Abstract
We report a surgical case of primary polymorphous low-grade adenocarcinoma (PLGA) of the minor salivary gland-type of the lung. A PLGA originating from the right upper lobar bronchial inlet was successfully treated by sleeve right upper lobectomy. PLGAs are thought to be indolent tumors that are preferentially localized to the palate, and they affect the minor salivary glands almost exclusively. Until now, two cases of distant metastases to the lung have been reported in the English literature. To the best of our knowledge, only one case of PLGA of minor salivary gland-type of the lung without evidence of a previous oropharyngeal primary tumor has been reported in the English literature. But the case was not a single lesion; it was bilateral tumors accompanied by tumors of the cervical lymph nodes. We report here the first case of a single primary PLGA of the minor salivary gland-type of the lung, which was successfully treated by sleeve bronchial resection of right upper lobe.
Polymorphous low-grade adenocarcinoma (PLGA) is a low-grade malignant infiltrative tumor of the minor salivary gland. The term polymorphous low-grade adenocarcinoma of the minor salivary glands was coined in 1984 by Evans and Batsakis (1), to reflect this tumor's morphologic appearance and clinical behavior. PLGAs are thought to be indolent tumors that are localized preferentially to the palate and almost exclusively affect the minor salivary glands. The local recurrence rates range from 10% to 20%, and metastases to locoregional lymph nodes occur in only 6-10% of the cases (2, 3).
Metastasis of this tumor to the lung occurs very rarely, and there have been only two reported cases, which were both microscopically confirmed (4, 5). Lee and his associates (6) reported the first clinical case of primary lung tumor of this type in 2004. But the patient presented with bilateral lung tumors and low cervical and supraclavicular lymph node involvement, and the possibility of metastases from an unknown primary tumor was not completely ruled out.
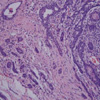
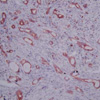
A 66-yr-old woman was admitted to the department of pulmonology due to her chronic and recently aggravated dyspnea. She had been treated for three years at another hospital under the diagnosis of asthma. The patient was referred to the department of pulmonology at our hospital. The finding of collapse and consolidation of the anterior segment of the right upper lobe was noted on her chest radiography (Fig. 1A). The bronchoscopic examination revealed a cystic fungating mass that nearly obstructing the inlet of the right main bronchus (Fig. 1B). A portion of the mass was hyperemic, and the biopsy from the periphery of the mass revealed a few atypical spindle cell proliferations in the stroma. The tentative diagnosis did not exclude the possibility of a spindle cell neoplasm. The patient was referred to the department of thoracic and cardiovascular surgery for surgical intervention. Preoperative chest CT scanning revealed about a 1.8-cm sized slightly lobulated and mildly heterogeneously enhancing endobronchial mass at the right main bronchus and the upper lobar bronchus with resultant postobstructive pneumonia in the right upper lobe and right middle lobe. The tracheobronchial lymph nodes and the subcarinal nodes were also noted to be enlarged. The patient was in the high risk group for pneumonectomy and the parameters of the lung function test were as followings; forced vital capacity (FVC) of 1.04 L and 47% of the predicted value, forced expired volume in 1 second (FEV1) of 0.76 L and 48% of the predicted value, residual volume (RV) of 2.49 L and 177% of predicted value, and diffusing capacity for carbon monoxide (DLCO) of 7.1 mL/mmHg/min and 51% of the predicted value. The operation of sleeve right upper lobectomy and mediastinal lymph node dissection was performed. The mass was found to have originated from the right upper lobar bronchial inlet, and it was about 1.0×0.7 cm in size upon fixation with formalin. The mass was lobulated, and the cut surface of the tumor was soft and tan-yellow. The microscopic findings revealed a low grade, infiltrating tumor with a mixed growth pattern: there were ductal, tubular, cystic and trabecular patterns. No definite cartilagenous differentiation was observed. Most of the tumor cells had bland-appearing nuclei and finely speckled chromatin; the cytoplasm was relatively scanty (Fig. 2, 3). Immunohistochemically, the tumor cells were positive for cytokeratin, epithelial membrane antigen (Fig. 4), S-100 protein and smooth muscle actin; they were negative for carcinoembryonic antigen (CEA), alpha-1-antitrysin and lysozyme. The bronchial cut margin was free from tumor infiltration, and there was no evidence of invasion to the visceral pleura, the lymphovascular structures and the perineural structures. The dissected lymph nodes were 13 in number and they were as follows; tracheobronchial nodes, hilar nodes, subcarinal nodes and interlobar nodes. The dissected lymph nodes were all negative for tumor invasion.
Her postoperative clinical course was uneventful, and she was discharged on her 9th postoperative day (Fig. 1C, D). Her head and neck examination was performed after we obtained the pathologic report. The study included a clinical examination of the oropharynx and laryngoscopy, and computer-assisted tomography (CAT) scans of the head and neck were done. She underwent the whole-body positron emission tomography (PET) scan 2 months after the operation. All the above examinations did not reveal any primary lesion outside the chest. She is still stable without any respiratory symptoms at the time of this report and the parameters of her lung function test, performed 2 months after the operation, were as followings; FVC of 2.37 L and 106% of the predicted value, FEV1 of 1.69 L and 107% of the predicted value, RV of 1.11 L and 78% of predicted value, and DLCO of 13.4 mL/mmHg/min and 88% of the predicted value.
Although not commonly, it is well recognized that salivary gland-type tumors can also occur in the lung. These are thought to arise from the mucous glands that line the bronchial tree. The most common salivary gland-type tumors that arise in the lung are adenoid cystic carcinoma and mucoepidermoid carcinoma. Polymorphous low-grade adenocarcinoma (PLGA) is a low-grade malignant infiltrative tumor of the minor salivary gland that displays bland-looking tumor cells and a diverse range of architectural patterns; this tumor was first described by Evans and Batsakis in 1984 (1). Since its original description and acceptance as a separate entity, more than 200 cases of this tumor have been reported. PLGA comprises 7.4% of the minor salivary gland tumors and 19.6% of those that are malignant (7). Despite its bland morphologic appearance, there are also a few reported cases where the tumor has undergone differentiation to a high-grade carcinoma, and often after a considerable period of years since the diagnosis (8). A large study of 164 cases (9) has shown that 97.6% of all patients were alive or they had died of unrelated disease after a mean follow-up period of 115.4 months after the treatment with surgical excision only. Complete surgical excision is the treatment of choice. The macroscopic examination usually displays a circumscribed but nonencapsulated, often lighttan to gray mass. Microscopically, as the name suggests, the tumor has a diverse range of growth patterns that may include tubules, trabeculae, single-cell files, solid nests, and fascicles, or cribriform, papillary or cystic structures. Unifying all these different patterns is the cytologic uniformity of the tumor cells, and these cells exhibit a bland or low-grade cytologic appearance. Immunohistochemically, the tumor cells show diffuse moderate to strong staining for epithelial markers, epithelial membrane antigen (EMA), S-100 and vimetin. Staining for smooth muscle actin is usually negative or weakly positive and focal. The tumor is generally negative for glial fibrillary acidic protein and monoclonal CEA.
Knowledge concerning the tumor site is rather important. A tumor arising in a central bronchial site would raise the possibility of a primary salivary gland tumor, as opposed to a conventional adenocarcinoma that is usually peripherally located. The markers CEA and TTF-1 could also be useful targets for antibody testing, as they are quite specific to lung adenocarcinoma. It is also important to distinguish this tumor from other types of salivary gland tumors, especially pleomorphic adenoma, adenoid cystic carcinoma (ACC), and mucoepidermoid carcinoma. The first tumor is benign, whereas the latter two malignant tumors have a more aggressive behavior compared to PLGA. Unlike PLGA, pleomorphic adenoma is a noninfiltrative, well-circumscribed tumor that consists of a biphasic population of epithelial and myoepithelial cells within a chondromyxoid stroma. Pleomorphic adenoma does not demonstrate perineural or stromal invasion. Adenoid cystic carcinoma shows a greater number of angular, pleomorphic nuclei and increased mitotic activity, as compared with the nuclei seen in PLGA, which are slightly larger, rounder and more uniform. The cytoplasm of the tumor cells is usually more eosinophillic in PLGA, whereas it is clearer in ACC. ACC shows EMA staining that is confined to the glandular lumina, and there is weak and patchy S-100 protein staining. In contrast, PLGA shows more diffuse EMA staining and more intense staining for S-100 protein. Mucoepidermoid carcinomas usually show definite squamoid or intermediate cells.
Although there are few reports on primary PLGAs of the lung, given the presence of minor salivary glands in the bronchial glands, this tumorous malady is theoretically possible (6). Primary PLGA of the minor-salivary gland-type of the lung had not been reported until 2004, when Lee and associates (6) reported a patient who had presented with bilateral lung tumors and low cervical and supraclavicular lymph nodes involvement without a known history of any previous or concurrent tumor or any oral surgery. The patient was managed by bilateral wedge resection of the lung. The patient underwent postoperative clinical examination including the laryngoscopy, CAT scans of the head, neck, chest and abdomen, and a whole-body PET scan, which did not reveal any primary lesion. However, the authors discussed a possitility that those lung tumors might have represented metastasis of unknown origin rather than primary lung tumors. In our case, the pathological features were typical of PLGA, where the tumor cells displayed a variety of growth patterns and they had a bland cytologic appearance, which was similar to its counterpart in the minor salivary gland. The diagnosis of PLGA was based on both the typical morphologic appearance and the immunohistochemical findings. There was no evidence of primary tumor outside the chest on the detailed head and neck examination including the laryngoscopy, chest CT scanning, and whole body PET-scanning.
The specific operative technique of bronchial sleeve resection was first performed by Price Thomas (10). It avoids the need for pneumonectomy and it spares the healthy lung tissue distal to the pathologic lesion. Benign or malignant tumors confined to the large bronchus can be successfully managed by sleeve lobectomy. Because the surgical risk is not higher than that for pneumonectomy, and a significantly better postoperative quality of life and physical activity is ensured by the preservation of the functioning and intact lung tissue, we regard this type of tumor with its low-grade malignant potential as being well suited for sleeve bronchial resection.
In conclusion, PLGA is a rare minor salivary gland-type tumor that has been thought to occur almost exclusively in the minor salivary glands in the oral cavity and the neck. However, PLGA should be considered in the differential diagnosis of patients presenting with low-grade gland-forming tumors of the lung. When this tumor originates from the large bronchus, it can be safely resected by the technique of bronchial sleeve resection.
Figures and Tables
Fig. 1
(A) Preoperative chest roentgenogram. (B) Preoperative bronchoscopic finding of the lobulated intraluminal mass in the right main bronchus. (C) Bronchoscopic finding on the 5th postoperative day. (D) Postoperative chest roentgenogram on the postoperative 9th day.

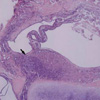
Fig. 2
The low-power view shows the various architectural patterns (arrow) including ductal, cystic and trabecular growth (H&E stain, ×40).
References
1. Evans HL, Batsakis JG. Polymorphous low-grade adenocarcinoma of minor salivary glands. A study of 14 cases of a distinctive neoplasm. Cancer. 1984. 53:935–942.

2. Vincent SD, Hammond HL, Finkelstein MW. Clinical and therapeutic features of polymorphous low-grade adenocarcinoma. Oral Surg Oral Med Oral Pathol. 1994. 77:41–47.

3. Gnepp DR, Chen JC, Warren C. Polymorphous low-grade adenocarcinoma of minor salivary gland. An immunohistochemical and clinicopathologic study. Am J Surg Pathol. 1988. 12:461–468.
4. Tanaka F, Wada H, Inui K, Mizuno H, Ike O, Yokomise H, Fukuse T, Hitomi S, Shoji K, Nakashima Y. Pulmonary metastasis of polymorphous low-grade adenocarcinoma of the minor salivary gland. Thorac Cardiovasc Surg. 1995. 43:178–180.
5. Hannen EJ, Bulten J, Festen J, Wienk SM, de Wilde PC. Polymorphous low grade adenocarcinoma with distant metastases and deletions on chromosome 6q23-qter and 11q23-qter: a case report. J Clin Pathol. 2000. 53:942–945.

6. Lee VK, McCaughan BC, Scolyer RA. Polymorphous low-grade adenocarcinoma in the lung: a case report. Int J Surg Pathol. 2004. 12:287–294.

7. Ellis LG, Auclair Paul L. Tumors of the Salivary Glands. atlas of tumor pathology. 1996. Washington, DC: Armed Forces Institute of Pathology;Third series. Fascicle no.17.
8. Simpson RH, Reis-Filho JS, Pereira EM, Ribeiro AC, Abdulkadir A. Polymorphous low-grade adenocarcinoma of the salivary glands with transformation to high-grade carcinoma. Histopathology. 2002. 41:250–259.

9. Castle JT, Thompson LD, Frommelt RA, Wenig BM, Kessler HP. Polymorphous low-grade adenocarcinoma: a clinicopathologic study of 164 cases. Cancer. 1999. 86:207–219.
10. Thomas PC. Conservative resection of the bronchial tree. J R Coll Surg Edinb. 1956. 1:169–186.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download