Abstract
We evaluated the safety and stability of the less-invasive submuscular bar fixation method in the Nuss procedure. One hundred and thirteen patients undergoing the Nuss procedure were divided into three groups according to the bar fixation technique employed. Group 1 consisted of 25 patients who had undergone bilateral pericostal bar fixation, group 2 consisted of 39 patients with unilateral pericostal one, and group 3 included 49 patients with bilateral submuscular one. The patients' age ranged from 2 to 25 yr, with an average of 7.2±5.67 yr. Bar dislocation occurred in 1 patient (4%) in Group 1, 2 patients (5.1%) in Group 2, and 1 patient (2.0%) in Group 3 (p=0.46). Hemothorax was noted in 2 patients (8%) in Group 1, 2 (5.1%) in Group 2, and none (0%) in Group 3 (Group 1 vs. Group 3, p=0.028). The mean operation time was shorter in Group 3 than Group 1 (50.1±21.00 in Group 3 vs. 67.2±33.07 min in Group 1, p=0.041). The submuscular bar fixation results in a decrease in technique-related complications and operation time and is associated with favorable results with regard to the prevention of bar dislodgement.
Pectus excavatum is a relatively common congenital chest wall deformity, which is often seen in conjunction with organic problems as well as cosmetic problems. Until recently, the most frequently performed operation for the correction of pectus excavatum has involved the removal of the abnormal cartilage, with preservation of the perichondrium as well as sternal elevation and stabilization (1).
In 1998, Nuss et al. published a report that described a minimally invasive technique for the remodeling of the anterior chest wall, employing a metal bar, and obviating the need for cartilage resection (2). This new approach was designed for better functional and cosmetic outcomes than invasive repairs.
One of the major problems associated with this new operation was the high risk of postoperative bar displacement (3). A lateral stabilizer is used during the Nuss procedure to prevent the bar from dislodging. However, Watanabe et al. reported that a lateral stabilizer is not always necessary for the prevention of bar displacement in small patients whose ribs and rib cartilage are still soft (4).
Nowadays, various pericostal bar fixation techniques are used extensively in the prevention of bar displacement (5-7). These techniques often successfully decrease the incidence of bar displacement, but are probably associated with increased risks of technique-related complications, such as hemothorax and pneumothorax, due to invasiveness of the procedure. In this study, our less invasive bar fixation method (submuscular bar fixation) for the Nuss procedure was evaluated with regard to the safety and stability.
From August 1999 to July 2004, 113 patients (82 males and 31 females) suffering from pectus excavatum underwent Nuss procedures at Guro Hospital, Korea University Medical Center. The patients' age ranged from 2 to 25 yr, with an average of 7.2±5.67 yr (median, 6.0 yr), and the mean Haller CT index was 4.31±1.12 (range, 2.4-7.56). All patients' data were retrospectively reviewed. Patients' follow-up is complete until present.
The submuscular bar fixation technique proceeds as follows: 1) 1 cm transverse incisions are made on the bilateral midaxillary line. 2) Serratus anterior muscles are dissected away from the ribs with electrocautery, in order to construct sufficient submuscular pockets, and submuscular tunnels to the hinge-points are created. 3) The bar (MX-bar system™, Medix Align Technology, Seoul, Korea) is passed across the mediastinum under the depressed sternum and then rotated 180 degrees in order to elevate the chest wall depression. 4) Both ends of the bar are placed between the ribs and serratus anterior muscles. 5) Both ends of the bar are firmly fixed in the submuscular pockets by suturing to muscles with PDS 1-0 (Fig. 1).
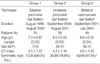
Patients undergoing the Nuss procedure were divided into three groups, depending on the bar fixation technique employed. Group 1 consisted of 25 patients, on whom the bilateral pericostal bar fixation technique was performed between August 1999 and August 2000. Group 2 consisted of 39 patients, on whom the pericostal bar fixation technique was performed on one side, and the submuscular technique was performed on the other between September 2000 and August 2001. Group 3 consisted of 49 patients, on whom the bilateral submuscular bar fixation technique without pericostal fixation was performed between September 2001 and July 2004 (Table 1). There were no significant differences between the groups with regard to age, sex ratio, and Haller CT index. However, the ratio of patients with symmetric-type pectus excavatum was significantly higher in Group 3 than in Group 1 (87.8% in Group 3 vs. 68% in Group 1, p=0.037).
To determind intergroup significances, one-way ANOVA and chi-square analysis with STATISTICA 6.0 (Statsoft Tulsa, OK, U.S.A.) were used. Significance limit was set at a p-value of <0.05.
All operations were completed as Nuss procedures, and in no cases did we convert to a Ravitch operation. The bars used in the Nuss procedures were 10.4±2.07 inches long in Group 1, 9.5±1.48 inches long in Group 2, and 10.1±1.71 inches long in Group 3 (p=0.34). A total of 10 patients (2 patients in Group 1, 6 in Group 2, and 2 in Group 3) required the stabilizer to be fixed to the edge of the bar unilaterally, and this occurred predominantly with the adult patients exhibiting asymmetric pectus excavatum. 2 patients in Group 1, and 1 patient in Group 2, all of whom exhibited broad and asymmetric pectus excavatum, required the installation of a second bar, which was fixed parallel to the main bar. The mean operation time for Group 1 was 67.2±33.07 min, 57.9±33.90 for Group 2, and 50.1±21.00 for Group 3. The mean operation time for Group 3 was significantly shorter than that recorded for Group 1 (p=0.041).
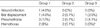
Bar dislodgement occurred in 4 patients (3.5%) in the total study subjects, and all of these patients suffered from asymmetric pectus excavatum. Reoperations for the relocation of the bar were performed in all patients exhibiting bar displacement. Pneumothorax developed in 7 of 113 patients (6.2%) and all of these patients were successfully treated via catheter-guided aspiration. No statistical significance with regard to bar dislodgement and pneumothorax was observed among the three groups. Hemothorax developed in 4 patients with asymmetric pectus excavatum (3.5%). All of these patients were treated successfully via thoracostomies. The incidence of hemothorax was significantly lower in Group 3 than in Group 1. In one patient with destructive lung, which was ascribed to pneumonia developed in the past, the bar was removed due to wound infection (Table 2). In univariate analysis, chest wall asymmetry was a significant risk factor for bar displacement (p=0.032), hemothorax (p=0.032), and pneumothorax (p=0.041).
After their operations, patients were transferred to the intensive care unit for one day, with no ventilator support. A patient-controlled anesthesia pump was utilized for the control of postoperative pain. All patients maintained a supine position during the period immediately after operation, a 45-degree semi-fowler position at 3.9±0.62 days postoperatively, a sitting position at 5.0±0.69 days, and ambulation at 6.1±0.55 days. The mean duration of hospital stay was 8.0±1.55 days.
Although early reports regarding the Nuss procedure documented difficulties with bar dislocation, often requiring reoperation (8), the popularity of this new technique has continued to increase.
Due to the possibility of bar dislocation in an otherwise well-tolerated and popular therapeutic modality, lateral stabilizers, which are attached to the pectus bar, have been developed in order to minimize the risk of this complication (8). Croitoru et al reported that bar shift before the use of stabilizers occurred at a rate of 15%, which decreased to 6% after stabilizers were placed, and then to 5% with the use of a wired stabilizer (9).
However, despite the use of a stabilizer, bar displacement has continued to be a significant problem with the Nuss procedure (4). Molik et al. discouraged the routine use of these stabilizers, since they were also quite conspicuous on the chest walls of younger patients (8). Likewise, the lateral bar is clearly visible in Miller's illustration (10).
The pericostal bar fixation technique is known to be successful in the prevention of bar dislodgement, and to cause a minimum of wound problems. Hebra et al. described the "third point of fixation", in which, under thoracoscopic visualization, a nonabsorbable suture is passed around the bar and around one rib on the anterior chest, to the right of the sternum (5). Schaarschmidt et al. reported the "submuscular bar, multiple pericostal bar fixation, bilateral thoracoscopy" (6) technique, which involves the positioning of the bar into a submuscular pocket located directly on the bony thorax, and then usually 4 to 6 heavy pericostal figure of 8 sutures are used to fix each bar on every side of the patient. Moreover, in this technique the end holes of the bar are also fixed, via the passing of pericostal figure of 8 sutures through the holes. Park et al. presented the "five-point fixation" method, in which steel wires encircle the rib above and the rib below at each end of the bar. Each wire passes through the end-hole of the bar, and a fifth wire is added on the right side at the hinge-point, which encircles both the bar and one rib (7). These multiple point pericostal bar fixation techniques are expected to prevent the bar from migrating in either a superior or inferior direction.
In our hospital, we performed bilateral pericostal bar fixations initially (Group 1), but eventually became concerned that this technique could increase the risk of both hemothorax and pneumothorax because of the possibility of lung or intercostal vessel injury during the large needle going through pleural space. Park et al. performing the Nuss procedure in 335 patients with the pericostal bar fixation reported the very low complication rate by the accumulation of experience and advancement of surgical technique (11). However, we thought that it would be more secure if the large needle did not penetrate the pleura. Therefore, we later began to attempt to position the bar in a submuscular pocket located directly on the bony thorax, with the overlying muscle being tightly enveloped by sutures on one side (group 2). This unilateral submuscular bar fixation technique was not associated with any higher incidence of bar dislodgement. Currently, however, (Group 3), we have been performing bilateral submuscular bar fixation the results of which are similar to those of Group 1 and 2 with regard to bar displacement. In addition, the incidence of hemothorax was significantly decreased, and the operation time was significantly reduced.
Schaarschmidt et al. purported that it is impossible to secure bars to chest wall muscles (6). However, if the ends of the bar were bent rather tightly, in order to cling to the rib, and the right-angle positioning of the bar was maintained, facing toward the peak of the sternal depression by the flipping of the bar either superiorly or inferiorly, submuscular fixation without pericostal fixation was sufficient for the prevention of bar displacement.
Because this study revealed that chest wall asymmetry was risk factor for postoperative complications, patients with asymmetry were hesitated to do the submuscular bar fixation in the Nuss procedure. Therefore, authors performed the Nuss procedure on patients with symmetric and mildly asymmetric pectus excavatum. Modified Ravitch operations (12) (minimal incision and pectus bar insertion) were performed on patients exhibiting moderate and severe asymmetric pectus excavatum, as well as adult patients. Currently, our institution has eschewed the use of any stabilizers or secondary bars in the repair of pectus excavatum. The Ravitch operation has evolved toward minimal invasiveness, an evolution which has resulted in more favorable morphological outcomes (13, 14). Therefore, it has become our policy to select either operation method, depending on the type of pectus excavatum being evidenced. Therefore, in the present study, the population of patients exhibiting symmetric chest wall deformities was higher (68% to 87.8%) than in other studies (7), which constitutes a major limitation of this study.
Despite this limitation, we were able to conclude that it is not, in fact, necessary to apply the pericostal fixation technique to all patients undergoing Nuss procedures. In patients with symmetric pectus excavatum, or young patients with mild asymmetric pectus excavatum, the submuscular bar fixation technique resulted in satisfactory outcomes, with regard to the prevention of bar displacement in the Nuss procedure. Additionally, the use of this technique, as opposed to the pericostal fixation technique, is strongly associated with a reduction in incidence of technique-related complications, including hemothorax and operation time.
Another limitation of this study is that patient grouping of this study was not randomized but followed the authors' experience chronologically. And, a longer follow-up study with a larger volume of patients would be necessary for the establishment of this method as an accepted part of the Nuss procedure.
Figures and Tables
References
1. Ravitch MM. Operative treatment of congenital deformities of the chest. Am J Surg. 1961. 101:588–597.

2. Nuss D, Kelly RE, Croitoru DP, Katz ME. A 10-year review of a minimally invasive technique for the correction of pectus excavatum. J Pediatr Surg. 1998. 33:545–552.

3. Hebra A, Swoveland B, Egbert M, Tagge EP, Geogeson K, Othersen HB Jr, Nuss D. Outcome analysis of minimally invasive repair of pectus excavatum; Review of 251 cases. J Pediatr Surg. 2000. 35:252–255.

4. Watanabe A, Watanabe T, Obama T, Ohsawa H, Mawatari T, Ichimiya Y, Abe T. The use of a lateral stabilizer increases the incidence of wound trouble following the Nuss procedure. Ann Thorac Surg. 2004. 77:296–300.

5. Hebra A, Gauderer MW, Tagge EP, Adamson WT, Othersen HB Jr. A simple technique for preventing bar displacement with the Nuss repair of pectus excavatum. J Pediatr Surg. 2001. 36:1266–1268.

6. Schaarschmidt K, Kolberg-Shwerdt A, Dimitrov G, Straus J. Submuscular bar, multiple pericostal bar fixation, bilateral thoracoscopy: a modified Nuss repair in adolescents. J Pediatr Surg. 2002. 37:1276–1280.

7. Park HJ, Lee SY, Lee CS, Youm W, Lee KR. The Nuss procedure for pectus excavatum: evolution of techniques and early results on 322 patients. Ann Thorac Surg. 2004. 77:289–295.

8. Molik KA, Engum S, Rescorla F, West KW, Scherer LR, Grosfeld JL. Pectus excavatum repair: experience with standard and minimally invasive techniques. J Pediatr Surg. 2001. 36:324–328.
9. Croitoru DP, Kelly RE, Goretsky MJ Jr, Lawson ML, Swoveland B, Nuss D. Experience and modification update for the minimally invasive Nuss technique for pectus excavatum repair in 303 patients. J Pediatr Surg. 2002. 37:437–445.

10. Miller KA, Woods RK, Sharp RJ, Gittes GK, Wade K, Ashcraft KW, Snyder CL, Andrews WM, Murphy JP, Holcomb GW 3rd. Minimally invasive repair of pectus excavatum: a single institution's experience. Surgery. 2001. 130:652–659.

11. Park HJ, Lee SY, Lee CS. Complications associated with the Nuss procedure: analysis of risk factors and suggested measures for prevention of complications. J Pediatr Surg. 2004. 39:391–395.

12. Jo WM, Choi YH, Sonh YS, Kim HJ, Hwang JJ, Cho SJ. Surgical treatment for pectus excavatum. J Korean Med Sci. 2003. 18:360–364.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download