Abstract
This study was performed to evaluate the usefulness of carbohydrate-deficient transferrin (CDT) as a marker of heavy drinking in Korean males. The subjects (143 Korean males) were classified into 2 groups according to the amount of drinking, moderate drinkers (72 individuals) who drank 14 drinks or less per week and heavy drinkers (71 individuals) who drank more than 14 drinks per week. Using %CDT, gamma glutamyl transferase (GGT), aspartate aminotransferase (AST), and alanine aminotransferase (ALT) as clinical markers for heavy drinking, sensitivity, specificity, positive and negative predictive values were investigated. Sensitivities of %CDT, GGT, AST, and ALT were 83.1%, 67.6%, 52.1% and 46.5%, respectively. Specificities were 63.9%, 45.8%, 72.2%, and 54.2%, respectively. Positive predictive values were 69.4%, 55.2%, 64.9%, and 50.0% respectively. Negative predictive values were 79.3%, 58.9%, 60.5%, and 50.6% respectively. The areas under the receiver operating characteristic curve (95% confidence interval) for %CDT, GGT, AST, and ALT were 0.823 (0.755-0.891), 0.578 (0.484-0.673), 0.622 (0.528-0.717), and 0.516 (0.420-0.613), respectively. CDT is considered as the most reliable marker for detecting heavy drinking in Korean males.
Alcohol abuse is a very common problem in Korea. According to the data published by the Korean National Statistical Office (1) in January 2006, each of Korean adults aged over 19 drank around 25.6 L of soju (Korean type of beverage of hard liquor), 55.0 L of beer, and 68.5 L of other types of alcohol on average. The report (2) that the lifetime prevalence of alcohol use disorder was 21.98% means that at least 2 out of 10 adults experienced mental diseases caused by drinking.
Despite the clinical and social seriousness of the drinking problem, many cases of alcoholism are not diagnosed because of the low awareness of the seriousness not only among ordinary people but also among physicians (3). The clinical quantitative definition of heavy drinking is considered as more than two drinks per day for male adults and more than one drink for female adults (4). Twelve grams of alcohol is the drinking quantity equivalent to the clinical definition of a standard drink, which is contained in each of 1.5 ounce of 80 proof whiskey, 12 ounce of beer, and 5 ounce of wine, because the specific gravity of alcohol is 0.7893 (4).
Chronic heavy drinking increases biological indicators such as aspartate aminotransferase (AST), alanine aminotransferase (ALT), gamma glutamyl transferase (GGT), mean corpuscular volume (MCV), carbohydrate-deficient transferrin (CDT), high-density lipoprotein cholesterol, uric acid, etc. These biological indicators can be useful information not only for diagnosing alcohol abuse but also for providing visible feedback to reduce drinking in clinical counseling over heavy drinking (5). However, the level of liver enzymes shows relatively low specificity, MCV has a relatively long half-life, and GGT can be increased by liver injury caused by situations other than drinking (6).
CDT is drawing attention as a new indicator related to heavy drinking. American Psychiatric Association (7) recommended CDT as a useful marker monitoring recurrence of alcoholic disease. The US FDA also certified it alone among various biological indicators as the most specific indicator to heavy drinking (8). Serum transferrin is a glycoprotein conveying iron and exists in serum in several forms depending on the degree of its bond with carbohydrate. That is, according to the degree of sialylation, it takes one of forms such as pentasialo-transferrin, tetrasialo-transferrin, trisialo-transferrin, disialo-transferrin, monosialo-transferrin, and asialo-transferrin (9). The degree of transferrin's bond with carbohydrate is determined by the activity of glycosyltransferase that joins carbohydrate with transferrin and sialidase that removes carbohydrate from transferrin. Transferrin exists mostly in the form of tetrasialo-transferrin in normal people's serum. Because alcohol and acetaldehyde hinders transferrin from joining with carbohydrate by suppressing the activity of glycosyltransferase and by increasing the activity of sialidase, heavy drinking increases transferrin in the forms of asialo-transferrin, monosialo-transferrin, and disialo-transferrin, which have a low degree of bond with carbohydrate (10). Such types of transferrin are called CDT. Different from GGT, the concentration of CDT in blood is not affected by the drugs prescribed by general physicians (11). In addition, it is known to be more sensitive and specific than GGT in diagnosing heavy drinking or alcohol dependence (12).
Nevertheless, experiments or researches on CDT have been insufficient in Korea. This study was carried out in order to evaluate the clinical usefulness of CDT in Korean male drinkers.
The subjects of this study were 143 males who visited the Department of Family Medicine of Chungnam National University Hospital for health promotion during the period from March 2004 to March 2005, and they agreed to participate in the research. The subjects were limited to those who were negative for HBsAg and AntiHCV test, showed neither any mass in the liver nor any abnormality in the biliary tract in abdominal ultrasonography, were not suspected to have liver cirrhosis on blood tests and liver ultrasonography, and had never taken medicine during the previous one month. The ethics committee of Chungnam National University Hospital approved this study.
The quantity of drinking was measured using the timeline followback method (13), which collects detailed information on a person's daily drinking using a table for a specific period particularly 1-12 months before visiting. The quantity of drinking was represented as the mean weekly quantity of drinking during the previous one month based on the standard drink (4). Those who drank 14 drinks or less per week were classified into the moderate drinking group and those who drank more than 14 drinks into the heavy drinking group.
Indicators tested were %CDT, GGT, AST, and ALT. The serum level of CDT was measured through %CDT turbidimetric immunoassay (TIA) (Bio-Rad, Hercules, CA, U.S.A.) (14). The %CDT TIA is a heterogeneous immunoassay with column separation followed by turbidimetric measurement. The assay measures the relative amount of CDT in proportion to total transferrin and reports in %CDT.
Student's t-test was used to compare the heavy drinking group with the moderate drinking group in terms of age, body mass index (BMI), weekly quantity of drinking, %CDT, GGT, AST, and ALT. Pearson's correlation analysis was conducted by the two-tailed significance method in order to examine the relationships among %CDT, GGT, AST, ALT, and weekly quantity of drinking.
Sensitivity, specificity, and the positive and negative predictive values of %CDT, GGT, AST, and ALT for heavy drinking were investigated. Differences in the diagnostic usefulness of %CDT, GGT, AST, and ALT for detecting the male heavy drinking group were obtained by comparing the area under the curve (AUC) of the receiver operating characteristic curve (ROC curve). All statistical analyses were done using SPSS for Windows, and we set the significance level at 0.05.
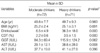
The mean (±SD) age of the subjects was 49.63 (±8.56) yr. According to the results of t-test, no significant difference was observed between the moderate drinking group (n=72) and the heavy drinking group (n=71) in age (p=0.983), BMI (p=0.891), GGT (p=0.062), and ALT (p=0.396). The weekly quantity of drinking (p=0.000), %CDT (p=0.000), and AST (p=0.008) were significantly higher in the heavy drinking group (Table 1).
The optimal cut off point of %CDT to heavy drinking on the ROC curve was 2.4%, at which the sensitivity, specificity, positive predictive value, and negative predictive value of %CDT to heavy drinking were 83.1%, 63.9%, 69.4%, and 79.3%, respectively. The optimal cut off point of GGT on the ROC curve was 60.0 IU/L, at which the sensitivity, specificity, positive predictive value, and negative predictive value of GGT to heavy drinking were 67.6%, 45.8%, 55.2%, and 58.9%, respectively. The optimal cut off point of AST on the ROC curve was 31.0 IU/L, at which the sensitivity, specificity, positive predictive value, and negative predictive value of AST to heavy drinking were 52.1%, 72.2%, 64.9%, and 60.5%, respectively. The optimal cut off point of ALT on the ROC curve was 36.0 IU/L, at which the sensitivity, specificity, positive predictive value, and negative predictive value of ALT to heavy drinking were 46.5%, 54.2%, 50.0%, and 50.6%, respectively (Table 3).
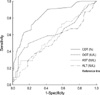
Among the ROC curves of the indicators, that of %CDT appeared to be closest to the top left end. The AUC (95% confidence interval) of the ROC curves for %CDT, GGT, AST and ALT was 0.823 (0.755-0.891), 0.578 (0.484-0.673), 0.622 (0.528-0.717), and 0.516 (0.420-0.613), respectively. Thus, %CDT showed the largest AUC (Fig. 1).
Among the biological indicators, diagnostic sensitivity for heavy drinking was relatively high in %CDT and GGT, and specificity was high in AST and %CDT. With regard to positive and negative predictive values, they were relatively high in %CDT and AST. The results seem to be consistent with previous researches performed in the other cultures by Stibler et al. (10) and Huseby et al. (15). Two studies in Korea had examined the usefulness of %CDT as a diagnostic marker for alcohol dependence. Shin et al. (16) reported the sensitivity, specificity, positive predictive value, and negative predictive value of %CDT to alcohol dependence as 85.1%, 93.3%, 88.7%, and 90.6%, respectively. Our study showed those of %CDT to heavy drinking were 83.1%, 63.9%, 69.4%, and 79.3%, respectively. The differences in subjects need to be considered in the interpretation of the numerical differences in the percentages of the results because, unlike our study that was designed for the males with heavy drinking, the study by Shin et al. was performed on the patients with alcohol dependence without discrimination of sex of the subjects. Hur et al. (17) reported the AUC of the ROC curves to alcohol dependence was the largest for %CDT among the three markers; %CDT, GGT, and MCV. Our study also showed similar finding that the AUC of %CDT to heavy drinking was the largest among the four markers; %CDT, GGT, AST, and ALT. These findings suggest that %CDT is more useful in the diagnosis of alcohol dependence and heavy drinking than existing biological indicators such as AST, ALT, GGT, and MCV.
Through this research the authors could confirm the opinion by Kim et al. (18) that %CDT can reflect the weekly drinking amount and can be a potential biological marker for the purpose of quantitative monitoring the drinking behavior of Korean male heavy drinkers. Our study showed that %CDT did not show any correlations with other indicators except AST, but AST showed high correlations with other two liver enzymes. This finding seems to be consistent with the report by Meerkerk et al. (19) that generally AST, ALT, and GGT increase after liver cell damage by alcohol, whereas CDT increases after heavy drinking, independent of liver cell damage.
In the current situation that CDT has not been examined enough in Korea, the present research is one of a few studies on the usefulness of CDT in screening heavy drinkers in Korea. The results of our research were consistent with previous researches from foreign countries; however, this study has a limitation in that it was conducted on only male subjects. To strengthen the usefulness of CDT in the Korean population, further studies are needed on other population characteristics such as sex and specific age groups.
Figures and Tables
Fig. 1
Receiver operating characteristic curves of %CDT, GGT, AST, and ALT for detection of heavy drinkers.
References
1. Korean National Statistical Office. 2005 social indicators in Korea. 2006. Korean National Statistical Office.
2. Lee CK, Lee KH. A national epidemiological study of mental disorders in Korea (15)-prevalence of alcoholism. J Korean Neuropsychiatr Assoc. 1994. 33:832–845.
3. Schuckit MA. Why don't we diagnose alcoholism in our patients? J Fam Pract. 1987. 25:225–226.
4. US Department of Agriculture. Dietary guidelines for Americans. 2005. US Department of Agriculture;43–46.
5. Kim JS. Diagnosis and treatment of alcohol use disorders. J Korean Acad Fam Med Suppl. 2004. 25:256–265.
7. American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 2000. 4th edition. Washington DC: American Psychiatric Association;text revision.
8. Arndt T. Carbohydrate-deficient transferrin as a marker of chronic alcohol abuse: a critical review of preanalysis, analysis, and interpretation. Clin Chem. 2001. 47:13–27.

9. Wong KL, Regoeczi E. Some observations on the carbohydrate composition of purified transferrin. Int J Pept Protein Res. 1977. 9:241–248.

10. Stibler H. Carbohydrate-deficient transferrin in serum: a new marker of potentially harmful alcohol consumption reviewed. Clin Chem. 1991. 37:2029–2037.

11. Stibler H, Borg S, Joustra M. Micro anion exchange chromatography of carbohydrate-deficient transferrin in serum in relation to alcohol consumption (Swedish patent 8400585-5). Alcohol Clin Exp Res. 1986. 10:535–544.
12. Allen JP, Sillanaukee P, Anton R. Contribution of carbohydrate deficient transferrin to gamma glutamyl transpeptidase in evaluating progress of patients in treatment for alcoholism. Alcohol Clin Exp Res. 1999. 23:115–120.

13. Sobell LC, Sobell MB. Litten RZ, Allen JP, editors. Timeline followback technique: a technique for assessing self-reported alcohol consumption. Measuring alcohol consumption: psychosocial and biochemical methods. 1995. Totowa NJ: Humana Press;41–72.
14. Bio-rad. Instruction manual for %CDT TIA. 2002. USA: Bio-rad;1–32.
15. Huseby NE, Nissen O, Erfurth A, Wetterling T, Kanitz RD. Carbohydrate-deficient transferrin and alcohol dependency: variation in response to alcohol intake among different groups of patients. Alcohol Clin Exp Res. 1997. 21:201–205.

16. Shin MG, Ryang DW. Serum level of carbohydrate deficient transferrin and genetic polymorphisms of cytochrome P4502E1 in patients with alcoholism. Korean J Lab Med. 2004. 24:160–165.
17. Hur MN, Lee KM, Shin DH, Cho HC, Kim SK, Choi IG. Diagnostic utility of carbohydrate-deficient transferrin as a marker of alcohol dependence. Korean J Lab Med. 2004. 24:40–44.
18. Kim JS, Oh MK, Kim SS, Park BK, Jung JK, Kwon KC, Park JW, Kim GJ. Can carbohydrate-deficient transferrin (CDT) reflect alcohol consumption in Korean male drinkers? J Korean Acad Fam Med. 2005. 26:451–455.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download