Abstract
Endomyocardial biopsy (EMBx) is a useful tool for diagnosing various cardiac pathologies. However, the routine use of EMBx has not gained widespread acceptance due to the possible complications related to the EMBx. Thus, not much information is available on the complications related to the EMBx. We prospectively evaluated 90 consecutive patients who underwent 2-D echocardiography guided transfemoral right ventricular EMBx at Kyungpook National University Hospital between March 2002 and November 2005 to determine the incidence, nature and subsequent management of complications related to EMBx. The clinical diagnoses before the EMBx were arrhythmogenic right ventricular dysplasia in 54, dilated cardiomyopathy in 19, Brugada syndrome in 9, myocarditis in 6 and miscellaneous in 2 patients. The overall major complication rate was 5.6% and no procedure-related mortality occurred. Myocardial perforation (n=3), which was the most frequent complication, did not progress to cardiac tamponade requiring pericardiocentesis in any patient. Hemodynamically unstable ventricular tachycardia occurred in 1 patient. New and persistent right bundle branch block occurred in another. Our findings suggest that 2-D echocardiography guided transfemoral right ventricular EMBx is a relatively safe procedure.
Nowadays, both two-dimensional (2-D) echocardiography and fluoroscopy have become the preferred imaging modalities to guide endomyocardial biopsy (EMBx) (1-3). In contrast to traditional fluoroscopic guidance, 2-D echocardiography in addition to fluoroscopic guidance facilitates the direct control of the bioptome in the right ventricle, and therefore, reduces the risk of damage to the heart structures. Two-D echocardiography also permits one to detect a perforation at the moment of its occurrence and to manage the cardiac tamponade immediately.
Although 2-D echocardiography guided EMBx is useful for reducing the development of serious complications and their management, the routine use of EMBx in the diagnosis of diverse cardiac pathologies has not gained widespread acceptance in Korea due to the possible complications related to the procedure. Thus, not much information is available on the rate and kind of complications related to EMBx. In this study, we prospectively evaluated 90 consecutive patients who underwent 2-D echocardiography guided transfemoral right ventricular EMBx to determine the incidence, nature, and subsequent management of the complications related to the EMBx.
The study group consisted of 90 consecutive patients who underwent EMBx at Kyungpook National University Hospital between March 2002 and November 2005. A history, physical examination, routine laboratory studies, chest radiography, 12-lead ECG and 2-D echocardiography were performed on all patients. In selected cases, a Holter ECG, signal-averaged ECG, exercise-ECG, dobutamine echocardiography and cardiac MRI were also obtained. In a large number of patients, coronary angiography, cardiac catheterization, and ventricular tachycardia induction were also carried out simultaneously. Usually the EMBx was performed as the final diagnostic tool for confirming and making a differential diagnosis of various cardiac pathologies. The protocol of this study was approved by the ethics committee of the hospital and written informed consent was obtained from each patient.
Intravenous access was made through the right femoral vein as right heart catheterization and ventricular tachycardia induction were planned concomitantly during the EMBx. The right femoral vein was cannulated using the Seldinger technique. The puncture needle remained in the vein and a 0.032 inch guide wire was inserted through it. An 8 Fr Mullin sheath and dilator (Medtronic, Minneapolis, MN, U.S.A.) were then inserted over the wire. A 5.5 Fr 104 cm bioptome (Cordis, Miami, FL, U.S.A.) was inserted through the sheath. Two-D echocardiography was used to confirm the position of the bioptome in the right atrium and right ventricle. For ideal visualization of the instruments both in the right atrium and ventricle, an apical 4 chamber view, subcostal view, and parasternal short axis view were used. As it passed across the tricuspid valve, 2-D echocardiography was used to confirm that the direction of the bioptome was toward the right side of the interventricular septum. Two-D echocardiographic monitoring was carried out with a System Five® (GE Vingmed Ultrasound, Horten, Norway) with a 2.5 MHz probe. Once contact with the endocardium was confirmed by echocardiography, the bioptome was withdrawn 1 to 2 cm, its jaws were opened and advanced slowly to engage the endocardium. Gentle forward pressure was maintained while the jaws were closed. The bioptome containing the specimen was removed by gentle traction on the shaft. Two to 8 samples were obtained from each patient mainly from the right ventricular septum. However, in a small number of patients, the right ventricular outflow tract or right ventricular apex were biopsied to increase the sensitivity in cases of suspected arrhythmogenic right ventricular dysplasia (ARVD) or Brugada syndrome.
The major complications associated with the EMBx were divided to 4 categories (2, 4): complications related to venous cannulation, abnormalities of the heart rhythm, conduction abnormalities, and mechanical damage to the heart structures. Minor chest discomfort after the EMBx, although the relation was uncertain, was also evaluated.
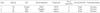
A total of 90 patients underwent EMBx from March 2002 to November 2005 (Table 1). They were 42±13 yr old and 60 were male. Their clinical diagnoses before the EMBx were ARVD (60.0%), dilated cardiomyopathy (21.1%), Brugada syndrome (10.0%), myocarditis (6.7%), hypertrophic cardiomyopathy (1.1%), and exercise-induced sustained ventricular tachycardia (1.1%) (Table 2). The right femoral vein was used in all cases. The number of specimens taken was 2 to 8 (mean: 4.6±1.4). The primary site of the EMBx was the right ventricular septum (93.3%). The right ventricular outflow tract was biopsied in 5 cases. In 1 case with dilated cardiomyopathy, a septal wall biopsy was technically difficult, so the right ventricular apex was mainly biopsied. Coronary angiography (96.7%) and ventricular tachycardia induction (68.9%) were carried out before the EMBx in the majority of the cases. The final EMBx reports were as follows; ARVD (32.2%), undetermined type cardiomyopathy (13.3%), dilated cardiomyopathy (8.9%), myocarditis (6.7%), fibrosis only (1.1%), and no diagnostic abnormality (37.8%).
Our overall major complication rate was 5.6% and no procedure related mortality was observed (Table 3). The most frequent complication was perforation (n=3), and it did not progress to cardiac tamponade requiring pericardiocentesis in any cases. Hemodynamically unstable sustained ventricular tachycardia requiring direct current cardioversion occurred in 1 patient. New and persistent right bundle branch block occurred in another. No complications related to the venous cannulation occurred in our series.
Hemodynamically unstable sustained ventricular tachycardia occurred in 1 patient. He was admitted to undergo an electrophysiological study and catheter ablation for paroxysmal supraventricular tachycardia. In the catheterization room, unexpected and recurrent ventricular fibrillations occurred several times during the insertion of the catheters and pacing. Two days after the successful catheter ablation of an atrioventricular reentrant tachycardia, ventricular tachycardia induction and an EMBx were performed in order to rule out any occult cardiomyopathy. After ventricular tachycardia induction and angiography were carried out, an EMBx was performed at the right ventricular septum. Hemodynamically unstable ventricular tachycardia developed during the second sampling and direct current cardioversion was applied to restore sinus rhythm. Two-D echocardiography showed no accumulation of pericardial effusion. No ventricular tachycardia or fibrillation recurred after the EMBx.
New and persistent right bundle branch block occurred just after the EMBx in 1 case. His clinical diagnosis was dilated cardiomyopathy and the ECGs recorded before and during the EMBx exhibited sinus tachycardia without bundle branch block. The EMBx specimens were obtained from near the apex, and no hemodynamic changes or chest pain occurred during the procedure. However, the ECGs recorded just after the procedure, revealed a right bundle branch block. His ECG did not progress to complete heart block and his general condition remained stable with no intervention.
Echocardiographic evidence of perforations was obtained in 3 subjects (Table 4). The ventricular tachycardia induction, coronary angiography, right heart catheterization, and right ventriculography were all performed before the EMBx. In the initial echocardiography just before the EMBx, there were no pericardial effusions. The pericardial effusions developed just after the EMBx, so we regarded them as perforations related to the EMBx. The right ventricular septum was the primary site for the EMBx in 2 of those patients. However, the EMBx was performed at the right ventricular outflow tract to increase the sensitivity of the EMBx in the other. The clinical diagnoses before the EMBx of those patients were ARVD (n=2) and Brugada syndrome (n=1). Two-D echocardiography revealed an accumulation of the pericardial effusion immediately after the procedure in all 3 cases. The effusions increased up to a maximum diameter of 6 mm with no significant hemodynamic changes. Close observation with hemodynamic monitoring was carried out and none of them progressed to a cardiac tamponade and the effusions resolved over several days.
Some abnormal symptoms or signs developed after the EMBx. Those abnormalities were nonspecific, transient, and may not have been related to the EMBx. Six patients (6.7%) complained of chest discomfort after the EMBx. The nature of the chest discomfort was both diverse and nonspecific. Although 2-D echocardiography during and after the EMBx did not show any accumulation of the pericardial effusion, we regarded the chest discomfort as a possible sign of a perforation and carried out a close observation. The atypical chest discomfort subsided spontaneously after several hours. However, acetaminophen was prescribed for relief of the chest discomfort in 1 case.
Two patients (2.2%) developed cold sweats, nausea, vomiting, and hypotension several hours after the EMBx. The laboratory studies, ECGs, and 2-D echocardiography revealed no significant abnormalities. In the first patient, sinus bradycardia (minimum heart rate 38 beats/min) was accompanied with hypotension. Projectile vomiting after food intake occurred before the hypotension and bradycardia, so we thought an increased vagal tone was the cause in that patient. Intravenous atropine and hydration with normal saline improved general condition. The second patient complained of hunger and cold sweats with the development of hypotension (minimum blood pressure 63/30 mmHg). However, she had maintained a fasting state for many hours before the EMBx and was tired with stress and insomnia. Intravenous hydration and oral feeding was used to restore her blood pressure and general condition. One patient developed nonsustained ventricular tachycardia a few hours after the EMBx and another complained of a severe headache during and after the EMBx. A neurological examination and brain imaging study including a brain CT and MRI revealed no abnormalities and his symptoms were relieved with analgesics. A transient fever developed in another case with no abnormal findings in the routine studies. The fever subsided without any medication.
Although the histological and biochemical analyses of the heart tissue obtained by an EMBx is the most likely technique to advance our understanding of various myocarditis and cardiomyopathies (5-7), some serious complications that might endanger one's life also have long been noted (4, 8). In fact, some believe that an EMBx may not be the appropriate diagnostic strategy in unknown cardiomyopathy due to the associated risks of major complications such as ventricular wall perforation (9). However, there are some patients whose diagnoses remain unclear even after extensive noninvasive evaluations and we may need histologic confirmation to make a proper diagnosis, differential diagnosis and risk stratification of the patients (5). This study was from a single center and all the EMBx procedures were unrelated to heart transplantations, thus, we believe that our results may reflect the real situation of the complications related to EMBx procedures.
Four categories of complications might occur in association with an EMBx (2, 4). The first includes complications related to venous cannulation. Over half of the complications such as an incidental arterial puncture, bleeding, hematoma, vasovagal reaction, or rarely, a pneumothorax when the internal jugular approach is used may occur during the venous cannulation (3, 5, 10). When compared with the internal jugular vein, the femoral venous approach has the risk of a deep vein thrombosis and subsequent pulmonary embolism due to the use of longer sheaths and the required immobilization after the procedure (11). However, we did not experience any serious complications in our series. We also could cannulate femoral vein with no difficulty in all cases probably due to the relatively large diameter of the femoral vein.
The second category is comprised of abnormalities of the heart rhythm. The heart rhythms in patients with a prior history of arrhythmias were reported to have a tendency to be exacerbated by endocardial irritation induced by the bioptome (2, 4, 12, 13). Supraventricular tachycardia has been known to be most frequently observed arrhythmia during EMBx (4). However, the development of ventricular tachycardia was also reported (4, 5). In our series, 1 patient developed sustained ventricular tachycardia during the EMBx. Even though he had only a history of documented paroxysmal supraventricular tachycardia, ventricular fibrillation was repeatedly induced during the electrophysiologic study and sustained ventricular tachycardia developed during the EMBx. The arrhythmogenic irritation caused by the bioptome under a high sympathetic tone may have been the cause of these arrhythmias in this young man. We think that having a history of certain types of arrhythmias does not guarantee that only the same type of arrhythmia will occur during the EMBx and the operator must be prepared to manage any kind of arrhythmia during the EMBx.
The third category is comprised of conduction abnormalities. Rarely, right bundle branch block may be created or complete heart block may result in patients with a preexisting left bundle branch block because the conduction system in the right ventricular septum may be damaged by the bioptome during the EMBx (4, 12, 14). Most conduction abnormalities related to the EMBx procedure are known to be transient and without any significant hemodynamic consequences. One case of asymptomatic and persistent right bundle branch block developed after the EMBx in this study. Although most conduction abnormalities have a benign course, the operator must be prepared for the abrupt development of complete heart block in the case of a preexisting left bundle branch block.
The fourth category of complications includes mechanical damage to the heart structures such as injury to the tricuspid valve and perforation of the heart or central veins. Right ventricular pseudoaneurysms (15), coronary artery to right ventricular fistulas (16), and atrioventricular fistulas (17) have also been reported. Several reports have described the development of tricuspid regurgitation after an EMBx in heart transplant recipients (18-21). In heart transplant recipients, the EMBx is usually performed repeatedly for the early detection of a graft rejection and the number of EMBx procedures is known to be directly related to the occurrence of significant tricuspid regurgitation, especially if the EMBx is performed under fluoroscopic guidance only (2, 18, 20). No significant tricuspid regurgitation was observed in our series since EMBx was performed only once and under the guidance with both fluoroscopy and 2-D echocardiography. We paid great care to avoid any damage to the tricuspid valve by the bioptome manipulation. Even the sheath was inserted slowly over the wire to pass the tricuspid valve while the dilator was somewhat withdrawn into the sheath to reduce the possibility of tricuspid valve damage by the pointed tip of dilator. In some cases, we also shaped the sheath into a more suitable form to pass across the tricuspid valve without any damage to valvular structure. We think that 2-D echocardiography was especially useful in guiding the passage of the sheath across the tricuspid valve without any damage to the valvular and subvalvular structures.
Right ventricular free wall perforations and resultant pericardial effusion, tamponade or death remain the most concerning complications of EMBx procedures (1-4, 13). In the survey of 1,591 biopsies, of which 445 were done solely with echocardiographic guidance, Ragni et al. reported only 2 cases of right ventricular perforations (0.13%) with both occurring during fluoroscopic guidance (1), which suggests the improved safety of 2-D echocardiography guided EMBx to conventional fluoroscopy-guided EMBx. In our series, 3 out of 90 patients developed pericardial effusions, however, none progressed to cardiac tamponade or death. The interventricular septum has been known to be the safest part of the right ventricle for an EMBx, however, it is also known to usually be spared from any fibro-fatty replacement associated with ARVD (6). Therefore, we selected to use the right ventricular outflow tract and right ventricular apex for the biopsy site in some cases to improve the diagnostic sensitivity in such cases. One of those 5 patients in whom the EMBx was performed from the right ventricular outflow tract developed pericardial effusion. However, perforations also occurred when the EMBx was performed mainly from the right ventricular septum (n=2). Although the perforations occurred only in patients with ARVD (n=2) or Brugada syndrome (n=1), we think that the biopsy site was more important than the disease entity in order to predict a perforation for a few reasons. First, our study group was mainly composed of patients with suspected ARVD or Brugada syndrome, and therefore perforations occurred mainly in those 2 groups. Secondly, the EMBx was intentionally performed from the right ventricular outflow tract and right ventricular apex, where the risk of perforation is known to be higher than that of the septum, in order to increase the diagnostic sensitivity. Two perforations, in which the septum was the primary site for the biopsy, might be related to the other possible technical causes such as taking an EMBx from the septal-free wall junction, excessive push applied to the bioptome, or too large size of a sample removed (1, 10). The number of cases presented in this study may not have been large enough to assess the risk of perforation according to the type of cardiac pathology. A larger series comparing the risk of perforations among diverse cardiac pathologies may be required. Although complete prevention of perforations was not feasible, we could easily detect the perforations as accumulating pericardial effusions in the early stages by 2-D echocardiography. Two-D echocardiography was also useful for close monitoring of the pericardial effusions.
Several minor abnormalities also occurred after the EMBx procedures. In our experience, most of those symptoms and signs were transient without any sequelae. However, great care must be paid to those minor abnormalities to determine whether or not they are truly insignificant abnormalities or omens of grave complications.
Figures and Tables
ACKNOWLEDGEMENTS
We thank Mr. John Martin and Dr. SungHee Kim for their assistance with the preparation of this manuscript.
References
1. Ragni T, Martinelli L, Goggi C, Speziali G, Rinaldi M, Roda G, Pederzolli C, Intili PA, Raisaro A, Vigano M. Echo-controlled endomyocardial biopsy. J Heart Transplant. 1990. 9:538–542.
2. Bedanova H, Necas J, Petrikovits E, Pokorny P, Kovalova S, Malik P, Ondrasek J, Cerny J. Echo-guided endomyocardial biopsy in heart transplant recipients. Transpl Int. 2004. 17:622–625.

3. Drury JH, Labovitz AJ, Miller LW. Echocardiographic guidance for endomyocardial biopsy. Echocardiography. 1997. 14:469–474.

4. Deckers JW, Hare JM, Baughman KL. Complications of transvenous right ventricular endomyocardial biopsy in adult patients with cardiomyopathy: a seven-year survey of 546 consecutive diagnostic procedures in a tertiary referral center. J Am Coll Cardiol. 1992. 19:43–47.

5. Ardehali H, Qasim A, Cappola T, Howard D, Hruban R, Hare JM, Baughman KL, Kasper EK. Endomyocardial biopsy plays a role in diagnosing patients with unexplained cardiomyopathy. Am Heart J. 2004. 147:919–923.

6. Angelini A, Thiene G, Boffa GM, Calliari I, Daliento L, Valente M, Chioin R, Nava A, Volta SD. Endomyocardial biopsy in right ventricular cardiomyopathy. Int J Cardiol. 1993. 40:273–282.

7. Fast JH, Kubat K, van Haelst UJGM, Schuurmans Stekhoven JH. The usefulness of an endomyocardial biopsy in heart disease of unknown etiology. Int J Cardiol. 1986. 11:317–328.

8. Mason JW. Techniques for right and left ventricular endomyocardial biopsy. Am J Cardiol. 1978. 41:887–892.

9. Wu LA, Lapeyre AC 3rd, Cooper LT. Current role of endomyocardial biopsy in the management of dilated cardiomyopathy and myocarditis. Mayo Clin Proc. 2001. 76:1030–1038.

10. Anderson JL, Marshall HW. The femoral venous approach to endomyocardial biopsy: comparison with internal jugular and transarterial approach. Am J Cardiol. 1984. 53:833–837.
11. Vorlat A, Conraads VM, Vrints CJ. Deep vein thrombosis after transfemoral endomyocardial biopsy in cardiac transplant recipients. J Heart Lung Transplant. 2003. 22:1063–1064.

12. Talwar KK, Varma S, Chopra P, Wasir HS. Endomyocardial biopsy-technical aspects experience and current status. An Indian perspective. Int J Cardiol. 1994. 43:327–334.
14. Ali N, Ferrans VJ, Roberts WC, Massumi RA. Clinical evaluation of transvenous catheter technique for endomyocardial biopsy. Chest. 1973. 63:399–402.

15. Rodrigues AC, de Vylder A, Wellens F, Bartunek J, De Bruyne B. Right ventricular pseudoaneurysm as a complication of endomyocardial biopsy after heart transplantation. Chest. 1995. 107:566–567.

16. Henzlova MJ, Nath H, Bucy RP, Bourge RC, Kirklin JK, Rogers WJ. Coronary artery to right ventricle fistula in heart transplant recipients: a complication of endomyocardial biopsy. J Am Coll Cardiol. 1989. 14:258–261.

17. Katta S, Akosah K, Stambler B, Salter D, Guerraty A, Mohanty PK. Atrioventricular fistula: an unusual complication of endomyocardial biopsy in a heart transplant recipient. J Am Soc Echocardiogr. 1994. 7:405–409.

18. Tucker PA 2nd, Jin BS, Gaos CM, Radovancevic B, Frazier OH, Wilansky S. Flail tricuspid leaflet after multiple biopsies following orthotopic heart transplantation: echocardiographic and hemodynamic correlation. J Heart Lung Transplant. 1994. 13:466–472.
19. Braverman AC, Coplen SE, Mudge GH, Lee RT. Ruptured chordae tendineae of the tricuspid valve as a complication of endomyocardial biopsy in heart transplant patients. Am J Cardiol. 1990. 66:111–113.





 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download