med. 2002. 162:2229–2235.

25. Wyllie DH, Peto TE, Crook D. MRSA bacteraemia in patients on arrival in hospital: a cohort study in Oxfordshire 1997-2003. BMJ. 2005. 331:992.

26. Huang SS, Platt R. Risk of methicillin-resistant Staphylococcus aureus infection after previous infection or colonization. Clin Infect Dis. 2003. 36:281–285.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download