Abstract
Macrophage infiltration has been observed in the renal biopsy specimens of diabetic nephropathy (DN), and hyperglycemic state stimulates the renal expression of RANTES (regulated upon activation, normal T-cell expressed and secreted) and MCP-1 (monocyte chemoattractant protein-1). Upregulation of RANTES and MCP-1 with infiltrating macrophages may play a crucial role in the development and progression of DN. Genetic polymorphisms of RANTES and its receptors were reported to be independent risk factors for DN. We genotyped single nucleotide polymorphism (SNPs) in the MCP-1 G-2518A, CCR2 G46295A, RANTES C-28G and G-403A in 177 diabetic end-stage renal disease (ESRD) patients and 184 patients without renal involvement (controls) in order to investigate the effects of these SNPs on DN in Korean patients with type 2 DM. There were no differences in the frequencies of SNPs and the distribution of haplotypes of RANTES promoter SNPs between two groups. In conclusion, there were no associations of MCP-1, CCR2 and RANTES promoter SNPs with diabetic ESRD in Korean population. Prospective studies with clearly-defined, homogenous cohorts are needed to confirm the effect of these genetic polymorphisms on DN.
Diabetic nephropathy is the leading cause of chronic kidney disease in Korea, and accounts for 43% of new dialysis patients in 2004. Nephropathy complicates only 20-40% of cases of type 2 diabetes, which suggests several genetic factors would play an important role in the development of nephropathy.
Recently, inflammatory cells, especially macrophages and related chemokines, are suggested to be involved in the development and progression of diabetic nephropathy (1). In streptozotocin-induced diabetic rat model, hyperglycemia is followed by early macrophage recruitment (2). Also, macrophage infiltration is observed during the moderate stage of diffuse diabetic glomerulosclerosis in the kidney biopsy specimen from diabetic patients (3). Infiltrated macrophages release various inflammatory mediators, such as IL-1, TNF-α, and TGF-β that result in inflammation, interstitial fibrosis, and finally permanent kidney damage.
MCP-1 (Monocyte chemoattractant protein-1) and RANTES (regulated upon activation, normal T-cell expressed and secreted) are the most potent chemokines that recruit monocyte/macrophages to the damaged tissues. A high glucose concentration in the culture medium stimulated the MCP-1 expression in human mesangial cells (4). Urinary MCP-1 levels were significantly elevated in patients with diabetic nephropathy and advanced tubulointerstitial lesions. Moreover, urinary levels of MCP-1 were well correlated with the number of CD68-positive infiltrating cells in the interstitium (5). In addition, ACE inhibitor, lisinopril treatment for one year improved renal function, reduced proteinuria, and significantly decreased urinary MCP-1 levels in patients with diabetic nephropathy (6). All of these observations suggest that macrophages and associated chemokines may be involved in the development and progression of diabetic nephropathy.
Recently, RANTES promoter single nucleotide polymorphism (SNP) -28G genotype and its major receptor, chemotactic cytokine receptor 5 (CCR5) promoter 59029A genotype were shown to be associated with diabetic nephropathy in patients with type 2 diabetes (7, 8). However, effects of MCP-1 and its receptor CCR2 polymorphisms have not been fully assessed so far on diabetic nephropathy.
The authors investigated the effects of these SNPs-MCP-1, CCR2 and RANTES-on diabetic nephropathy in Korean patients with type 2 diabetes.
We studied 361 unrelated patients with type 2 diabetes comprising two groups according to the following criteria: 1) control subjects (n=184), patients with diabetic retinopathy and a duration of type 2 diabetes of >15 yr, but without signs of renal involvement, i.e., a urinary albumin to creatinine ratio of <30 mg/g and with a creatinine clearance (using the Cockroft-Gault formula) of >60 mL/min/m2; or 2) ESRD cases (n=177), patients with diabetic retinopathy and ESRD due to type 2 diabetes as indicated by a creatinine clearance rate of <15 mL/min/m2 or who were on renal replacement therapy. We excluded subjects with ESRD with any one of the following criteria: 1) those without retinopathy; 2) a consistent hematuria history before renal failure; 3) no past history of proteinuria before renal failure; 4) contracted kidneys on imaging study; and 5) those suspected to have non-diabetic glomerular diseases. Patients with family history of diabetic ESRD were also excluded because the unknown genetic factors specific to those families could interfere the effects of polymorphisms. All subjects enrolled in this study were of Korean ethnicity. Type 2 diabetes was diagnosed based in the World Health Organization criteria. Subjects positive for GAD antibodies and who started insulin treatment within 1 yr of diagnosis, and those who were prone to ketosis were excluded. The Institutional Review Board of the Clinical Research Institute at Seoul National University Hospital approved the study protocol, and informed consent for genetic analysis was obtained from each subject.
Genomic DNA was extracted from peripheral blood cells, and then we genotyped G-2518A in the MCP-1 promoter region, G46295A in the CCR2 gene, C-28G and G-403A in the promoter region of the RANTES gene. Briefly, for the genotyping of polymorphic sites, amplification and extension primers were designed for single-base extension (SBE) (9). Primer extension reactions were performed with SNaP-shot ddNTP Primer Extension Kit (Applied Biosystems, Foster City, CA, U.S.A.). To clean up the product of the primer extension reaction, one unit of SAP was added to the reaction mixture and the mixture was incubated at 37℃ for 1 hr, followed by 15 min at 72℃ for enzyme inactivation. The DNA samples, containing extension products, and Genescan 120 Liz size standard solutions were added to Hi-Di formamide (Applied Biosystems). The mixture was incubated at 95℃ for 5 min, followed by 5 min on ice and then analyzed by electrophoresis on the ABI Prism 3100 Genetic Analyzer (Applied Biosystems). The results were analyzed using the software GeneScan and Genotyper (Applied Biosystems). Haplotypes for the SNP C-28G and G-403A in the RANTES gene were determined using the PHASE (version 2.3) software (10).
The data were expressed as means±standard deviation. Chi-square test and Fisher's exact test, as appropriate, were used to test differences between the ESRD and control groups for significance. To assess the relationship of genotypes with nephropathy, multiple logistic regression analysis was performed using the SPSS statistical package (SPSS Inc. Chicago, IL, U.S.A.). A p value less than 0.05 was considered statistically significant.
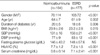
We studied 361 patients with type 2 diabetes, comprising 177 patients with ESRD (ESRD group) and 184 patients with diabetic retinopathy and duration of type 2 diabetes of >15 yr but without evidence of renal disease (the control group). The clinical characteristics of these groups are summarized in Table 1. There were significant differences in the male-to-female ratio (1.46:1 in ESRD vs. 0.61:1 in controls, p<0.001) and mean (±SD) age (61±9 in ESRD vs. 64±7 in controls, p=0.002). Systolic/diastolic blood pressure of the ESRD groups was also higher than those of control groups (150±21/83±12 mmHg vs. 131±16/77±9 mmHg, p<0.001).
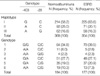
Genotype distributions for the polymorphisms of MCP-1 G-2518A, CCR2 G46295A, RANTES C-28G and G-403A are presented in Table 2. The distributions of these genotypes were in Hardy-Weinberg equilibrium, indicating a lack of selection for or against each. The genotype frequencies of those SNPs were not different between two groups.
We observed six genotypes of RANTES C-28G and G-403A polymorphisms. RANTES -28G/G was not found in subjects with the -403G allele, while RANTES -403G/G was not observed in subjects with the -28G allele. Therefore, there were three haplotypes of the RANTES promoter region (haplotypes I, II, and III in Table 3). This is consistent with the results of previous studies (7, 11). The frequencies of haplotypes I, II, and III in ESRD groups were 63.6%, 20.1%, and 16.3%, and those in control groups were 58.2%, 25.0%, and 16.8%, respectively. There were no significant differences in the frequencies of each genotype and haplotype between two groups.
Macrophages are not only the major effecter cells in innate immune response but are also one of the central mediators of renal vascular inflammation, and their accumulation is known to be one of the characteristic features of diabetic nephropathy (1). Infiltrated macrophages are found within kidney tissues from diabetic nephropathy patients (3), and macrophage-derived products can induce further inflammation in the diabetic kidney. In a streptozotocin-induced diabetic rat model, macrophages were recruited within glomeruli at the very early stage of hyperglycemia, and macrophage recruitment was associated with an increase in alpha chain type IV collagen mRNA and glomerular hypertrophy (2). In addition, glomerular expression of VCAM-1 (vascular cell adhesion molecule-1), ICAM-1 (intracellular adhesion molecule-1), and MCP-1 increased in advance, which have been shown to be important in macrophage accumulation and renal injury in models of nondiabetic and diabetic kidney (12, 13).
MCP-1, also termed monocyte chemotactic and activating factor (MCAF) or CCL2, is a potent chemokine that is known to affect both macrophage accumulation and its function. Urinary MCP-1 levels were increased in patients with diabetic nephropathy and advanced tubulointerstitial lesion and there were MCP-1 positive cells in the intersititium in the kidney tissues (5). Also, urinary MCP-1 levels correlate with urinary excretion level of albumin in human diabetic kidney (14). Moreover, blockade of the renin-angiotensin system reduced urinary MCP-1 levels, lowered glomerular expression of MCP-1, decreased macrophage infiltration, and improved renal function (6, 15, 16). These findings suggest that renoprotection conferred by renin-angiotensin blockade is at least partly dependent on the inhibition of macrophage infiltration and interstitial fibrosis mediated by MCP-1.
Recently, Chow et al. showed that the macrophage infiltration and renal injury were markedly suppressed in diabetic MCP-1 (-/-) mice compared to MCP-1 (+/+) mice despite the equivalent blood glucose and hemoglobin A1c levels (17). This study further supports the importance of MCP-1 mediated accumulation and activation of macrophage in the development of diabetic nephropathy.
RANTES is another chemokine that has been shown to be important in macrophage recruitment and renal injury. However, little is known about the pathogenic role in diabetic nephropathy. Previous studies using renal allograft model showed that Met-RANTES, a chemokine receptor antagonist, suppressed recruitment of inflammatory cells, mainly monocytes, into renal allografts, reduced proteinuria and significantly ameliorated glomerulosclerosis, interstitial fibrosis, and tubular atrophy (18).
We hypothesized that genetic variability in the expression of MCP-1 and RANTES may influence the development of diabetic nephropathy
There are few studies that examined the associations between chemokine gene polymorphisms and nephropathy in type 2 DM. Nakajima et al. reported that the RANTES promoter -28G genotype and the major RANTES receptor, CCR5, promoter 59029A genotype were associated with the diabetic nephropathy (7, 8). However, existing data for most of polymorphism studies in diabetic nephropathy are inconclusive because of the small sample size and heterogeneity of type 2 diabetes itself. Therefore, we defined type 2 diabetic patients with DM duration of more than 15 yr but no signs of renal involvement as the control group, and patients with DM ESRD as the nephropathy group in order to improve the statistical power given the relatively small sample size. It is well known that about 90% of diabetic individuals have type 2 DM, and within this category no more than 10% can be accounted for by monogenic forms such as maturity onset diabetes of the young (MODY) and mitochondrial diabetes or late-onset autoimmune diabetes of the adult, which is actually a late-onset type 1 diabetes. Also, 20-30% of patients with type 2 DM may progress to a significant degree of renal impairment while remaining normoalbuminuric (19). It has been suggested that "age-associated" renal senescence, interstitial fibrosis, and ischemic vascular disease, such as atherosclerotic involvement of the renal artery and intrarenal vascular disease may contribute the renal progression (20). Thus we selected the nephropathy group by the strict clinical criteria, and excluded normoalbuminuric patients with reduced creatinine clearance from the control group.
To our knowledge, this is the first study investigating the association between the MCP-1 SNP and diabetic nephropathy in Korea, involving a well-controlled study with clearly-defined subjects. In the present study, the distribution of SNPs in the regulatory region of MCP-1, RANTES, and CCR2 did not differ between the diabetic patients without nephropathy and the diabetic ESRD patients. This is not consistent with the previous study from the Japanese population (7). Differences in the study design and patient selection criteria, e.g. normoabuminuria vs. microalbuminuria vs. macroalbumnuria group, may explain the conflicting result.
It is also possible that the subjects with ESRD and high risk genotypes may be excluded from the present study because of premature mortality due to cardiovascular events. In Caucasian type 2 DM patients on hemodialysis, carriers of the RANTES -403A allele had an 81% higher risk for all-cause mortality, mainly due to cardiac events (21). Since chemokines and macrophages are important in the development of atherosclerosis as well as nephropathy, it cannot be ruled out that high risk genotypes affected not only microvascular but also macrovascular complications. It may be postulated that carriers of the RANTES -403A genotype are more subject to atherosclerosis and premature death due to cardiovascular diseases before progressing to ESRD, whereas carriers of RANTES -403G genotype live long enough to reach ESRD.
More importantly, the other possibility is that chemokine-mediated macrophage recruitment might play a pivotal role in the earlier stage of diabetic nephropathy than the advanced stage as in our nephropathy group, and other factors may be involved in the progression of diabetic nephropathy to ESRD. Subjects in the nephropathy group were slightly younger and had more male subjects. However, this reflects the real world, and there were no differences in the genotype frequencies when stratified by sex and age (data not shown).
In conclusion, there were no associations of MCP-1, CCR2 and RANTES promoter SNPs with diabetic ESRD in the Korean population. Prospective studies with clearly-defined, homogenous cohorts are needed to confirm the effect of these genetic polymorphisms on diabetic nephropathy.
Figures and Tables
ACKNOWLEDGMENTS
We thank Kang E-T, Kim JC, Kim SG, Lee JG, and Oh JE for their help in recruiting the subjects and collecting the data.
References
1. Galkina E, Ley K. Leukocyte recruitment and vascular injury in diabetic nephropathy. J Am Soc Nephrol. 2006. 17:368–377.

2. Sassy-Prigent C, Heudes D, Mandet C, Belair MF, Michel O, Perdereau B, Bariety J, Bruneval P. Early glomerular macrophage recruitment in streptozotocin-induced diabetic rats. Diabetes. 2000. 49:466–475.

3. Furuta T, Saito T, Ootaka T, Soma J, Obara K, Abe K, Yoshinaga K. The role of macrophages in diabetic glomerulosclerosis. Am J Kidney Dis. 1993. 21:480–485.

4. Ihm CG, Park JK, Hong SP, Lee TW, Cho BS, Kim MJ, Cha DR, Ha H. A high glucose concentration stimulates the expression of monocyte chemotactic peptide 1 in human mesangial cells. Nephron. 1998. 79:33–37.

5. Wada T, Furuichi K, Sakai N, Iwata Y, Yoshimoto K, Shimizu M, Takeda SI, Takasawa K, Yoshimura M, Kida H, Kobayashi KI, Mukaida N, Naito T, Matsushima K, Yokoyama H. Up-regulation of monocyte chemoattractant protein-1 in tubulointerstitial lesions of human diabetic nephropathy. Kidney Int. 2000. 58:1492–1499.

6. Amann B, Tinzmann R, Angelkort B. ACE inhibitors improve diabetic nephropathy through suppression of renal MCP-1. Diabetes Care. 2003. 26:2421–2425.

7. Nakajima K, Tanaka Y, Nomiyama T, Ogihara T, Ikeda F, Kanno R, Iwashita N, Sakai K, Watada H, Onuma T, Kawamori R. RANTES promoter genotype is associated with diabetic nephropathy in type 2 diabetic subjects. Diabetes Care. 2003. 26:892–898.

8. Nakajima K, Tanaka Y, Nomiyama T, Ogihara T, Piao L, Sakai K, Onuma T, Kawamori R. Chemokine receptor genotype is associated with diabetic nephropathy in Japanese with type 2 diabetes. Diabetes. 2002. 51:238–242.

9. Vreeland WN, Meagher RJ, Barron AE. Multiplexed, high-throughput genotyping by single-base extension and end-labeled free-solution electrophoresis. Anal Chem. 2002. 74:4328–4333.

10. Stephens M, Smith NJ, Donnelly P. A new statistical method for haplotype reconstruction from population data. Am J Hum Genet. 2001. 68:978–989.

11. Liu H, Chao D, Nakayama EE, Taguchi H, Goto M, Xin X, Takamatsu JK, Saito H, Ishikawa Y, Akaza T, Juji T, Takebe Y, Ohishi T, Fukutake K, Maruyama Y, Yashiki S, Sonoda S, Nakamura T, Nagai Y, Iwamoto A, Shioda T. Polymorphism in RANTES chemokine promoter affects HIV-1 disease progression. Proc Natl Acad Sci USA. 1999. 96:4581–4585.

12. Chow F, Ozols E, Nikolic-Paterson DJ, Atkins RC, Tesch GH. Macrophages in mouse type 2 diabetic nephropathy: correlation with diabetic state and progressive renal injury. Kidney Int. 2004. 65:116–128.

13. Anders HJ, Vielhauer V, Schlondorff D. Chemokines and chemokine receptors are involved in the resolution or progression of renal disease. Kidney Int. 2003. 63:401–415.

14. Morii T, Fujita H, Narita T, Shimotomai T, Fujishima H, Yoshioka N, Imai H, Kakei M, Ito S. Association of monocyte chemoattractant protein-1 with renal tubular damage in diabetic nephropathy. J Diabetes Complications. 2003. 17:11–15.

15. Kato S, Luyckx VA, Ots M, Lee KW, Ziai F, Troy JL, Brenner BM, Mackenzie HS. Renin-angiotensin blockade lowers MCP-1 expression in diabetic rats. Kidney Int. 1999. 56:1037–1048.

16. Lee FT, Cao Z, Long DM, Panagiotopoulos S, Jerums G, Cooper ME, Forbes JM. Interactions between angiotensin II and NF-κB-dependent pathways in modulating macrophage infiltration in experimental diabetic nephropathy. J Am Soc Nephrol. 2004. 15:2139–2151.

17. Chow FY, Nikolic-Paterson DJ, Ozols E, Atkins RC, Rollin BJ, Tesch GH. Monocyte chemoattractant protein-1 promotes the development of diabetic renal injury in streptozotocin-treated mice. Kidney Int. 2006. 69:73–80.

18. Song E, Zou H, Yao Y, Proudfoot A, Antus B, Liu S, Jens L, Heemann U. Early application of Met-RANTES ameliorates chronic allograft nephropathy. Kidney Int. 2002. 61:676–685.

19. MacIsaac RJ, Tsalamandris C, Panagiotopoulos S, Smith TJ, McNeil KJ, Jerums G. Nonalbuminuric renal insufficiency in type 2 diabetes. Diabetes Care. 2004. 27:195–200.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download