Abstract
Unilateral thoracic sympathectomy in patients with palmar hyperhidrosis causes a skin temperature drop in the contralateral hand. A cross-inhibitory effect by the post-ganglionic neurons innervating hands is postulated as a mechanism of contralateral vasoconstriction. The purpose of our study was to evaluate whether this cross-inhibitory effect also occurs in the feet. Twenty patients scheduled for thoracoscopic sympathicotomy due to palmar hyperhidosis were studied. Right T3 sympathicotomy was performed first, followed by left T3 sympathicotomy. The thenar skin temperatures of both hands and feet were continuously monitored using a thermometer and recorded before induction of anesthesia, during the operation, 4 hr after and 1 week later. Following right T3 sympathicotomy, the skin temperature of the ipsilateral hand gradually increased, however the skin temperature of the contralateral hand gradually decreased. Immediately after bilateral sympathicotomy, the skin temperature differences between hands and feet increased, but these differences decreased 1 week later. Our results show that cross-inhibitory control may exist in feet as well as in the contralateral hand. Thus, the release of cross-inhibitory control following T3 sympathicotomy results in vasoconstriction and decrease of skin temperature on the contralateral hand and feet. One week later, however, the temperature balance on hands and feet recovers.
Primary palmar hyperhidrosis is usually managed by sympathectomy, which removes the upper thoracic sympathetic ganglia controlling sweating of the upper extremities (1). Among various surgical modalities, video-assisted thoracoscopic sympathicotomy has evolved into an effective treatment for severe hyperhidrosis of the upper limbs due to its high immediate and permanent success rate and low morbidity (2, 3).
As it is impossible to obtain histologic diagnosis during sympathicotomy, an increase in skin temperature due to vasodilatation following sectioning of the sympathetic chain is used to confirm successful sympathicotomy (4). Intraoperative monitoring of palmar skin temperature was found to be very important in locating and confirming the correct sympathetic segment for laser ablation (4, 5). Moreover, physiologic confirmation was believed to be more reliable than histologic verification (5). Wu et al. (6) found an interesting fact. Following thoracic ganglionectomy, unilateral palmar temperature was found to increase, whereas contralateral finger surface temperature decreased. These results suggested the existence of a cross-inhibitory effect by the post-ganglionic neurons innervating blood vessels of the upper extremities and a release of this effect after ganglionectomy, resulting in contralateral vasoconstriction and decrease of palmar temperature (6). To our knowledge, however, there is little information on skin temperature changes of the upper and lower extremities after thoracic sympathicotomy.
We therefore evaluated changes in the skin temperature of both hands and feet during and after thoracic sympathicotomy, to determine whether this cross-inhibitory effect occurs in the feet as well as in the contralateral hand.
We studied 20 patients (13 men, 7 women) scheduled for endoscopic transthoracic sympathicotomy due to palmar hyperhidosis. All patients were free of any cardiovascular disease. Patients ages ranged from 13 to 38 yr (mean 21.6±6.8 yr), their mean weight was 58.2±9.9 kg, and their mean height was 166.0±7.8 cm. All patients gave informed consent to participate in the study, and the study was approved by the local ethical committee of the hospital.
No medication was administered on the day of surgery. The operating room was maintained at a temperature of 25℃ with an air-conditioning system. Blood pressure, cardiac rhythm, and oxygen saturation (SpO2) were monitored during the operation. Core temperature using esophageal stethoscope with temperature sensor (DeRoyal Inc., Powell, TN, U.S.A.) was recorded after induction of anesthesia, before right side sympathicotomy, after left side sympathicotomy, and before extubation of double-lumen tube. The thenar skin temperatures of both hands and feet were continuously monitored using a thermometer (Hewlett Packard Co., Palo Alto, CA, U.S.A.). Anesthesia was induced by intravenous infusion of propofol (2 mg/kg), fentanyl (0.15 µg/kg), and vecuronium (0.15 mg/kg). The trachea was intubated using a 35-Fr or a 37-Fr left double-lumen tube (Broncho cath®, Mallinckrodt, Dublin, Ireland). Anesthesia was maintained with continuous intravenous infusion of propofol (8-12 mg/kg/hr). Incremental doses of fentanyl and vecuronium were given as required. Estimated fluid losses were replaced by intravenous infusion of warmed Hartmann solution. The legs and the arms were wrapped to prevent heat radiation.
Surgery was performed on patients in the standard 30° head-up position. A straight thoracoscopy (Richard Wolf GmbH, Knittlingen, Germany) was inserted between the 2nd and 3rd rib in the right anterior axillary line and connected to a computer compact disc camera video system (Video Processor, Sony Co., Tokyo, Japan). The T3 ganglion was identified and coagulated completely with a unipolar diathermy probe. The same procedure was repeated on the left side. Single lung ventilation was performed for wider vision. At the end of surgery on each side, PEEP up to 35 cm H2O was applied for 10 sec concomitant with the evacuation of intrapleural air and CO2 via a 12-Fr catheter. Chest radiography was performed in the recovery room of the one-day surgery center to check for the presence of intrapleural air or fluid.
Skin temperatures were recorded before induction of anesthesia, at baseline (i.e. before right side sympathicotomy), 2 min, 4 min, 6 min, and 10 min after right side sympathicotomy, 10 min after left side sympathicotomy, 4 hr after surgery, and at follow up 1 week later.
All data are expressed as mean±SD. Data were analyzed using the statistical software SigmaStat™ (version 2.03, SPSS Inc., Chicago, IL, U.S.A.). Multiple comparisons (Tukey test) of the repeated measured analysis of variance (ANOVA) were used to analyze differences in thenar skin temperatures at each time. p values <0.05 were considered statistically significant.
Esophageal temperature after induction of anesthesia, before right side sympathicotomy, after left side sympathicotomy, and before extubation of double-lumen tube were 36.1±0.4℃, 35.9±0.4℃, 35.9±0.4℃, and 35.8±0.5℃, respectively. These showed no significant differences.
Thenar skin temperatures of both hand and feet during and after thoracoscopic T3 sympathicotomy are summarized in Table 1.
After the induction of anesthesia, the skin temperature of both hands and feet increased significantly. Following coagulation of the right T3 ganglia, the skin temperature of the ipsilateral hand gradually increased, beginning at 2 min after right side sympathicotomy and becoming statistically significant at 4 min, 6 min, and 10 min (1.5±1.2℃, 2.1±1.9℃, and 2.7±2.0℃, respectively, p<0.05 each). Beginning at 2 min, the skin temperature of the contralateral hand gradually decreased, becoming statistically significant at 10 min (-0.7±0.9℃, p<0.05). Ten minutes after coagulation of the left T3 ganglia, the skin temperatures of both hands increased significantly (2.1±1.9℃ on the left hand, 3.3±2.4℃ on the right hand, p<0.05 each).
The skin temperatures of both feet did not change during right T3 sympathicotomy but the skin temperature of the left foot decreased slightly at 6 min and 10 min (-0.1±1.0℃ and -0.2±1.0℃, respectively, p>0.05), although these changes were not significant. Ten minutes after left T3 sympathicotomy, the skin temperatures of both feet decreased significantly (-1.3±0.8℃ on the left foot, -1.2±0.8℃ on the right foot, p<0.05 each).
Four hours after the operation, the skin temperatures of both hands had increased significantly (4.6±2.2℃ for the left hand, 4.9±2.5℃ for the right hand, p<0.05 each), whereas the skin temperatures of both feet decreased significantly (-3.1±2.0℃ for the left foot, -3.4±1.9℃ for the right foot, p<0.05 each) (Fig. 1).
The skin temperature differences between hands and feet decreased after induction of anesthesia and increased postoperatively, but had disappeared 1 week later (Fig. 2).
We have shown here that the skin temperature of the ipsilateral hand gradually increased, whereas the skin temperature of the contralateral hand gradually decreased, following coagulation of right T3 ganglia. In contrast, the skin temperature of both hands increased and the skin temperature of both feet decreased after bilateral T3 sympathicotomy. These alterations in skin temperature, however, were no longer present 1 week after surgery.
Although primary hyperhidrosis is not life-threatening, the excessive sweating that accompanies this embarrassing disorder is the dominant indication for sympathetic surgery (1). Recently, the results of thoracoscopic sympathectomy limited to the resection of the T3 ganglion were similar to those following conventional thoracoscopic resection of the 1st through the 4th thoracic sympathetic ganglia (7, 8). As the severity of compensatory hyperhidrosis can be correlated with the number of ablated or resected ganglia (9), video-assisted thoracoscopic sympathicotomy limited to the T3 ganglion is usually performed in our hospital. Our selective T3 sympathicotomy has a success rate of nearly 100% and a moderate compensatory hyperhidrosis rate of less than 10%.
The mechanisms underlying the thenar skin temperature drop on the contralateral hand after right T3 sympathicotomy and the skin temperature reduction on feet after bilateral T3 sympathicotomy are not clear. Many factors and physiologic mechanisms are related to temperature regulation. Thermoregulatory sweating remarkably increases cutaneous heat loss. In this study, however, the patients' hands and feet did not sweat while they were under general anesthesia. Thus, the skin temperature reduction on the contralateral hand after unilateral sympathicotomy is not related to heat loss through increased sweat excretion. In addition, we prevented heat loss of the body during anesthesia and surgery with warmed fluid, wrapped extremities, and well maintained room temperature. Measured esophageal temperature proved that core temperature was constant during the surgery. So, the possibility of heat loss during anesthesia and thus a fall in temperature were excluded.
Thermoregulation is the central neural integration of body temperature. There are as many thermoregulatory integrators as thermoregulatory responses, including sweating, vasoconstriction, and shivering. Furthermore, these integrators are represented at many levels of the nervous system, with each level facilitated or inhibited by levels above and below (10). The purpose of such a complicated arrangement is to achieve fine control over body temperature. The sympathetic system is responsible for maintaining vasomotor homeostasis and mediating changes in the microcirculation (11), and excessive sympathetic (presumably vasoconstrictor) outflow to the skin may reduce sensory axon-reflex responses (12). Patients with palmar hyperhidrosis have been reported to have a much more complex dysfunction of autonomic nervous system, involving compensatory high parasympathetic activity as well as sympathetic overactivity (13, 14), suggesting that sympathicotomy initially induces a sympathovagal imbalance with a parasympathetic predominance, and that this is restored on a long-term basis (14). Therefore, thoracic sympathicotomy may cause a temporary impairment of the caudal-to-rostral hierarchy of thermoregulatory control and changes in microcirculation. The reduction of finger skin temperature on the non-denervated side may be due to either a decrease in the cross-inhibitory effect or the abnormal control of the inhibitory fibers by the sudomotor center (6). Vasoconstrictor neurons have been found to be largely under the inhibitory control of various afferent input systems from the body surface, whereas sudomotor neurons are predominantly under excitatory control (15). The basic neuronal network for this reciprocal organization is probably located in the spinal level (15). Therefore, the reduction in the contralateral skin temperature may be explained by cross-inhibitory control of various afferent in the spinal cord.
In particular, our study showed that, following bilateral T3 sympathicotomy, the skin temperatures on the hands increased whereas the skin temperatures on the feet decreased. These findings suggest a cross-inhibitory control between the upper and lower extremities. However, the pattern of skin temperature reduction on the feet differed from that on the contralateral hand. The skin temperature on the feet did not decrease after right T3 sympathicotomy but decreased significantly after bilateral T3 sympathicotomy. This finding may have been caused by the vasodilatory effect of propofol (16). Although propofol was used as a general anesthetic in all our patients due to relatively low vasodilatory capacity (17), the vasodilatory effect of propofol on peripheral blood flow may attenuate the vasoconstrictive effect caused by the loss of cross inhibitory control between the upper and lower extremities. The cross-inhibitory control of the contralateral hand is likely to be stronger than that between the upper and lower extremities, in as much as the skin temperature on the contralateral hand decreased significantly during propofol anesthesia. If the release of cross inhibitory control was involved in the drop of temperature on the feet, the temperature of the feet should have decreased below the preanesthetic level after the operation. The latter was not observed, however, possibly because patients with hyperhidrosis already have an overactive sympathetic nervous system, thus preventing further vasoconstriction. In addition, the skin of the feet is thicker than that of the hands making it less sensitive to slight changes of temperature. Furthermore, the release of the cross-inhibitory mechanism could have been weaker 4 hr after the operation. Because the temperature difference between the hands and feet decreased 1 week later, unknown homeostatic mechanisms of the body may have regulated the temperature balance of the whole body.
The autonomic nervous system is a complex system, in which post-ganglionic neurons at any level in the spinal cord can modulate activities reciprocally. Thus, our results may not be explained in full by a simple mechanism of cross-inhibitory control in the spinal cord. However, the existence of cross-inhibitory control between the upper and lower extremities may explain one of the mechanisms of compensatory hyperhidrosis, which is a matter of concern during the treatment of palmar hyperhidrosis. After sympathectomy in patients with palmar hyperhidrosis, increased sweating on another body surface may be caused by increased sympathetic activities due to the loss of cross-inhibitory control between the upper extremities and another body surface. Thus, additional studies and a greater understanding of cross-inhibitory control may provide further clues to the etiology of compensatory hyperhidrosis.
In conclusion, our results suggest that cross-inhibitory control by various afferents in the spinal cord may exist in the feet as well as in the contralateral hand. The release of cross-inhibitory control by T3 sympathicotomy results in vasoconstriction and a decrease of skin temperature on the contralateral hand and the feet. Homeostatic mechanisms, however, may restore the temperature balance of the body.
Figures and Tables
Fig. 1
(A) Time course of skin temperature difference of hands compared with baseline value during and after T3 sympathicotomy. The skin temperature of the contralateral (left) hand decreases significantly after right T3 sympathicotomy but increases as much as that of the right hand after bilateral T3 sympathicotomy. (B) Time course of skin temperature difference of feet compared with baseline value during and after T3 sympathicotomy. The skin temperature of the feet dose not change after right T3 sympathicotomy but decreases significantly after bilateral T3 sympathicotomy. Pre: before induction of anesthesia, Baseline: before sympathicotomy, 2, 4, 6, and 10: 2, 4, 6, and 10 min after right T3 sympathicotomy, respectively, Lt 10: 10 min after left T3 sympathicotomy, OSC; 4 hr after the operation in the one-day surgery center, Follow up: 1 week after the operation. *: p<0.05 compared with baseline value, †: p<0.05 compared with right side value, ‡: p<0.05 compared with OSC value.

Fig. 2
Time course of skin temperature difference between hands and feet compared with preinduction value during and after T3 sympathicotomy. The skin temperature difference on both sides are reduced significantly after induction of anesthesia but increase after sympathicotomy on each side, becoming maximal 4 hr after the operation but decreasing significantly 1 week later. Pre: before induction of anesthesia, Baseline: before sympathicotomy, 2, 4, 6, and 10: 2, 4, 6, and 10 min after right T3 sympathicotomy, respectively, Lt 10: 10 min after left T3 sympathicotomy, OSC; 4 hr after the operation in the one-day surgery center, Follow up: 1 week after the operation. *: p<0.05 compared with Pre value, †: p<0.05 compared with OSC value.

Table 1
Thenar skin temperature (℃) of both hands and feet during and after video assisted thoracoscopic T3 sympathicotomy
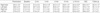
Baseline: before sympathicotomy; 2 min, 4 min, 6 min, 10 min: 2, 4, 6, 10 min after right T3 sympathicotomy respectively; Lt 10 min: 10 min after left T3 sympathicotomy; OSC; 4 hr after the operation in the one-day surgery center; Follow up: 1 week after the operation.
*, p<0.05 compared with baseline value.
References
1. Doolabh N, Horswell S, Williams M, Huber L, Prince S, Meyer DM, Mack MJ. Thoracoscopic sympathectomy for hyperhidrosis: indications and results. Ann Thorac Surg. 2004. 77:410–414.

2. Dumont P, Denoyer A, Robin P. Long-term results of thoracoscopic sympathectomy for hyperhidrosis. Ann Thorac Surg. 2004. 78:1801–1807.

3. Chuang KS, Liu JC. Long-term assessment of percutaneous stereotactic thermocoagulation of upper thoracic ganglionectomy and sympathectomy for palmar and craniofacial hyperhidrosis in 1742 cases. Neurosurgery. 2002. 51:963–970.

4. Lu K, Liang CL, Lee TC, Chen HJ, Su TM, Liliang PC. Changes of bilateral palmar skin temperature in transthoracic endoscopic T-2 sympathectomy. J Neurosurg. 2000. 92:44–49.

5. Kao MC, Tsai JC, Lai DM, Hsiao YY, Lee YS, Chiu MJ. Autonomic activities in hyperhidrosis patients before, during, and after endoscopic laser sympathectomy. Neurosurgery. 1994. 34:262–268.

6. Wu JJ, Hsu CC, Liao SY, Liu JC, Shih CJ. Contralateral temperature changes of the finger surface during video endoscopic sympathectomy for palmar hyperhidrosis. J Auton Nerv Syst. 1996. 59:98–102.

7. Yoon SH, Rim DC. The selective T3 sympathicotomy in patients with essential palmar hyperhidrosis. Acta Neurochir (Wien). 2003. 145:467–471.

8. Bonjer HJ, Hamming JF, du Bois NAJJ, van Urk H. Advantages of limited thoracoscopic sympathectomy. Surg Endosc. 1996. 10:721–723.

9. Hsia JY, Chen CY, Hsu CP, Shai SE, Yang SS. Outpatient thoracoscopic limited sympathectomy for hyperhidrosis palmaris. Ann Thorac Surg. 1999. 67:258–259.

10. Satinoff E. Neural organization and evolution of thermal regulation in mammals. Science. 1978. 201:16–22.

11. Holzer P. Morris JL, Gibbins IL, editors. Control of the cutaneous vascular system by afferent neurons. The Autonomic Nervous System. Autonomic Innervation of the Skin. 1997. Vol 12. Amsterdam: Harwood Academic;213–267.
12. Hornyak ME, Naver HK, Rydenhag B, Wallin BG. Sympathetic activity influences the vascular axon reflex in the skin. Acta Physiol Scand. 1990. 139:77–84.

13. Kaya D, Karaca S, Barutcu I, Esen AM, Kulac M, Esen O. Heart rate variability in patients with essential hyperhidrosis: dynamic influence of sympathetic and parasympathetic maneuvers. Ann Noninvasive Electrocardiol. 2005. 10:1–6.

14. Wiklund U, Koskinen LO, Niklasson U, Bjerle P, Elfversson J. Endoscopic transthoracic sympathicotomy affects the autonomic modulation of heart rate in patients with palmar hyperhidrosis. Acta Neurochir (Wien). 2000. 142:691–696.

15. Janig W, Kummel H. Organization of the sympathetic innervation supplying the hairless skin of the cat's paw. J Auton Nerv Syst. 1981. 3:215–230.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download